

Case Reports - Year 2000 - Volume 15 -
Extreme Case of Survival in Severely Burnt Patient - Case Report
Caso Extremo de Sobrevida em Paciente Grande Queimado - Relato de Caso
ABSTRACT
The authors present the case of a patient that had survived to massive thermal injury corresponding to 92% of his body surface (Lund-Browder Diagram) with second- and third-degree burns. The report discusses the importance of the correct hydration prescription, hypnoanalgesia during strict asepsy and disinfection of burnt area, as well as nutritional and antibiotic therapy to be preseribed to patients under these conditions. Comments are made also to the effective participation of the surgical team with timely tangential debridement and grafting on the deepest regions even with searce donor area.
Keywords: Burns; severely burnt patient; nutrition; hypnoanalgesia; hypertonic solution
RESUMO
Os autores apresentam o caso de um paciente que sobreviveu a lesão térmica maciça ocupando uma área correspondente a 92% de sua superfície corporal (Diagrama de Lund-Browder), com queimaduras de segundo e terceiro graus. Neste relato discutimos a importância da correta prescrição da hidratação, da hipnoanalgesia durante a rigorosa assepsia e degermação da área queimada, bem como a nutrição e a antibioticoterapia que devem ser prescritas a um paciente nessas condições. Tecemos também comentários à determinante participação da equipe cirúrgica, com desbridamentos tangenciais sempre oportunos e enxertia das regiões mais profundas, mesmo com a escassez de área doadora.
Palavras-chave: Queimaduras; grande queimado; nutrição; hipnoanalgesia; solução hipertônica
Burns are among the most severe injuries that body may withstand, not only for excruciating pain, but also for the possibility of hypovolemic and septic shock proportional to the extension and depth of the affected area. Survival rate of a patient victim of thermal trauma has not been statistically well documented in Brazil, where a trend to overvalue burnt area is observed. This fact is imputed to lack of information and non-utilization of the international criteria (Lund-Browder Diagram). In a study published in the Journal of the International Society of Burns with 3499 patients with ages ranging from 3 weeks to 90 years, interned in seven different hospitais in India, there was no report of survival of patients having more than 70% of burnt body surface. There was no survival with even more than 30% of burnt area. On the other end, the National Information Exchange on Burns Statistics in the USA - 1985, shows that the survival of an adult having 85% of body surface burnt ranged from 0% to 5%.
The reported case is about a 25-year old male patient that survived massive thermal trauma affecting 92% of body surface. Factors that possibly affected survival are described, which included a combination of immediate volemic replacement with aggressive surgical approach of daily dressings, nutritional support, prompt sepsis treatment and, basically, the dedication of multidisciplinary team comprised of intensive care clinicians, plastic surgeons, specialized nursing, nutritionists and psychologists. These factors seem to be the key for success in the treatment of severely burnt patient.
CASE REPORT
M.S.S., 25 year-old white male patient, presenting 92% burnt body surface (BBS) distributed as follows: 74% superficial second-degree, 13% deep second-degree and 5% third degree (Fig. 1).
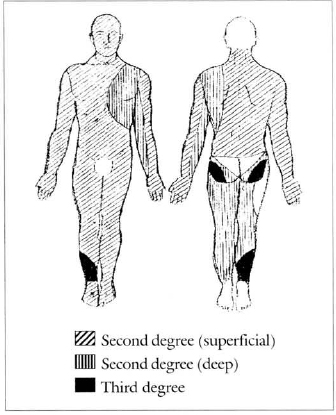
Fig. 1 - Burnt area diagram.
Burn was caused by direct flame, caused by explosion of an empty alcohol tank when the patient lighted a blowtorch to weld it. Interestingly, thirddegree deeper injuries affected lower limbs, once this region was that with major contact with fire while the patient got away fromn the accident area.
As the patient was in a semiclosed environment at the time of explosion (within the tank), smoke inhalation or airway burns by overheated vapor was suspected.
PROMPT TREATMENT
Patient was admitted to Hospital Geral do Andaraí's CTQ at 1:20 p.m. (2 hours and 20 minutes after accident), and presented himself lucid, oriented, and cooperative, with 112 pbm heart rate. He had clean lungs, 26 irpm no-effort respiratory rate, which temporarily excluded the likelihood of inhalation once the accident occurred within the tank. Previously healthy, the patient denied associated pathologies and did not present any other type of trauma at phvsical examination.
Right at the start, he was resuscitated with crystalloid solution (Ringer Lactate) at sufficient rate to maintain urinary output between 30 to 50 ml/hour. After vesical catheter introduction, the patient was referred to balneotherapy where, after endovenous analgesia with narcotic (Meperidine), he had burnt area washes with running water, disinfection with polyvinylpyrrolidone-iodine (PVPT), friction and phlyctena breakdown, followed by topical application of 1% silver sulphadiazine in addition to containment dressing and immunization against tetanus. The following examinations were requested on admission: complete blood count, biochemistry, blood typing, Rh factor and thorax radiograph.
Fluid diet, according to acceptance and gastric mucous membrane protection with 50 mg of intravenous Ranitidine every 8 hours were prescribed since the first moment. Bed head was maintained at 30° and burnt limbs also were kept raised.
FIRST 24 HOURS
During the first 5 hours, 3,000 ml Ringer Lactate were instilled intravenously. At 7:00 p.m., Ringer was temporarily replaced by 1.5% hypertonic solution, administered by the same route during one hour, summing up 500 ml. At that moment (20 hours), Ringer infusion was restarted, summing up 1.500 ml more within the next 8 hours. From then on (4 hours), venous hydration was changed again to a 7.5% hypertonic solution with the administration of 100 ml within 20 minutes, due to a slow and progressive diuresis from 80 ml/h ar 20 hours to 28/m1/h. Ringer Lactate (more than 1,000 ml) was retaken and maintained till the end of the first 24-hour hospitalization.
At the end of first day, hydric volume offered was 4,750 ml orally and 6,100 ml intravenously, summing up 10,850 ml for a diuresis corresponding to 1,136 ml, which equals to 47 ml/h urinary output on average.
BETWEEN 24-AND 48-HOUR TREATMENT
On the second day at CTQ, fluid diet according to acceptance (total of 4,450 ml) and venous hydration with Ringer Lactate (1,000 ml), were maintained, as well as gastric protection with 50 mg of Ranitidine intravenously every 8 hours, and human plasma replacement was initiated with a total of 600 ml/day.
DRESSING
Balneotherapy was the daily procedure adopted throughout the hospitalization period. It consisted of abundant injury washing with running water, at Morgani's table, withdrawal of devitalized tissue, use of polyvinylpyrrolidone disinfection (PVPI) solution, followed by application of a large 1% silver sulphadiazine layer, and occlusion with gauze and crepon.
Analgesic scheme routinely used at CTQ (Midazolan 0.1 ml/kg + Cetamine 1 mg/kg), besides helping with the task, allowed us to approach the burnt area always on a timely basis and offering early tangential debridements from the 5th day of hospitalization, which allowed maintenance of bacterial colonization of burnt area under control.
During hospitalization, some areas, initially thought as being superficial second degree, were observed to have deepened and required early surgical intervention. Burn depth delimitation was achieved in the 5th day of hospitalization only.
HEMODYNAMIC CHANGES
On biochemical examination, patient presented hypoproteinemia throughout practically the initial thirty days after injury, so colloid solution with human plasma (600 ml/day) and albumin (150 ml/ day) up to 38th day of burning were associated to treatment. A total of 15 units of erythrocyte concentrate were administered during the first 30 days, indicated by the microhematocrit criteria routinely performed at the service.
Around 10,000 ml of plasma and 4,200 ml albumin, equivalent to sixty-seven 150-ml bags and eighty-four 50-ml bottles, respectively, were administered.
INFECTION
On third day of hospitalization, patient evolved with sustained hyperthermia (38.6°C), tachycardia (144 bpm), tachypnea (38 irpm), oliguria (28 ml/h) , generalized edema, slow capillary filling and respiratory tract with no changes. Infection was suspected and then, after blood sample collection for blood count and hemoculture, antibiotic therapy with firs-tgeneration cephalosporin (Cefalotine 2g IV, each 6 hours) was started, associated to an aminoglucoside (Amicacine 500 mg IV, each 12 hours).
On 9th day at CTQ, five days after first antibiotic association, patient remained stable under clinical view, but his conditions were bad due to burnt area extension. He remained feverish and blood count showed leukocytosis with important left deviation. Thus, Cephalotine was substituted for Imipenen (1g, each 6 hours) that remained associated to aminoglucoside for nine days.
He remained stable until the 17th day when a new sepsis clinical picture was initiated, which determined aminoglucoside replacement for vancomicyn (500 mg, each 6 hours). On the 20th day at CTQ, the patient remained under bad conditions and Imipenen was replaced with a third generation cephalosporin (cephtadizime 1 g, each 8 hours) that started actuating together with vancomicyn.
On the 36th day, vancomicyn + cephtadizime association was undone with the second being used as monotherapy up to the 39th day of hospitalization.
During self-grafting surgery to recover the already granulated area in the pre, per and immediate postoperative period, first generation cephalosporin was employed following CDC's recommended rule.
Antibiotics were maintained ar changed according to clinical and laboratory picture of infection.
NUTRITIONAL SUPPORT
Oral diet, on the first 24 hours, was freed according to the patient's acceptance. A routine antiemetic (metachlopramide) was prescribed. The patient accepted 4,750 ml on the first 24 hours.
On the 4th day, when patient was hemodynamically stable, enteral nutritional support (EN5) was initiated using Curreri's formula(2) as basis for total caloric value (TCV). Diet followed the 100:1 calorie/nitrogen ratio due to the need for maintaining a nitrogen balance in face of the burnt patient's large consumption according to Kagan et col. (5) suggestions.
Two hand-made diets are available for enteral use in the service: Q1 (1,000 kcal into 1,000 ml) and Q2 (2,000 kcal into 1,000 ml).
We started with 1,000 ml Q1 by infusion pump for 24 hours, associated to 2,000 kcal and 125 g oral protein, according to patient's tolerance. Ranitidine was suspended after enteral started as this is sufficient to protect gastric mucous membrane(4). Soon on the following day (5th day at CTQ), oral diet was increased to 2,500 kcal plus 150 g proteins and Ql was passed to 1,500 ml daily.
On the 14th day, oral diet was changed to 3,500 kcal plus 200 g daily proteins and enteral to Q2 with 1,200 ml/day.
On the l.6th day, Q2 enteral diet was increased to 1,500 ml/day.
On the 19th day, Q2 enteral diet was increased to 1,800 ml daily.
Enteral was increased on the 22nd day, reaching 7,000 kcal daily divided into 3,000 kcal orally (plus additional 250 mg protein) and 2,000 ml Q2 by enteral, due to calorie satisfactory acceptance. This diet was maintained up to the 27th day when proteins were reduced to 210 g daily.
Enreral diet was suspended on the 28th day and only oral diet was maintained.
From the 41st day, oral diet was reduced to 2,900 kcal plus 250 g protein until dismissal.
VENOUS ACCESS
The search for deep venous access in non-burnt area of a patient who had only 8% of healthy body surface, represented one of the major challenges faced along the treatment. On the 10th day of hospitalization, right femoral vein dissection and puncuture were carried out.
On the 17th, left femoral vein dissection was carried out.
During a great deal of the hospitalization period, venous access route was the peripheral one.
SURGERIES
Surgical approach offered to patient consisted of several surgical debridement times and a self-grafting time (mesh graft) performed on a timely basis characterized by those moments in which the patient presented hemodynamic stability, infection control and area aspect indicated for debridement.
Most of these procedures were performed during daily balneotherapy, benefited by analgesic scheme adopted for the case. Other larger procedures were performed at the hospital's operating room due to the need for a greater analgesia time for a more aggressive debridement.
RESULTS
The good results obtained with treatment are due to surgical clinical approach. Factors likely to have influenced survival were immediate volemic replacement combined with surgical aggressive approach of daily dressings, under effective analgesia, summed up to nutritional support with high caloric and protein rates, in addition to sepsis aggressive treatment.
Patient was dismissed from hospital on 05/13/1998, after 72-day hospitalization, deambulating, with renal function preserved, with no burnt area exposed and with no functional seguelae.
DISCUSSION
HEMODYNAMIC CHANGES
Burn comprises one of the major aggressions that organism may withstand. Loss of liguid for interstice as a function of capillary permeability increase in extensive burns causes the burn shock that provokes the need for aggressive and immediate volemic replacement to which we successfully arrived employing 1.5% and 7.5% hypertonic solution. The intensity of fluid loss is direct1y related to injury depth. During hospitalization, the patient presented low output episodes accompanied by lower limb and scrotal sac edema.
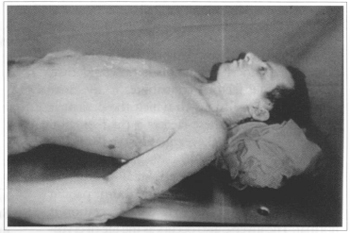
Fig. 2 - Balneotherapy in severely burnt parient.

Fig. 3 - Balneotherapy in severely burnt parient.
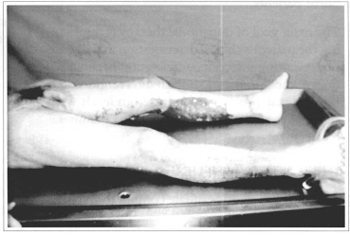
Fig. 4 - Area to be grafted at lower limb.
Finding extremely pale burnt patients with low hematocrit counts is very common.
A slight hemolysis upon thermal trauma occurs depending on the burn degree and injured area extension. Hemolysis goes unnoticed and hardly surpasses 10% of original hematocrit due to intensive fluid flow for interstice on burnt and non-burnt tissue and resulting hemo-concentration. The patient's initial hematocrit was 58.5% falling to 29.4% within 5 days.
After establishing hemodynamic balance, an important hematocrit reduction is observed that, added to other factors, contributes to the multiple blood transfusions to which the patient is submitted. One of these factors is the reduction of erythrocyte normal average lifetime from 120 days to approximately 40 days. This reduction arises out of erythrocyte peripheral destruction once if we transfuse blood from a burnt patient to a normal one, erythrocyte life expectation is normal. The inverse also occurs as the life of erythrocytes transfused to the burnt patient is reduced by the same process(5).
NUTRITIONAL SUPPORT
Burns constitute a difficult problem for nutritional therapy. Weight loss, negative nitrogen balance, neurohormonal changes imposed by a marked catabolism characterize post-thermal injury metabolic response with magnitude of these changes being related to injury extension and depth(6).
The marked increase of skeletal musculature proteolysis, together with lipolysis and gluconeogenesis, characterizes severely burnt patient metabolic changes that will determine a fast protein-caloric undernourishment process.
The nutritiona1 support revolutionized the burnt patient treatment in the last ten years and this was direct1y reflected on the survival of severely burnt patients.
The main goal of nutritional therapy is minimizing the patient's clinical deterioration in the sense of preventing infection, accelerating healing, reducing the number of surgical interventions and hospital stay time(7). Albumin serum levels were strict1y kept around 3 g by oral and parenteral rep1acement.
INFECTIOUS PICTURE
After thermal injury, exudate coming from burnt area constitutes an excellent culture media for the bacterial development and its proliferation. Intravascular clotting located at burnt area will prevent the immunologic system inflammatory mediator arrival as well as will prevent that antibiotics administered by parenteral route reach therapeutic levels on injured tissues. In addition, an important immunosupression occurs that is proportional to burn extension(8).
CONCLUSION
Successful treatment of patients with massive thermal trauma depends above all on a well coordinated, trained and 24-hour vigilant multidisciplinary team.
REFERENCES
1. DAVIES JWL. The problem of burns in India. Burns. 1990; Suppl. 1:S1-24.
2. CUNNINGHAM MKL, HEGARTY MT, MEARA PA, BURKE JF. Measured and predict calorie requirements of adults during recovery from severe burn trauma. Am. J. Clin. Nutr.1989;49:404-8.
3. KAGAN RJ. Restoring nitrogen balance after burn injury. Compr. Ther. 1991;17:60-7.
4. GOMES DR, SERRA MC et al. Alterações metabólicas e suporte nutricional no Grande Queimado. Ver. Bras. Terap. Intens. 1990;2:27-31.
5. ARTZ CP. Epidemiologia, causas e prognóstico. Queimaduras. Saunders Company, 1980. p. 14-19.
6. DINGELDEIN Jr. GP, HUGGINS BM. Nutritional support in thermal injury. SALISBURY RE, NEWMAN NM, DILGENDEIN Jr. GP. Manual of burn therapeutics. Boston, Little Brown. 1983;61-80.
7. DEMLING RH. Burns. N. Engl. J. Med. 1985;313:1389-98.
8. DEICH EA. Infection in the compromised host. Surg. Clin. North. Am. 1988;68:187-97.
I - Clinical Coordinator of Centro de Tratamento de Queimados of Hospital do Andaraí. Assistant Professor of Postgraduation Course in Plastic Surgery of PUC- Rio and Instituto de Pós-Graduacão Médica Carlos Chagas.
II - Pediatric Coordinator of Centro de Tratamento de Queimados do Hospital do Andaraí. Head of Pediatrics at Hospital Municipal Souza Aguiar. Assistant professor of Postgraduation Course in Plastic Surgery at PUC- Rio.
III - Plastic Surgeon. Head of Centro de Tratamento de Queimados of Hospital do Andaraí.
IV - Postgraduation student of Plastic Surgery at PUC-Rio (Professor Ivo Pitanguy's Service)
V - Probationer of Centro de Tratamento de Queimados do Andaraí.
Address for correspondence:
Dino Roberto Gomes, MD
R. Ataulpho Coutinho, 80 bl. 1 ap. 704
22793-090 - Rio de Janeiro - RJ Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter