

Articles - Year 2000 - Volume 15 -
Clinical Applications of the Antebrachial Flap in the Reconstructive Microsurgery
Aplicações Clínicas do Retalho Antebraquial na Microcirurgia Reconstrutiva
ABSTRACT
The antebrachial flap is extremely versatile. It has been used as a premolded or single free flap cutaneous island. Although this is a bigger matter for surgeons than to the patients, the major problem is the donator area. This work addresses its clinical applications at a series of 48 patients who received indications for the head and neck reconstruction, penis reconstruction or in the reconstructive microsurgery of the extremities, in which the innervated flaps where necessary, such as the thumb, hands and inferior limbs reconstruction.
Keywords: Reconstruction; microsurgery; antebrachial flap
RESUMO
O Retalho Radial Antebraquial é extremamente versátil. Tem sido utilizado como ilha cutânea, retalho livre simples ou pré-moldado. O grande problema tem sido sua área doadora; isto, no entanto, é um problema maior para os cirurgiões do que para os pacientes. Este trabalho discute suas aplicações clínicas numa série de 48 pacientes que tiveram indicações para reconstrução de cabeça e pescoço, reconstrução de pênis ou na cirurgia reconstrutiva das extremidades, em que retalhos inervados foram necessários; como na reconstrução do polegar, da mão ou dos membros inferiores.
Palavras-chave: Reconstrução; microcirurgia; retalho antebraquial
In 1978, doctors Yang Guo Fang, Chen Baogui and Gao Yuzhi(8)of the Shenyang Military General Hospital, described the Antebrachial Flap based on the radial artery(8); initially used as a Free Flap and latter used in Pediculate Island. In the last decade Fouche, Biemer and Stock(5), widely used it in severe traumas of the superior limb.
Besides having a big cutaneous territory, the antebrachial radial flap is very versatile and can be programmed according to the necessities(1)(premanufactured, premolded, as a composed flap with the tendons, muscles, bones, and/or vascularized nerves).
The purpose of this work is a retrospective analysis of the antebrachial radial flap used by the Reconstructive Microsurgery Group of Ribeirão Preto, from April 1994 to June 1998.
CASUISTIC AND METHOD
From April 1994 to June 1998, 48 flaps where performed in 48 patients; where 40 were males and 8 were females. The surgical interventions where performed by the Reconstructive Microsurgery group at the hospitais where they where required (HC - FMUSP; Hospital São Lucas; Santa Casa and Instituto Santa Lydia, in Ribeirão Preto).
The Flap design is variable, according to the size and location to be reconstructed. The Allen Test was performed in all the patients, and the Doppler and Digital Arteriography were associated to five of them due to the trauma severity. The dissection is initiated at the proximal extremity of the Flap, the Radial artery is localized between the brachioradial muscle and the radial flexor muscle of the wrist(3); after that, the cephalic vein is prepared until the cubital fossa, where the antebrachial lateral cutaneous nerve, responsible for the cutaneous island sensibility, was also isolated. An incision at the Flap's ulnar rim until the muscular fascia is further performed; this fascia is sutured to the dermis with 5-0 nylon; the dissection is performed until the lateral rim, the superficial flexor muscle of fingers, is reached. The radial rim dissection is performed until the medial extremity of the brachioradial tendon is reached, where the release of the vascular pedicle is performed; after that, the progressive dissection of the Flap is performed with a careful hemostasia of the several muscle branches(7).
In order to decrease the area, sutures with nylon 4-0 are performed at the defect edges of the donator area. The brachioradial muscle and the radial flexor muscle of the wrist are proximally put together; the paratenon is careful preserved at the forearm distal segment in order to allow the good integration of the cutaneous graft, which is sutured with 5-0 nylon to the wound edges. A Brown bandage is placed at the grafted area and is removed seven days after the surgery.
RESULTS
The radial artery sacrifice did not lead to any ischemic complication of the superior limb(9). Good results were obtained from 42 of thc 48 operated patients. The majority of the complications are related to the inferior limb traumas, which are always attributed to the PTVD (Post-traumatic Vascular Disease) that occurs very frequently in these patients(4).
The surgery follow up varied from 4 to 48 months. A delay of the donator area cicatrization is due to a partial lost of the cutaneous graft occurred in 3 case. The 3 patients were treated in a conservative way and the tendon expositions or important functional sequelae were not noted. Figures 1 to 6 show some of the obtained results.
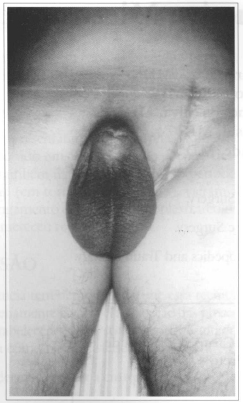
Fig. 1a - Complete amputation of the penis.
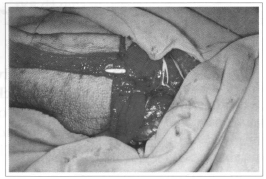
Fig. 1b - Neurovascular pedicle dissection.
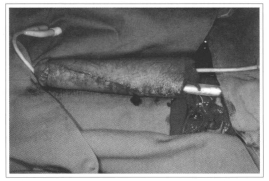
Fig. 1c - After the prosthesis introduction.
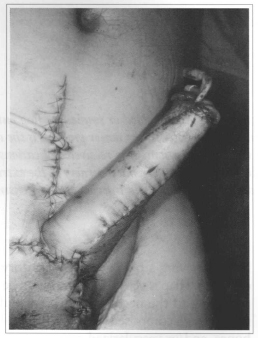
Fig. 1d - Immediate postoperative.

Fig. 1e - Physiological functions after 6 months.
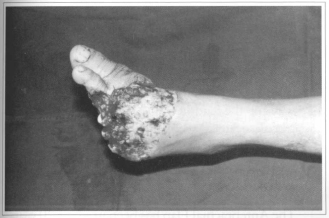
Fig. 2a - Foor partial amputation.
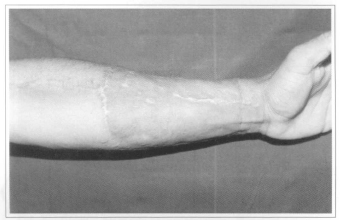
Fig. 2b - Donator area.
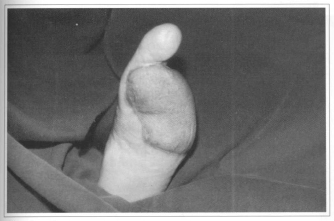
Fig. 2c - 3 years postoperative.
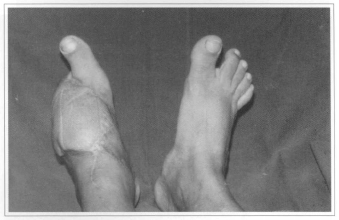
Fig. 2d - Reinnervated free flap - 36 months.
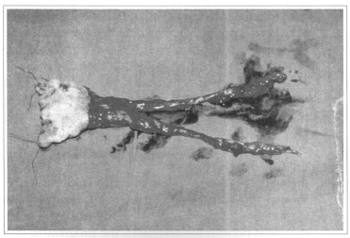
Fig. 3a - Pre-molded antebrachial flap for nasal reconstruction (preoperative).
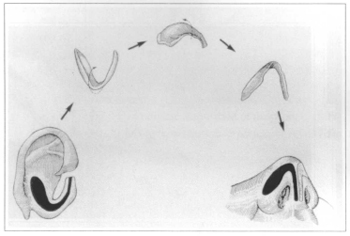
Fig. 3b - Reconstruction of the alar cartilage in a single block (Dr. Max Pereira Technique).
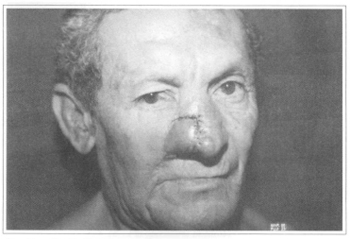
Fig. 3c - Profile Detail.
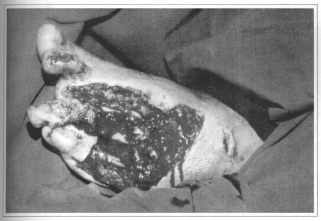
Fig.4a - Complex trauma of the inferior limb.
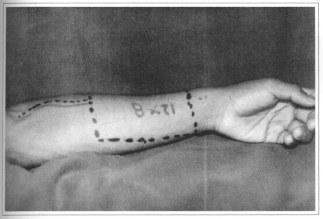
Fig.4b - Flap planning.

Fig. 4c - 3 years postoperative.

Fig. 5a - Fracture III b of the superior limb.

Fig. 5b - Flap prepared for vascular anastomosis.
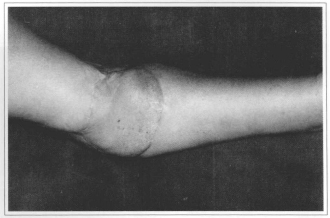
Fig. 5c - 4 years postoperative.
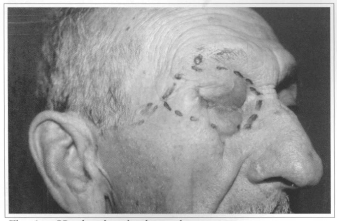
Fig. 6a - Head and neck advanced tumor.

Fig. 6b - CT: destruction of the right orbitary wall.
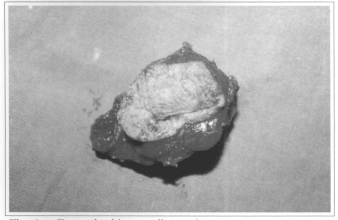
Fig. 6c - Eye and orbitary wall resection.
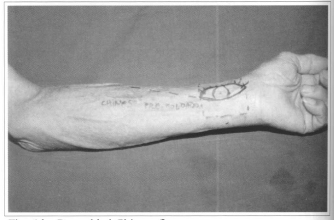
Fig. 6d - Premolded Chinese flap.
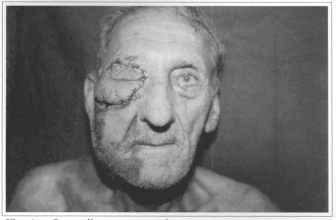
Fig. 6e - Immediate postoperative.
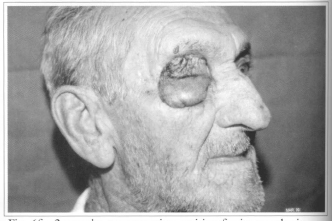
Fig. 6f - 3 months postoperative, waiting for its prosthesis.
DISCUSSION
The Antebrachial Flap has been used for 20 years(3,4) and it has been shown to be effective and safe in the reconstructive microsurgery. As time passes by, new techniques were developed allowing the everimproving functional and esthetic results.
The wide acceptance of the Antebrachial Microsurgical Flap is due to the fact that, besides its anatomy is more constant than the other flaps, it allows several technical variations to the surgeon(3).
Regarding this flap, the sear at the donator area is of big concern to the surgeons. At this revision of this young group of surgeons, it became clear that the scar has annoyed more the physicians than the patients.
It is the authors experience that the Antebrachial Flap has been shown as an efficient and safe method for the head and neck reconstrucrion, as well as for the penis reconstrucrion and/or extremities reconstructive surgery when there is an indication of innervated flaps(2).
CONCLUSION
The Antebrachial Flap has been used for 20 years and it has been shown to be effective and safe in the reconstructive microsurgery. Its wide acceptance is due to the fact that, besides its vascular anatomy is more constant than the other flaps, it allows several technical variarions to the surgeon(5,6,10). It is the authors experience that the scar at the donator area of the Antebrachial Flap has annoyed more the surgeons than the patients and that, together with the musculus rectus abdominis flap and the fibula, it is still one of the three big weapons in the Reconstructive Microsurgery.
REFERENCES
1. BESTEIRO JM. Comunicação pessoal. In: XXXIV CONGRESSO BRASILEIRO DE CIRURGIA PLÁSTICA. 1997, São Paulo.
2. BUNCKE HJ. Microsurgery transplantation replantation: an atlas text. Lea Feibenger, 1993. p. 687-97.
3. CHEM RC. Introdução à microcirurgia reconstrutiva. Rio de Janeiro : Medsi, 1993. p. 3-4.
4. FERREIRA MC. Transferência de retalhos livres com microcirurgia vascular. São Paulo : Faculdade de Medicina Universidade de São Paulo, 1978 (Tese de Livre Docência).
5. FOUCHER F, GENETCHEN N, MERLE M, MICHON J. Single staged thumb reconstruction by a composite forearm island flap; Br. J. Plast. Surg. 1984,37:139-48.
6. LAZO DAA, COLICCHIO O, CHAIN RG. O retalho antebraquial inervado na reconstrução do membro superior. In: XXXIII CONGRESSO BRASILEIRO DE CIRURGIA PLÁSTICA. 1995, Brasília.
7. O'BRIEN B, MORRISON WA. Reconstructive microsurgery. Edinburgh : Churchill Livingstone, 1987. p. 341-50.
8. SONG R, GAO Y, YU Y, SONG Y. The forearm flap. Clin. Plast. Surg. 1982;9:21-26.
9. TIMMONS MJ. The vascular basis of the radial forearm flap. Plast. Reconstr. Surg. 1986;77:80-91.
10. UPTON J, HAVLIK RJ, KHOURI RK. Refinements in hand coverage with microvascular free flaps. Clin. Plast. Surg. 1992;19:841-57.
I - Titular Member of the Brazilian Society of Plastic Surgery.
II - Associate Member of the Brazilian Society of Plastic Surgery.
III - Associate Member of the Brazilian Society of Orthopedics and Traumatology.
Address for correspondence:
Serviço de Microcirurgia e Cirurgia Plástica de Ribeirão Preto
Av. 9 de Julho, 1818 14020-170 - Ribeirão Preto - SP Brazil
Phone: (55 16) 636-8356 Fax: (55 16) 620-0297


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter