

Case Report - Year 2018 - Volume 33 -
V-Y flap of advancement after the recurrence of perineal cancer: case report and literature review
Retalho VY de avanço após recidiva de neoplasia perianal: relato de caso e revisão da literatura
ABSTRACT
INTRODUCTION: Anal cancer is a rare disease, with an increasing incidence. Flaps are complex options for closing large areas. The perineal region may be affected by extensive lesions that require the use of flaps for repair.
CASE REPORT: A 56-year-old female patient with anal adenocarcinoma underwent abdominoperineal amputation surgery of the rectum with postoperative radiotherapy for 2 years. She had cutaneous recurrence of the neoplastic lesion with indication of surgical margin expansion to control the local recurrence. After extensive resection with safety margins of the skin defect, we selected double V-Y flap of length 15 cm each and a total thickness of the gluteal subcutaneous tissue (ST) to fill up the dead space caused by resection and advancement of the defect. Intravenous antibiotic prophylaxis and deep venous thrombosis prophylaxis were administered. The patient progressed well from the procedure, with no problems.
DISCUSSION: A flap is a tissue that is mobilized based on vascular anatomy. Flaps based on the subdermal plexus include bipedicle, advancement (V-Y), rotation, and transposition flaps. Perineum reconstructions are often indicated for tumors, trauma, infections, burns, or pressure sores. The anal region is divided into the anal canal and the anal margin. Among the histological types of anal cancer, the most prevalent are squamous cell carcinoma (most common histology), adenocarcinoma, melanoma, small cell carcinoma, and sarcomas. The risk of regional recurrence after treatment can reach approximately 30% of cases and is the most frequent recurrence pattern.
Keywords: Adenocarcinoma; Perforator flap; Anal canal.
RESUMO
INTRODUÇÃO: O câncer anal é uma doença rara, cuja incidência está aumentando. Os retalhos são opções complexas de fechamento quando abrangem grandes áreas. A região perineal pode ser acometida por extensas lesões, requerendo utilização de retalhos.
RELATO DE CASO: Paciente feminina, 56 anos, diagnosticada com adenocarcinoma anal, foi submetida à cirurgia de amputação abdominoperineal do reto associada à radioterapia pós-operatória há 2 anos. Apresentou recidiva cutânea da lesão neoplásica, com indicação de ampliação de margem cirúrgica para controle da recidiva. Após ampla ressecção com margem de segurança o defeito cutâneo, optou-se por duplo retalho em V-Y com 15 cm de comprimento cada e espessura total do tecido celular subcutâneo (TCS) de região glétea para preenchimento do espaço morto deixado pela ressecção e avanço sobre o defeito. Implementou-se antibioticoprofilaxia endovenosa e profilaxia para trombose venosa profunda. Paciente evoluiu bem do procedimento sem intercorrências.
DISCUSSÃO: Retalho é um tecido que é mobilizado conforme sua anatomia vascular. Retalhos baseados no plexo subdérmico incluem os bipediculados, de avanço (V-Y), retalhos de rotação e transposição. Reconstruções de períneo são indicadas devido a tumores, traumas, infecções, queimaduras ou élceras de pressão. A região anal é dividida em canal anal e margem anal. Dentre os tipos histológicos de neoplasia na região do canal anal, podem ser citados: carcinoma de células escamosas (histologia mais comum), adenocarcinoma, melanoma, carcinoma de pequenas células e sarcomas. O risco de recidiva locorregional, após tratamento, pode atingir cerca de 30% dos casos e é o padrão de recidiva mais frequente.
Palavras-chave: Adenocarcinoma; Retalho perfurante; Canal anal.
Anal cancer is a rare disease, with an increasing incidence. The most common histologic type is squamous cell carcinoma, typically affecting individuals older than 60 years. This article reports a case of perianal cutaneous recurrent anal carcinoma subjected to double V-Y flap.
It is interesting that most studies have reported that the advancement V-Y flap is used to close bedsores and benign disease, but it may also be used for other types of defect, showing the versatility of the flaps. The flaps are made based on the vascular structure of the region, considering the vascular, physiological, and biomechanical skin patterns. The V-Y flap is one of the advancement flap types, which also include uniped, bipediculate, Y-V, and pediculated island of subcutaneous tissue flaps.
CASE REPORT
A 56-year-old female patient with anal adenocarcinoma underwent abdominoperineal amputation surgery of the rectum with postoperative radiotherapy for two years. She had cutaneous recurrence of the neoplastic lesion with indication of a surgical margin expansion to control the local recurrence (Figure 1).
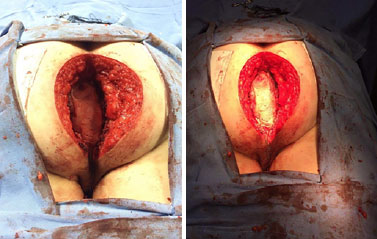
Figure 1. Enlargement of surgical margin.
After extensive resection with safety margins, the resulting skin defect was approximately 38 cm × 32 cm in diameter and 25-cm deep, and the rear wall of the uterus at the posterior limit. We selected double V-Y flap of length 15 cm each and a total thickness of the gluteal subcutaneous tissue (ST) to fill the dead space caused by resection and advancement of the defect (Figure 2).
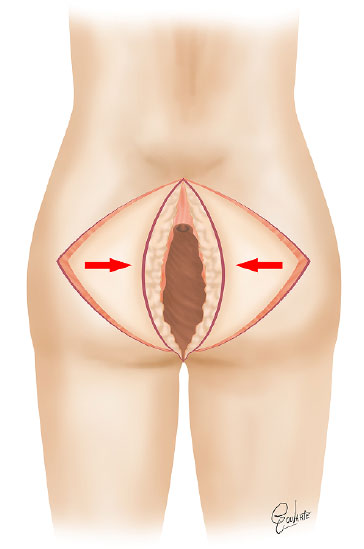
Figure 2. Scheme of the double V-Y flap.
Despite the large volume of the flaps, a small residual dead space remained at the bottom of the lesion, and a 5.2-cm Potomac drain was placed to prevent collection formation.
Intravenous antibiotic prophylaxis for deep venous thrombosis (DVT) was administered.
The patient progressed well from the procedure, without problems with the late postoperative period, showing good healing (Figures 3 and 4).

Figure 3. Double V-Y flap of 15 cm length each and total thickness in the gluteal region.

Figure 4. Late postoperative aspect.
DISCUSSION
We report a case of a perianal lesion reconstruction surgery with a V-Y flap after the recurrence of perineal cancer. The flaps are complex options for closing large areas. The aim of this type of surgery was to cover, protect, and fill the area of the disease. The perineal region may be affected by extensive lesions, requiring patches for repair1.
The flap is a tissue that is mobilized based on its vascular anatomy. The flaps are usually composed of: skin, skin and fascia, skin and muscle or skin, or muscle and bone. For tissue survival, dependence on deployment of the vascular anatomy of skin tissue and underlying tissue is not needed.
Flaps based on the subdermal plexus include bipedicle, advancement (V-Y), rotation, and transposition flaps. Perineum reconstructions are often indicated due to tumors, trauma, infections, burns, or pressure sores. The wounds may be extensive and infections are frequent because of proximity to the urethra and anus. Prostheses and local radiation therapy may aggravate the injury2.
Among the muscles that can be used as donors for the damaged area is the sartorius, which has multiple vascular pedicles, which limit its arc of rotation. The gracilis muscle is a bow with two-way rotation and can be used for reconstruction of the groin and perineum, besides the vagina, penis, scrotum, and anal sphincter. The tensor fascia lata, rectus femoris, and rectus abdominis are ideal for irradiated flaps of the perineum, gluteus maximum, and thigh gluteus. The extension flap is important because the larger the flap, the greater the blood supply3,4.
The anal region is divided into the anal canal and anal margin. Anatomically, the canal extends from the straight to the perianal skin, with a length of approximately 2.5 to 3.5 cm. The upper part of the canal is lined with mucus similar to that in the rectum, and the bottom part is lined by epithelium similar to that in the perianal skin. Among these regions, the anal and anal valve columns are the dentate line. There are two types of tumors in this region based on the location: those originating from the mucous membranes, called anal cancer, and those from the skin or distal portion of the mucocutaneous junction, called anal margin cancer5,6.
Among the histological types of anal cancer, the most prevalent are squamous cell carcinoma (most common histology), adenocarcinoma, melanoma, small cell carcinoma, and sarcomas7.
Tumors of the perianal skin region are generally squamous cell carcinomas, and basal cell carcinoma, melanoma, Bowen’s disease, and extramammary Paget’s disease can also exist6,8.
Most anal cancers originate from the mucosa cells, and below it are glands that produce mucus. Adenocarcinoma is an anal cancer from these glandular cells6,8.
Anal cancer is rare and less common than colon or rectum cancer, but the number of cases is increasing. It is rare in people younger than 35 years and found mainly in older adults with a mean age at onset of 60 years6,8.
Despite the knowledge of some risk factors for anal cancer (human papilloma virus infection [HPV], with subtype 16 related to squamous cell carcinoma and 18 to adenocarcinoma, cigarette smoking, low immunity, anal receptive sex, and multiple sexual partners), the exact cause is unknown6,8.
Most patients with anal cancer present with initial rectal bleeding symptoms. Pain and rectal mass sensation may occur in up to 30% of cases.
Anal cancer is a predominantly regional disease with local extent of the primary tumor and spread to the lymph nodes of the inguinal and pelvic region. Hematogenous dissemination is rare. Local spread to the rectum and/or the perianal skin occurs in approximately 50% of cases. The deep invasion of the rectovaginal septum occurs in 10% of cases6.
The risk of regional recurrence after treatment can reach approximately 30% of cases and is the most frequent recurrence pattern7. If the cancer recurs in the anus or a nearby lymph injury after treatment, the conduit depends on the treatment performed previously, and generally progresses with colostomy6.
Some cases are diagnosed by screening tests, such as digital rectal examination and/or anal Papanicolaou test6,8.
COLLABORATIONS
GJSAF Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; writing the manuscript or critical review of its contents.
EF Writing the manuscript or critical review of its contents.
LPSR Writing the manuscript or critical review of its contents.
IAYK Writing the manuscript or critical review of its contents.
FYK Writing the manuscript or critical review of its contents.
ERGF Writing the manuscript or critical review of its contents.
REFERENCES
1. Gehlen D, Grandi J, Reis LFM, Silva MO, Porcides RD, Pitanguy I. Retalho gléteo de avanço em V-Y fasciocutâneo para tratamento de élcera sacra. Rev Bras Cir Plást. 2013;28(3):70.
2. Calil JA, Ferreira LM, Neto MS, Castilho HT, Garcia EB. Aplicação clínica do retalho fáscio-cutâneo da região posterior da coxa em V-Y. Rev Assoc Med Bras. 2001;47(4):311-9. DOI: http://dx.doi.org/10.1590/S0104-42302001000400033
3. Barreiro GC, Millan LS, Nakamoto H, Montag E, Tuma P Jr, Ferreira MC. Reconstruções pelveperineais com uso de retalhos cutâneos baseados em vasos perfurantes: experiência clínica com 22 casos. Rev Bras Cir Plást. 2011;26(4):680-4. DOI: http://dx.doi.org/10.1590/S1983-51752011000400025
4. Laitano FF, Teixeira LR, Siqueira EJ, Alvarez GS, Oliveira MP. Tumor cutâneo em parede nasal lateral e as opções de retalhos cutâneos para reconstrução após ressecção neoplásica. Rev AMRIGS. 2012;56(3):229-33.
5. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471-4. DOI: http://dx.doi.org/10.1245/s10434-010-0985-4
6. American Cancer Society. Cancer Facts & Figures 2016. Atlanta: American Cancer Society; 2016.
7. Ibañez N, Abrisqueta J, Luján J, Hernández Q, Parrilla P. El colgajo V-Y como método de reparación de defectos perianales extensos. Cir Esp. 2016;94(9):525-30. DOI: http://dx.doi.org/10.1016/j.ciresp.2016.06.006
8. Gürbulak EK, Akgün İE, Ömeroğlu S, Öz A. Giant perianal condyloma acuminatum: Reconstruction with bilateral gluteal fasciocutaneous V-Y advancement flap. Ulus Cerrahi Derg. 2015;31(3):170-3.
1. Clínica Belvivere de Cirurgia Plástica e Laser, Criciéma, SC, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
3. Universidade do Extremo Sul Catarinense, Criciéma, SC, Brazil
4. Escola Paulista de Medicina, Universidade Federal de São Paulo, SP, Brazil
Institution: Clínica Belvivere de Cirurgia Plástica e Laser, Criciéma, SC, Brazil.
Corresponding author:
Glayse June Sasaki Acacio Favarin
Rua Coronel Pedro Benedet, 505, sala 10
Centro - Criciéma, SC, Brazil - Zip Code 88801-250
E-mail: glaysejune@yahoo.com.br
Article received: October 22, 2016.
Article accepted: January 26, 2018.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter