

Articles - Year 2002 - Volume 17 -
The Open Palm Technique in Severe Dupuytren's Contracture
Utilização da Técnica da Palma Aberta nas Contraturas Graves de Dupuytren
ABSTRACT
This paper aims to study the authors' experience with the open palm technique originally described by McCash for the treatment of severe Dupuytren's contractures. All patients presented hand ulnar border (ring and little fingers) impairment and belonged to stages III to IV of the classification proposed by Tubiana. In a period of 6 years, 35 patients were submitted to regional fasciectomy. On average, 18 days were necessary (extremes of 15 and 25) to complete scar healing. We obtained an average articular residual deficit of 25° to the ring finger and 30° to the little finger at the proximal interphalangeal articulation level.
Keywords: Dupuytren; McCash; open palm
RESUMO
Este estudo tem como objetivo demonstrar a experiência dos autores com a técnica da palma aberta descrita originalmente por McCash para o tratamento das contraturas graves de Dupuytren. A totalidade dos pacientes apresentava acometimento da borda ulnar da mão (anular e mínimo) e pertenciam aos estágios III e IV da classificação proposta por Tubiana. Em um período de 6 anos, 35 pacientes foram submetidos à fasciectomia regional. Foram necessários 18 dias, em média (extremos 15 e 25), para completar a cicatrização cutânea. Obteve-se um déficit residual articular médio de 25º ao dedo anular e 30º ao dedo mínimo, sempre ao nível da articulação interfalangiana proximal.
Palavras-chave: Dupuytren; Mc Cash; palma aberta
The etiology and treatment of Dupuytren's disease remain controversial(1-6). When preparing the therapeutic plan, it is important to determine the stage of disease. Much has been investigated on surgical techniques, since surgery was considered the only really effective method to control the condition(7-11). Intraoperative technical difficulties and postoperative complications are directly related to the stage of disease. The incidence of hematoma, skin necrosis, infection and relapse substantially increase in severe cases of Dupuytren's disease. The need for larger dissection, skin devitalization and excessive suture tension are factors that predispose to such complications. In the open palm technigue originally described by McCash(12), a regional fasciectomy is performed to allow for finger extension, which results in a large skin defect. The wound is left open to heal by second intention, thus avoiding tension and hematoma, which would decrease the incidence of necrasis, infection, and the possibility of relapse.
The objective of this paper is to report our experience with the open palm technigue in severe contractures of Dupuytren's disease, evidencing its advantages and disadvantages.
MATERIAL AND METHOD
In the period from January 1994 to December 1999, 35 patients, including 30 bilateral patients, with clinical diagnosis of Dupuytren's disease and important functional deficit were submitted to palmar fasciectomy.
Patients' average age was 60 years old (ranging from 48 to 75). Average follow-up postoperative was 48 months and minimum follow-up was 24 months. Five patients presented impairment in the little finger only. None of the patients had been submitted to previous surgery for Dupuytren's Disease. Evolution time ranged from four to eight years (average of six years) (Table I).
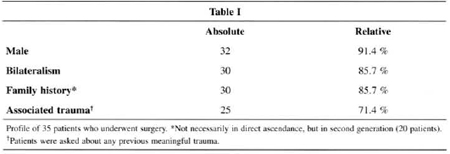
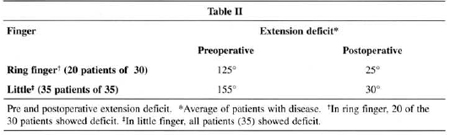
We followed the classification advocated by Tubiana et al.(13), in which the sum of the extension deficits of metacarpal-phalangeal articulations (MP), the proximal interphalangeal joint (PIJ) and the distal interphalangeal joint (DIJ), measured at a digital goniometer, are divided into four stages: stage I: 0-45°, stage II: 46-90°, stage III: 91-135° and stage IV: > 135°. We only included in this study patients classified in degrees III and IV Ring finger average was 125°, all fingers presenting values between 110° and 130°, Tubiana stage III. Little finger average was 155°, ranging from 145° to 165°, Tubiana stage IV.
The surgical technigue used in all patients was that advocated by McCash(12), with digital elongation through a Brunner's incision. Postoperative care was limited to changing dressings weekly, except that the vaseline bandage placed on the exposed area was not removed until total skin healing (Figs. 1 to 6). A volar plastered splint in the intrinsic plus position (wrist in flexion of 30°, MP in flexion of 70° to 90°, PIJ and DIJ at 0° of extension) was maintained for 15 days, and total digital movement freedom was permitted after this period. All patients were submitted to Weber's test (static sensitive discrimination of two points) in the sixth postoperative month.

Fig. 1 - Contracture in ring and little fingers, left: hand.

Fig. 2 - Transoperative period, showing loss of skin substance using the open palm technique, complete finger extension.

Fig. 3 - Five days, postoperative.

Fig. 4 - Ten days, postoperative.

Fig. 5 - Fifteen days, postoperative.

Fig. 6 - Complete scar healing, small extension deficit of little finger.
RESULTS
Open palm technique results in the cases classified as Tubiana's degree III and IV(l3) were considered satisfactory. No cases of cutaneous suffering and infection were recorded. The residual extension deficit, evaluated at 6 months, in 20 of the 30 patients with impairment at the ring finger, was 25°(average) (Figs.7, 8 and 9). All patients presented deficit in the little finger, with an average of 30°, always at the PIJ articulation level. Thirteen patients referred to pain during effort for a postoperarive period of four months.

Fig. 7 - Contracture in ring and little fingers.

Fig. 8 - Loss of substance and full extension during transoperarive period.

Fig. 9 - Full extension, with minor deficit of little finger.
Weber's test in the postoperarive period showed 14 patients with alterations in sensitivity immediately after surgery. Weber's test score remained lower than for the same contralateral finger after surgery for five out of the 14 patients (Table II).
Complete scar healing at the exposed palmar area occurred in 18 days on average (range: 15 and 25). An average of sixty days was needed for patients to resume independent manual activity. By December 2001, no relapses were recorded.
DISCUSSION
Surgical management of Dupuytren's disease began by performing the relaxation of the contracted fascia (Dupuytren, 1834), and since then several techniques and modifications have been described: fasciectomy (Fergusson, 1846), dermofasciectomy with a skin graft (Lexer, 1931), regional fasciectomy (Hamlin, 1952 and Hueston, 1962), radical fasciectomy (McIndoe, 1958), open palm technique (McCash, 1964), fasciectomy with skin preservarion (Skoog, 1967), limited fasciectomy (Colville, 1968), segmental aponeurectomy (Moermans, 1986), percutaneous fasciectomy (Bryan, 1988).
There are controversies in the literarure on the advantages and disadvantages of open palm techniques. It is suggested that the open palm technique determines large skin elongation, in addition to preventing complications such as hematoma (8,9,14-18). The disadvantage is that there is a higher risk of infection and patient discomfort owing to the "open" lesion. In this series, there were no cases of infection and none of the patients complained of having a healing wound in the palm of the hand. A comparative study between both techniques concluded that patients operated on by techniques in which the palm was completely closed developed a higher residual contracture(15).
Complication and relapse rates vary hugely, regardless of the technique employed (4,7,14,17,19). Relapse rates in the literature range from 28%(19) to 50%(13,20). None of the parients in this series have had relapses to date. We believe this results from the average postoperative follow-up of 48 months and also because we did not have any young patients, 60 year-old average (ranges between 48 and 75).
Results obtained from using the open palm technique were sarisfactory, considering the severity of digital contracture in the preoperative period. These results are evidenced both by the low incidence of complications and by residual extension deficit (30°). We believe the McCash technique is an excellent alternative for severe cases of Dupuytren's disease (stages III and IV).
REFERENCES
1. Badalamente M, Hurst L, Sampson SP. Prostaglandins influence myofibroblast contractility in Dupuytren's disease. J Hand Surg [Am]. 1988; 13:867-71.
2. Barros F, Barros A, Almeida S. Enfermidade de Dupuytren: Avaliação de 100 casos. Ver Bras Ortop. 1997; 32:177-83.
3. Luch JV Dupuytren's contracture. A new concept of the pathogenesis correlated with surgical management.J Bone Surg [Am]. 1959; 41:635-64.
4. McGouther DA. La maladie de Dupuytren, to incise or excise? J Hand Surg [Br] J. 1988; 13:368- 70.
5. Murrel GA, Francis MJ, Brornley L. Free radicals and Dupuytren's contracture. Br Med J. 1987; 295:1373-5.
6. Skoog T Dupuytren's contracture: pathogenesis and surgical treatment. Surg Clin North Am.1967; 47:433-44.
7. Bryan AS, Ghorbal MS. Long term result of closed palmar fasciotomy in the management of Dupuytren's contracture. J Hand Surg [Br]. 1988; 13:254-7.
8. Freitas AD, Pardini AG, Neder AT Contratura de Dupuytren: tratamento pela técnica da palma aberta. Ver Bras Ortop. 1997; 32:301-4.
9. Gonzales RI. Open fasciectomy and full-thickness skin graft in the correction of digital flexion deformity. In: Green. Operative hand surgery.Edinburgh. Livingstone ed. 1974. p.123-7.
10. Moraes GPN, Chambriard C, Osório L et al.Fascioctomia percutânea na correlação da deformidade da articulação metacarpofalângica na contratura de Dupuytren. Ver Bras Ortop. 1996; 31:347-50.
11. Harnlin JRE. Limited excision of Dupuytren's contracture. Ann Surg. 1952; 135:94-7.
12. McCash CR. The open palm technique in Dupuytren's contracture. Br J Plast Surg. 1964; 17:271-80.
13. Tubiana R, Fahrer M, McCullough MA. Recurrence and other complications in surgery of Dupuytren's contracture. Clin Plast Surg. 1981; 8:45-9.
14. Hueston JT. Digital Wolfe grafts in recurrent Dupuytren's contracture. Plast Reconstr Surg. 1962; 29:342-4.
15. Lubahn JD, Lister GD, Wolfe T. Fasciotomy and Dupuytren's disease: a comparison between the open palm and wound closure. J Hand Surg [Am].1984; 9:53-8.
16. Malta MC, Vianna SE, Wolfe T. A técnica da palma aberta na contratura de Dupuytren, Rev Bras Ortop. 1984; 19:46-8.
17. Tonkin MA, Burke FD, Varian JPW Dupuytren's contracture: a comparative study of fasciectomy and dermofasciectomy in one hundred patients. J Hand Surg [Br]J. 1984; 9:156-62.
18. Schneider LH, Hankin FM, Eisenberg T. Surgery of Dupuytren's disease: a review of the open palm method. J Hand Surg [Am]J. 1986; 11:23-7.
19. Hueston JT. Recurrent Dupuytren's contracture.Plast Reconstr Surg. 1962; 31:66-9.
20. McFarlane RM. Patterns of the diseased fascia in the fingers in Dupuytren's contracture. Plast Reconstr Surg. 1974; 54:31-44.
I - Professor of Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS) Medical School. Specialist in Hand Surgery by AMB and the Brazilian Society of Hand Surgery.
II - Candidate Member of SBCP.
III - Head of the Plastic Surgery Service of Hospital São Lucas - PUCRS.
Study performed at the Plastic Surgery Service of São Lucas Hospital of Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS)
Address for correspondence:
Jefferson Braga Silva, MD
Av. Ipiranga, 6690 - Conj. 216 Centro Clínico PUCRS
90610-000 - Porto Alegre - RS Brazil
Phone: (55 51) 3315-6277 - Fax: (55 51) 3320-5040
e-mail: jeffmao@terra.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter