

Original Article - Year 2018 - Volume 33 -
Bichectomy: technical systematization applied in 27 consecutive cases
Bichectomia: sistematização técnica aplicada a 27 casos consecutivos
ABSTRACT
INTRODUCTION: Despite buccal fat removal having been performed for a long time, its popularity has increased only in recent years, leading to a rise in the demand for bichectomy in plastic surgery clinics. Buccal fat pad removal is still considered controversial, even when properly indicated, especially with the lack of a systematized surgical technique to make it safe and reproducible.
METHODS: The intraoral bichectomy described herein was systematically applied in 27 consecutive patients from January 5, 2016 to December 15, 2016.
RESULTS: The mean patient age was 32 years; 15% were men, and 85% were women. Isolated buccal fat pad removal was performed in six patients (22%) and in combination with other procedures in 21 patients (78%). The main procedure combined was neck liposuction (55%), and most patients were operated under general anesthesia (93%). No permanent or significant complications occurred, and there were only two minor complications, i.e., inferior mandibular neuropathy and significant swelling, which improved without treatment during the following weeks.
CONCLUSIONS: Buccal fat removal can be performed in a predictable, fast, and safe manner, leading to volumetric reduction of the lower third of the face, enhancing facial shape. When applied in a safe surgical environment, following all surgical security standards and considering the complex anatomical boundaries of the cheek, our technique can yield secure and satisfactory outcomes both for surgeons and patients.
Keywords: Rhytidoplasty; Anatomy regional; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: Embora realizada há muito tempo, a remoção da bola de Bichat ganhou notoriedade nos últimos anos devido a sua grande procura nos consultórios do cirurgião plástico. Mesmo quando adequadamente indicada, ainda é considerada um procedimento controverso, uma vez que ainda não existe uma técnica cirúrgica sistematizada na literatura atual, visando torná-la segura e reprodutível.
MÉTODOS: A técnica da bichectomia intraoral descrita no trabalho foi aplicada de maneira sistemática em uma série de 27 pacientes consecutivos, no período de 5 de janeiro de 2016 a 15 de dezembro de 2016.
RESULTADOS: A idade média dos pacientes foi de 32 anos, sendo 15% do sexo masculino e 85% do sexo feminino. A bichectomia foi realizada isoladamente em 6 pacientes (22%) e em conjunto com outros procedimentos em 21 pacientes (78%). O procedimento mais comumente associado foi a lipoaspiração cervical, realizada em 55% dos pacientes. A imensa maioria dos casos foram operados com anestesia geral (93%). Nenhuma complicação permanente e importante foi verificada no pós-operatório, apenas um caso de neuropatia transitória do ramo bucal e um caso de edema mais pronunciado, que prontamente se resolveram nas semanas seguintes.
CONCLUSÃO: A remoção de gordura bucal pode ser realizada de forma previsível, rápida e segura, proporcionando diminuição volumétrica do terço inferior facial, com maior realce dos contornos faciais. Quando aplicada em um ambiente cirúrgico seguro, seguindo todos os padrões de segurança da cirurgia e respeitando os complexos limites anatômicos da região, nossa técnica levará os cirurgiões e pacientes a um resultado seguro e satisfatório.
Palavras-chave: Ritidoplastia; Anatomia regional; Procedimentos cirúrgicos reconstrutivos.
For many years, the Bichat fat ball has caught the attention of anatomists and facial surgeons. Its peculiar anatomy and the possibility of using this structure for aesthetic or reconstructive purposes have already been widely studied by several authors1-7. Satisfactory aesthetic results can be obtained by manipulating the buccal fat, either through its transposition as a graft or flap for filling or resection, i.e., bichectomy3,6,8-10.
Although performed a long time ago for both aesthetic purposes and repair3,11, the removal of the Bichat fat ball is increasingly sought by plastic surgeons. The search for a diminished cheek volume, leading to a "thinning" of the face with zygomatic enhancement, has been the main goal sought, possibly motivated by changes in the current aesthetic standards.
The removal of oral fat allows for predictable and highly satisfactory results4,7. Even when properly indicated, it is still a controversial procedure, since it does not have a surgical technique adequately systematized in the current literature to make it safe and reproducible, considering the intricate and challenging anatomy of the region.
OBJECTIVE
The aim of this study was to describe a series of 27 patients in whom our intraoral bichectomy technique was applied systematically so that safe, predictable, and satisfactory results could be achieved, providing more confidence to both surgeons and patients during the procedure.
METHODS
The described intraoral bichectomy technique was systematically applied in a series of 27 consecutive patients operated on at the São Lucas Hospital of PUCRS, Porto Alegre, RS from January 5, 2016 to December 15, 2016, who sought to diminish their cheeks and/or to thin their face owing to the complaint of having a very "rounded" face. The work properly followed the principles of Helsinki, and all patients were operated on after signing the informed consent form. The mean age of the patients was 32 years; 15% were men, and 85% were women. Bichectomy was performed alone in six patients (22%) and together with other procedures in 21 patients (78%). The most commonly associated procedure was cervical liposuction in 55% of the patients. The majority of the patients were operated on under general anesthesia (93%).
In all cases, the Bichat ball was removed following the technique described herein. Table 1 shows the characteristics of the patients.
Surgical technique
Positioning of the surgeon and the patients
The proper positioning of both the patients and the surgeon and his assistant is critical for a better view and approach of the region. We began with the patients in the supine position with their head elevated, preferably at 45º, which caused the Bichat ball to "fall" lower and move closer to the incision. The surgeon started at the right side of the patients' head to approach the left cheek, changing sides when approaching the right cheek; this sequence made the surgery more comfortable and promoted a better visualization of the structures.
Intraoral incision planning
Proper planning of the intraoral incision is critical for a direct and accurate approach to the Bichat ball.
An ideal and accurate incision should allow a safe and predictable approach to the oral fat with adequate visualization and exposure, preserving the buccal branches of the facial nerve and parotid duct and reducing the risk of bleeding from the transverse facial vein.
A properly planned incision will make the surgery easier to perform. To systematize it in the best possible manner, we have idealized the "intraoral" technique defined as follows (Figure 1):
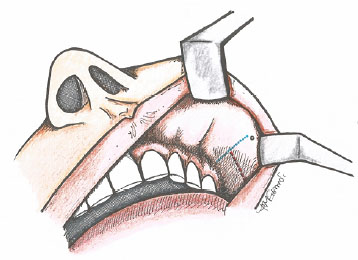
Figure 1. Schematic drawing demonstrating the intraoral "T" technique: Step 1: Identify the parotid duct (right-hand point); Step 2: Identify the intraoral vein (upper line); Step 3: Draw a perpendicular line in the middle of the distance between the duct and the gingivobuccal sulcus; this line starts in the vein and ends at the level of the second to the third molar, measuring approximately 2 cm. Step 4: Ensure that this line (which will be the incision line) forms a "T" along with the vein providing the precise location of the incised site.
•Step 1: Identify the parotid duct.
•Step 2: Identify the intraoral vein.
•Step 3: Draw a perpendicular line in the middle of the distance between the duct and the gingivobuccal sulcus; this line starts in the vein and ends at the level of the second to the third molar measuring approximately 2 cm.
•Step 4: Ensure that this line (which will be the incision line) forms a "T" along with the vein providing the precise location of the incised site.
Anesthesia and infiltration
The preference is to perform bichectomy under general anesthesia, which provides greater safety, better airway control, more comfort for the patient and surgeon, and better conditions for performing cervical liposuction or other procedures; these were observed in the majority of the cases.
To reduce the risk of bleeding that could make it difficult to identify adjacent anatomical structures and buccal fat, an extremely cautious infiltration of the area to be incised was performed, with 2% xylocaine with 1: 150,000 epinephrine; this infiltration was limited to the mucosa and buccinator muscle.
It is not advised to infiltrate large volumes of solution as this often distorts the local anatomy, making it difficult to identify the structures accurately, as well as to use anesthetics (such as ropivacaine) for a longer period owing to the fact that they can cause prolonged facial paralysis and consequently unnecessary concerns to both the surgeon and the patient
Incision and dissection
Once the incision line has been defined by the intraoral T technique, the mucosa was incised using a knife blade 15. The buccinator muscle can now be visualized via divulsion using Kelly or Halsted forceps; we did not directly incise the muscle, which greatly reduced bleeding. The divulsion of the muscle should always be performed parallel to its fibers, reducing their rupture and surgical trauma.
Accurate dissection and identification of the Bichat fat
After muscular opening, the buccal space and buccal fat was also accessed via divulsion using the Halsted caliper on the right hand of the surgeon. Thereafter, a long Langenbeck retractor held on the left hand of the surgeon was inserted, providing better surgical field and visualization.
The dissection was continued by spreading the forceps in a supero-posterior direction towards the midline between the lower edge of the zygomatic arch and the earlobe. The surgeon placed the index finger of the hand, holding the retractor in this region to indicate the location of the Bichat ball more accurately. We do not advise maneuvers that perform external digital compression, as they result in anatomical distortion and access difficulty.
The divulsion proceeded until the oral fat (always located at the bottom of the "tunnel") was identified. When it was difficult to identify the fat, it could be because of an even posterior position of the fat (which occurs as a function of decubitus). In this case, we recommend identifying the anterior border of the masseter muscle (with its "white aponeurotic aspect") and continuing the dissection by the anterior face of the masseter in the posterior direction. In this manner, the buccal and pre-masseteric space can be accessed, and the Bichat fat ball invariably will be located there.
Less experienced surgeons may confuse the Bichat fat with the subcutaneous tissue and/or salivary glands (the two with a lobulated and a less intense yellow appearance), and in the attempt of withdrawal or traction, bleeding and inadvertent injury in the buccal branches of the facial nerve may occur. When in doubt, the following maxim must be performed: when the Bichat fat ball is identified, it will appear to be quite mobile and have a stronger yellow and striking appearance, having an "egg yolk" aspect. The Bichat fat ball is encapsulated, tending to "herniate" when it is reached.
The internal visualization of the parotid duct during dissection has not been purposely mentioned so far. Therefore, by following the steps outlined above, there should be no "contact" with this structure, which evidences the safety of the technique described herein in relation to the inadvertent injury of this structure. If the duct is identified internally, the dissection takes place in a lower position and "distancing" of the Bichat fat in a supero-lateral position.
Bichat fat removal with safety and precision - the "broom" technique
Once the Bichat fat has been identified by its strong, yellow, encapsulated mobile characteristic, its anterior portion was immediately pinched using Allis or Halsted forceps. This is because of the fact that it is highly mobile and can move later, making its subsequent hold insecure (Figure 2).
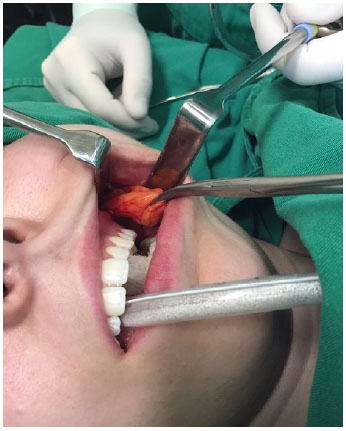
Figure 2. Once the Bichat fat pad is identified by its strong, yellow, encapsulated mobile characteristic, its anterior portion must be immediately pinched using Allis or Halsted forceps.
The technique dubbed "broom" refers to the analogy of sweeping; that is, after grasping the fat, the surgeon passes the Langenbeck retractor to the assistant, holding the fat with his left hand (as if we were sweeping) around the Bichat fat capsule. With light traction, the structure was pulled and "swept" externally; the dissection around the capsule, preferably without breaking it, makes this maneuver quite safe and extinguished (Figure 3).
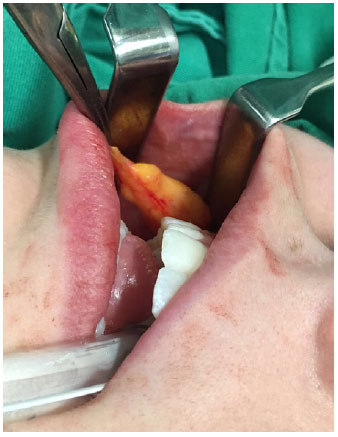
Figure 3. With light traction, the structure is pulled and "swept" externally; dissection around the capsule, preferably without rupturing it, is then performed, making this maneuver quite safe and bloodless.
After full exposure of the oral fat, it can be "freed" from its posterior junctions and fibers by separating these fibrous tissues. We removed approximately 90% of the fat, keeping its posterior portion that was more adhered to the deep structures (Figure 4).

Figure 4. Approximately 90% of the fat is removed, keeping its posterior portion, which is more adhered to the deep structures.
After removal, a hemostasis revision was performed with direct visualization of the cavity with the aid of the Langenbeck retractor. With the technique described above, some expressive bleeding is rare, and when it occurs, we always prefer to use bipolar cautery for hemostasis.
At the end of the procedure, the incision was closed using two to three points of Vicryl 4.0. It is of fundamental importance that these sutures are created in such a manner as to encompass the fibers of the buccinator muscle and the mucous layer with a "generous" thickness, avoiding possible dehiscence of the surgical wound.
These points were maintained for 3 weeks by when, for the most part, they had already fallen naturally.
RESULTS
Twenty-seven patients with a mean age of 32 years were consecutively operated on. In one patient, there was "pronounced edema." A temporary neuropraxia was managed with botulinum toxin application on the contralateral side to reduce the asymmetry, which resolved spontaneously in 2 weeks. There was no need for surgical reintervention owing to the presence of hematoma or other operative site complications.
All patients were very satisfied with the results obtained with the surgery (Figures 5 and 6).

Figure 5. A: Right profile view - preoperative; B: Left profile view - preoperative; C: Left profile view - postoperative; D: Right profile view - postoperative.

Figure 6. A: Left profile view - preoperative; B: Right profile view - preoperative; C: Left profile view - postoperative; D: Right profile view - postoperative.
DISCUSSION
Bichectomy for an aesthetic purpose has been reported for a long time by several authors3,6,7,12,13 and was mainly performed with the aim of fine-tuning the middle third of the face, delineating and enhancing the bone angulations of the zygomatic region, and collaborating for an aesthetic facial appearance7.
There are few studies in the current medical literature describing clearly the technique of intraoral bichectomy, with the main one being the study published by Matarasso in 2006. Despite the precise technical description7, the author did not report its application in a series of cases. Thus, we believe that our report is the first to use the surgical bichectomy technique consistently in a series of cases.
The technique described herein differs from that described by the author in some aspects7, with the main ones being that we do not recommend external pressure for identification of the Bichat fat. We prefer to maintain the intact capsule when possible, which facilitates a more precise removal of the fat, applying traction by removing the inferior fat almost entirely.
An average age of 52 years presented in our series of cases with associated surgeries was shown to be increased as a function of two patients in whom bichectomy was associated with rhytidoplasty (Figure 7). When we considered only the patients who sought bichectomy only for an aesthetic purpose and to diminish the volume of the cheeks and tune the face, the average age was 32 years.

Figure 7. A: Front view - preoperative; B: Right profile view - preoperative; C: Left profile view - postoperative; D: Front view - postoperative; E: Right profile view - postoperative; F: Left profile view - postoperative.
A more complete anatomical study suggests that poor facial ligament development, ligament laxity secondary to facial aging, and/or fatty cushion rupture could cause the Bichat fat to prolapse or fall into the mouth or subcutaneous tissue14.
Despite the difficulty in adequately quantifying the results obtained through satisfaction questionnaires after facial procedures, our perception is that the majority of the patients were very satisfied with the results obtained, considering them to be natural and adequate to their initial expectations. However, objective studies are still needed to quantify and qualify the results obtained after bichectomy.
A fact that should be taken into account, deserving greater attention in future studies, is that in 78% of the patients in our series, bichectomy was associated with other complementary procedures, which may influence the final quality of the result and degree of satisfaction of the patients.
The two authors who described the removal of the aesthetic buccal fatty cushion3,13 emphasize the superiority of the results with associated procedures, ranging from liposuction3 to filling of the malar region with hydroxyapatite granules13. According to Jackson13, buccal fat removal alone can produce virtually imperceptible results even when not correctly indicated. Therefore, further studies are needed to evaluate the results of isolated bichectomy.
In our series of cases, no major complications, such as definitive nerve lesions or large bleeding requiring reintervention or use of electrocautery, were observed, proving the safety of the procedure when performed under adequate conditions, a fact already reported in main studies on removal of the buccal adipose cushion7,13.
We believe that performing the surgery under general anesthesia and in a hospital environment, with adequate visualization of the dissection and blood pressure control in the intraoperative period, also contributes to the safety of bichectomy in our series. Our case series corroborates the claim of Jacksons that "removal of oral fat is virtually free of complications"13.
We highlight some important aspects that contribute to the safety of the technique described above. We do not use scissors or sharp instruments inside the "tunnel." The dissection is performed in a blunt and delicate manner. In this manner, direct injury by transfixation of the buccal branches or the parotid duct, as well as bleeding due to injury to the transverse facial vein or artery, is very unlikely.
CONCLUSION
When the systematized steps of the described technique are precisely followed, intraoral bichectomy can be performed in a predictable and safe manner. However, such a surgery should never be trivialized, always considering the delicate anatomical region where it is performed, as well as its proper indication.
COLLABORATIONS
GSA Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
EJS Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; writing the manuscript or critical review of its contents.
REFERENCES
1. Bradley P. Buccal pad of fat and its applications in oral and maxillofacial surgery: a review of published literature (February) 2004 to (July) 2009. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(2):146. DOI: http://dx.doi.org/10.1016/j.tripleo.2011.01.045
2. Dubin B, Jackson IT, Halim A, Triplett WW, Ferreira M. Anatomy of the buccal fat pad and its clinical significance. Plast Reconstr Surg. 1989;83(2):257-64. PMID: 2911625 DOI: http://dx.doi.org/10.1097/00006534-198902000-00009
3. Guerrerosantos J, Manjarrez-Cortes A. Cheek and neck sculpturing: simultaneous buccal fat pad removal and subcutaneous cheek and neck lipoplasty. Clin Plast Surg. 1989;16(2):343-53. PMID: 2736869
4. Hong Z, Chen Y. Cosmetic surgery of cheek and anatomy buccal fat pad. Zhonghua Zheng Xing Wai Ke Za Zhi. 2000;16(3):180-2.
5. Jackson IT. Anatomy of the buccal fat pad and its clinical significance. Plast Reconstr Surg. 1999;103(7):2059-60. DOI: http://dx.doi.org/10.1097/00006534-199906000-00042
6. Matarasso A. Buccal fat pad excision: aesthetic improvement of the midface. Ann Plast Surg. 1991;26(5):413-8. PMID: 1952712 DOI: http://dx.doi.org/10.1097/00000637-199105000-00001
7. Matarasso A. Managing the buccal fat pad. Aesthet Surg J. 2006;26(3):330-6. PMID: 19338917 DOI: http://dx.doi.org/10.1016/j.asj.2006.03.009
8. Toshihiro Y, Nariai Y, Takamura Y, Yoshimura H, Tobita T, Yoshino A, et al. Applicability of buccal fat pad grafting for oral reconstruction. Int J Oral Maxillofac Surg. 2013;42(5):604-10. DOI: http://dx.doi.org/10.1016/j.ijom.2012.07.009
9. Khiabani K, Keyhan SO, Varedi P, Hemmat S, Razmdideh R, Hoseini E. Buccal fat pad lifting: an alternative open technique for malar augmentation. J Oral Maxillofac Surg. 2014;72(2):403.e1-15. DOI: http://dx.doi.org/10.1016/j.joms.2013.10.002
10. Jung BK, Song SY, Kim SH, Kim YS, Lee WJ, Hong JW, et al. Lateral Oropharyngeal Wall Coverage with Buccinator Myomucosal and Buccal Fat Pad Flaps. Arch Plast Surg. 2015;42(4):453-60. DOI: http://dx.doi.org/10.5999/aps.2015.42.4.453
11. Chia CY, Rovaris DA, Fontana R. Lipoma gigante do coxim adiposo bucal: relato de caso e revisão da literatura. Rev Bras Cir Plást. 2016;31(1):112-7.
12. Newman J. Removal of buccal fat pad by liposuction. Plast Reconstr Surg. 1990;86(2):385-6. DOI: http://dx.doi.org/10.1097/00006534-199008000-00054
13. Jackson IT. Buccal fat pad removal. Aesthet Surg J. 2003;23(6):484-5. PMID: 19336124 DOI: http://dx.doi.org/10.1016/j.asj.2003.08.005
14. Zhang HM, Yan YP, Qi KM, Wang JQ, Liu ZF. Anatomical structure of the buccal fat pad and its clinical adaptations. Plast Reconstr Surg. 2002;109(7):2509-18. DOI: http://dx.doi.org/10.1097/00006534-200206000-00052
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS, Brazil
3. Hospital da Unimed-Nordeste, Caxias do Sul, RS, Brazil
4. Hospital do Círculo, Caxias do Sul, RS, Brazil
5. Hospital Saúde, Caxias do Sul, RS, Brazil
Institution: Hospital São Lucas, Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS, Brazil.
Corresponding author:
Gustavo Steffen Alvarez
Rua Mostardeiro, 5 - 501
Porto Alegre, RS, Brazil - Zip Code 90430-001
E-mail: alvarezplastica@gmail.com
Article received: February 13, 2017.
Article accepted: January 26, 2018.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter