

Original Article - Year 2018 - Volume 33 -
Evaluation of the Millard technique associated with zetaplasty in the treatment of patients with unilateral cleft lip
Avaliação da técnica de Millard associada à zetaplastia no tratamento de portadores de fenda labial unilateral
ABSTRACT
INTRODUCTION: Cleft lips are very common congenital deformities that affect, in varying degrees, the soft tissues and bone structures of the middle third of the face. Surgical treatment should be performed early and a protocol must be followed, which varies according to the reference center. There are numerous surgical techniques for lip repair, and among them, the Millard technique is the most used. The objective is to evaluate the association of the Millard type I with zetaplasty mucosal technique (used by the author) as the surgery of choice for primary lip repair in patients with unilateral cleft lip, and to understand whether the techniques are appropriate when the number of second surgeries (reoperation) is low.
METHODS: Sixty-five patients underwent operations by this technique from January 2007 to December 2012 in Santos, all of whom were followed for at least four years.
RESULTS: Of the 65 patients, 10 (15%) were considered to present "unsatisfactory results" and underwent reoperation.
CONCLUSION: Primary cheiloplasty with zetaplasty-associated Millard type I is appropriate when the number of reoperations is low, and our results agree with the current literature.
Keywords: Cleft lip; Reconstructive surgical procedures; Congenital abnormalities.
RESUMO
INTRODUÇÃO: As fendas labiais são deformidades congênitas muito comuns e acometem em grau variável as partes moles e estruturas ósseas do terço médio da face. O tratamento cirúrgico deve ser precoce e segue um protocolo que varia de acordo com o centro de referência. As técnicas cirúrgicas de queiloplastia são inúmeras e, dentre elas, uma das mais utilizadas é a de Millard. O objetivo é avaliar a técnica de Millard tipo I associada a uma zetaplastia da mucosa (técnica empregada pelo autor) como cirurgia de escolha na queiloplastia primária dos pacientes portadores de fenda labial unilateral, entendendo que a técnica é adequada se o número de cirurgias secundárias (reoperações) for baixo.
MÉTODOS: Foram operados 65 pacientes por essa técnica no período de janeiro de 2007 a dezembro de 2012 em Santos. Todos acompanhados por no mínimo quatro anos.
RESULTADOS: Dos 65 pacientes, 10 (15%) foram considerados "resultados insatisfatórios" e reoperados.
CONCLUSÃO: Queiloplastia primária à Millard tipo I associada a zetaplastia é adequada, com um número de reoperações baixo e semelhantes aos da literatura atual.
Palavras-chave: Fenda labial; Procedimentos cirúrgicos reconstrutivos; Anomalias congênitas.
Cleft lips are common congenital deformities that affect, in variable degrees, the soft tissues and bone structures of the midface1. The incidence of cleft lip ranges from 1/500 to 1/1000 live births, and this disorder is more frequent in the yellow race than in Caucasians and blacks.
The etiology of this disease is multifactorial. The genetic factors are identified in 35% of patients with this disease, and 65% of cleft lip incidences are due to mutations in embryogenesis that are caused by environmental factors, such as maternal endocrine factors (diabetes, hypothyroidism, increased secretion of the suprarenal glands), infections during pregnancy (influenza virus, rubella, toxoplasmosis), nutrient deficiency (folic acid), medication use during pregnancy (anticonvulsants, aspirin, corticosteroids, antiblastic, vitamin A), and exposure to radiation.
The treatment for patients with cleft lip is multidisciplinary2. The surgical steps are fundamental and must be practiced in accordance with the reference center's protocols3. Cleft lip surgery is recommended, and while there are several surgery techniques4 (Fisher5, Le Mesurier6, Spina7, Randall8, and others) today, the Millard I technique remains most frequently used9,10.
In 1955, Ralph D. Millard Jr.11 introduced the advancement and rotation of the lip flap technique, with final scar minimization of the philtral crest and respecting of the bow cupid, which are very important anatomical details in labial aesthetics (Figure 1). His technique quickly became popular, and today, it is the most used technique worldwide.

OBJECTIVE
The aim of this study was to evaluate the association of the Millard I technique12 with mucosalzetaplasty (author's adopted technique) as major surgeries in primary cleft lip repair in patients with unilateral cleft lip. We concluded that both techniques are appropriate when the number of secondary surgeries (reoperations) is low.
METHODS
Of the 1,354 patients with facial malformations registered at the Centro de Tratamento de Malformações Craniofaciais (CTMC) in Santos, 65 patients with unilateral cleft lip were selected, who underwent operations between January 2007 and December 2012 and were followed-up for at least four years. This study was previously approved by the ethics committee in human research of the University Center Lusíada - CEPSH UNILUS, on November 25, 2013, with protocol number: 208/2013 and CAAE: 24482513.4. 0000.5436.
As inclusion criteria, patients with unilateral cleft lip were exclusively selected, and those with cleft palate or associated syndromes were excluded. All patients were monitored in the CTMC from birth, made regular use of lip tape, and underwent Millard I lip repair with mucosal zetaplasty (procedure adopted by the author that prevents the formation of late mucosal retraction).
The CTMC protocol involves performing cleft lip repair when the patient is six months of age. In addition, the patients must accord to the "rule of ten"13, which has three basic requirements: hemoglobin > 10, weight > 10 lbs (4.5 kg), and age > 10 weeks. Monitoring and treatment are carried out from birth to early adulthood (21 years).
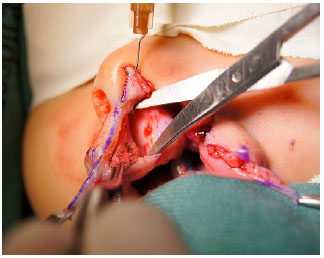
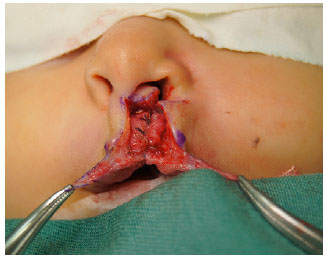
The surgical technique consists of an incision on the limits of the cleft lip, concocting an infracolumelar triangular fasciocutaneous flap in the medial portion of the lip, which will undergo rotation, and performing a perialar incision on the lip of the lateral portion of the cleft, which will make an advancement. Then the lip orbicularis muscles are dissected, disinserted from their anomalous position, rotated, and sutured with an absorbable surgical suture 3-0. The mucosa synthesis is made with a 4-0 suture, and the skin is closed with a surgical suture 6-0 (Figures 2 to 6).



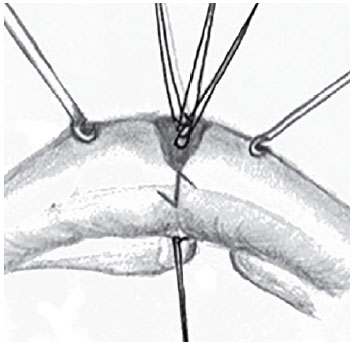
At this moment, zetaplasty is performed in the transition between the dry and wet mucosa (Figure 7), which can fix the aretraction in this place that is often caused by the lack of remaining tissue (Figure 8 to 10).



All patients who evolved a labial notch (Figure 11), mucosaretraction, mucocutaneous line break, or enlarged scar, which can arise in immediate or late postoperative periods and are considered "unsatisfactory results," underwent a secondary cleft lip surgery in this study.

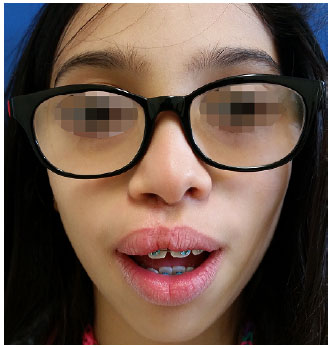
Patients who achieved an adequate aesthetic lip, without the mentioned deformities, and did not require secondary surgery were considered to achieve "satisfactory results" (Figures 12 to 14).


RESULTS
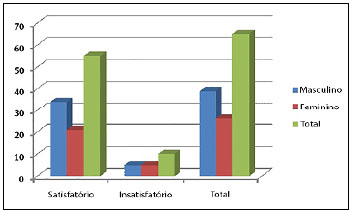
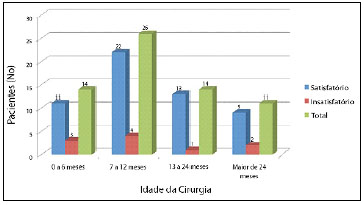
From 2007 to 2012, 65 patients, from a total of 1,354 patients who are registered in CTMC and underwent operations, were selected according to the inclusion criteria. Of these 65 patients, 39 (60%) were men and 26 (40%) were women (Figure 15). Most of them (45, 69%) had left cleft lip, and 40 (61.5%) patients underwent operations before one year of age (Figure 16) (Table 1).
From the 65 patients, 10 (15%) were considered to achieve "unsatisfactory results" and underwent reoperation. Of these, seven (70%) presented a labial notch and three (30%) had an enlarged scar (Table 2).
The remaining 55 (85%) patients did not require secondary surgery and were considered to achieve "satisfactory results" (Figure 16).
DISCUSSION
The search for the best aesthetic and functional results and the need to evaluate surgical techniques are common modern problems for plastic surgeons. A technique is determined to be appropriate when it can solve the deformity in question with a single operation, and secondary surgery is indicative of poor outcome. Hence, the aim of this study was to evaluate the use of Millard I cleft lip surgery technique with mucosal zetaplasty12,14 in the correction of unilateral cleft lips.
After operation, these 65 patients were followed-up for at least four years. Ten (15%) of the patients required a secondary lip repair due to "unsatisfactory results."
This percentage of reoperations is similar to that of Cheema e Asim15, who published an analysis of their surgeries in 2014. They operated on 1,907 patients and performed secondary lip repair for 189 (10%) of cases, after using Millard I as the first technique. This study showed that 65% of the corrections were due to a lip notch, which is similar to our 70% frequency of notches.
Another similar result was obtained by Rossell-Perry16 in 2008, who used a combination Reichert-Millard technique in 112 cases, and 14.2% of the patients required secondary lip repairs.
Baek et al.17 also reported that 14.4% of his 145 patients who underwent a new technique called "Start," a Millard variation, required secondary surgeries.
In Brazil, the study of Alonso et al.3 showed that of 108 procedures, 17.5% required secondary surgical revision of the lip/nose.
However, there are also studies in the literature that used the Millard unilateral lip repair technique and showed lower rates of secondary surgeries,18,19 between 6% and 8%, and larger indices1,15, between 35% and 46%
.
CONCLUSION
This study showed that the Millard I with zetaplasty mucosa lip repair technique is exclusively suitable for patients with unilateral cleft lip.
COLLABORATIONS
DCL Conception and design of the study; writing the manuscript; analysis and/or interpretation of data; completion of surgeries and/or experiments.
AFCC Conception and design of the study; writing the manuscript; analysis and/or interpretation of data; completion of surgeries and/or experiments.
LG Analysis and/or interpretation of data; completion of surgeries and/or experiments.
MRM Completion of surgeries and/or experiments.
OS Critical review of its contents; final approval of the manuscript.
REFERENCES
1. Modolin M, Kamakura L, Cerqueira EM. Classificação, etiologia, patogenia e incidência das fissuras labiopalatinas. In: Carreirão S, Lessa S, Zanini AS, eds. Tratamento das Fissuras Labiopalatinas. Rio de Janeiro: MEDSI; 1996.
2. Paranaíba LMR, Almeida H, Barros LM, Martelli DRB, Orsi Júnior JD, Martelli Júnior H. Técnicas cirúrgicas correntes para fissuras lábio-palatinas, em Minas Gerais, Brasil. Braz J Otorhinolaryngol. 2009;75(6):839-43. DOI: http://dx.doi.org/10.1590/S1808-86942009000600011
3. Alonso N, Tanikawa DYS, Lima Junior JE, Ferreira MC. Avaliação comparativa e evolutiva dos protocolos de atendimento dos pacientes fissurados. Rev Bras Cir Plást. 2010;25(3):434-8. DOI: http://dx.doi.org/10.1590/S1983-51752010000300006
4. Sitzman TJ, Girotto JA, Marcus JF. Current surgical practices in cleft care: unilateral cleft lip repair. Plast Reconstr Surg. 2008;121(2):261e-270e. DOI: http://dx.doi.org/10.1097/PRS.0b013e31816a9feb
5. Fisher DM. Unilateral cleft lip repair: an anatomical subunit approximation technique. Plast Reconstr Surg. 2005;116(1):61-71. PMID: 15988248 DOI: http://dx.doi.org/10.1097/01.PRS.0000169693.87591.9B
6. Le Mesurier AB. A method of cutting and suturing the lip in the treatment of complete unilateral clefts. Plast Reconstr Surg (1946). 1949;4(1):1-12. DOI: http://dx.doi.org/10.1097/00006534-194901000-00001
7. Spina V, Ludovici O. Conservative technique for treatment of unilateral cleft lip: Reconstruction of the midline tubercle of vermilion 1. Br J Plast Surg. 1960-1961;13:110-7. DOI: http://dx.doi.org/10.1016/S0007-1226(60)80027-6
8.Randall P. A triangular flap operation for the primary repair of unilateral cleft of the lip. Plast Reconstr Surg Transplant Bull. 1959;23(4):331-47.
9. Franco D, Eyler AD. Cirurgia de Fissurados: Detalhes que Facilitam. Rev Bras Cir Plast. 2003;18(1):55-69.
10. Mehrotra D, Pradhan R. Cleft lip: our experience in repair. J Maxillofac Oral Surg. 2010;9(1):60-3. DOI: http://dx.doi.org/10.1007/s12663-010-0017-8
11. Millard DR. A primary camouflage of the unilateral harelook. In: Skoog T, Ivy RH, eds. Transactions of the International Society of Plastic Surgeons. Baltimore: Williams & Wilkins; 1957. p. 160-6.
12. Narayanan PV, Adenwalla HS. Notch-free vermillion after unilateral cleft lip repair: The Charles Pinto Centre protocol. Indian J Plast Surg. 2008;41(2):167-70. DOI: http://dx.doi.org/10.4103/0970-0358.44935
13. Figueiredo JCA, Freitas AG. Fissuras labiais. In: Mélega JM, ed. Cirurgia Plástica: Fundamentos e Arte. Rio de Janeiro: Guanabara Koogan; 2008. p. 89-109.
14. Adenwalla HS, Narayanan, PV. Primary unilateral cleft lip repair. Indian J Plast Surg. 2009;42 Suppl:S62-70. DOI: http://dx.doi.org/10.4103/0970-0358.57189
15. Cheema AS, Asim M. An analysis of deformities in revision surgeries for secondary unilateral cleft lip. J Coll Physicians Surg Pakistan. 2014;24(9):666-9.
16. Rossell-Perry P. Combinación de la técnica de Reichert-Millard en el tratamiento de la fissura labial unilateral. Acta Med Peruana. 2008;25(1):16-21.
17. Baek RM, Choi JH, Kim BK. Practical Repair Method for Unilateral Cleft Lips: Straight-Line Advanced Release Technique. Ann Plast Surg. 2006;76(4):399-405. PMID: 25730452 DOI: http://dx.doi.org/10.1097/SAP.0000000000000425
18. Becker M, Svensson H, McWilliam J, Sarnäs KV, Jacobsson S. Millard repair of unilateral isolated cleft lip: a 25-year follow-up. Scand J Plast Reconstr Hand Surg. 1998;32(4):387-94. DOI: http://dx.doi.org/10.1080/02844319850158471
19. Lee SW, Kim MH, Baek RM. Correction of secondary vermilion notching deformity in unilateral cleft lip patients: complete revision of two errors. J Craniomaxillofac Surg. 2011;39(5):326-9. PMID: 20822915 DOI: http://dx.doi.org/10.1016/j.jcms.2010.07.001
Figure 1. Scheme of the rotation advancement (Millard I) technique.
Source: Patient from the Craniofacial Malformation Treatment Center.
Figure 3. Preparation of skin flaps in the upper lip.
Source: Patient from the Craniofacial Malformation Treatment Center.
Figure 4. Repair of the orbicularis oris muscle.
Source: Patient from the Craniofacial Malformation Treatment Center.
Figure 2. Markings for cheiloplasty using the rotation advancement technique.
Source: Patient from the Craniofacial Malformation Treatment Center.
Figure 5. Rotation and advancement of the skin flaps.
Source: Patient from the Craniofacial Malformation Treatment Center.
Source: Patient from the Craniofacial Malformation Treatment Center.
Figure 8. Aspects of the groove on the upper lip mucosa after cheiloplasty.
Figure 6. Reconstructive surgery (cheiloplasty) of the skin.
Source: Patient from the Craniofacial Malformation Treatment Center.
Figure 9. Markings for Z-plasty on the upper lip groove.
Source: Narayanan et al., 200812.
Figure 7. Scheme of Z-plasty in the mucosa.
Source: Patient from the Craniofacial Malformation Treatment Center.
Figure 10. Aspect of the lip mucosa after Z-plasty.
Source: Patient from the Craniofacial Malformation Treatment Center.
Source: Patient from the Craniofacial Malformation Treatment Center.
Figure 11. Aspect of the upper lip groove after surgery.
Figure 13. Postoperative results of cheiloplasty (Millard I).
Source: Patient from the Craniofacial Malformation Treatment Center.
Source: Patient from the Craniofacial Malformation Treatment Center.
Figure 12. Postoperative results of cheiloplasty (Millard I).
Figure 14. Postoperative results of cheiloplasty (Millard I).
Table 2. Incidences of secondary cheiloplasty in the postoperative period and complications in patients with unsatisfactory results.
Figure 15. Relationship between gender and degree of satisfaction with the surgical results.
Figure 16. Relationship between patient age at the time of surgery and the degree of satisfaction with the surgical results.
Table 1. Profile of the study patients and the degree of satisfaction with the surgical results.
1. Hospital Estadual Guilherme Álvaro, Santos, SP, Brazil
2. Centro de Tratamento de Malformações Cranio-faciais Mário Covas
3. Clínica Osvaldo Saldanha, Santos, SP, Brazil
4. Hospital São Lucas, Santos, SP, Brazil
Institution: Centro de Tratamento das Malformações Craniofaciais Mário Covas, Hospital Estadual Guilherme Álvaro, Santos, SP, Brazil.
Corresponding author:
Daniel de Cazeto Lopes
Rua Mario Tamashiro, 47 - Canto do Forte
Praia Grande, SP, Brazil - Zip Code 11700-180
E-mail: danielcazeto@yahoo.com.br
Article received: September 29, 2016.
Article accepted: July 10, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter