

Original Article - Year 2018 - Volume 33 -
Indications and limits of mammoplasty with "L-scar": 30 years' experience
Indicações e limites da mamoplastia com "cicatriz em L": experiência de 30 anos
ABSTRACT
INTRODUCTION: Studies recommend reducing the size of the scar on mammoplasties to the smallest possible, using L-scars as one of the techniques. However, its use is limited based on the resections of excess skin because of mammary ptosis. The objective of this study is to determine the limitations of L-mammoplasty.
METHODS: To describe the process of breast implantation, mammary lines are used to guide the mammoplasty to achieve anatomically perfect and beautiful breasts. This classifies as "aesthetic pathologies" with quantification of ptosis in centimeters and the limitations being considered in choosing the surgical technique. The proposed classification was used to reduce and model the hypertrophic and ptotic breasts. The suturing maneuvers involved a "semicolon" incision from the lateral side of the submammary groove to the medial and then upward toward point A, terminating in vertical suture, VY, or "areolar circular compensation bag," depending on the excess skin in the periareolar region. This maneuver reduces the extension of the horizontal scar to the maximum of AM plus 2 cm.
RESULTS: When mammary ptosis was less than 7 cm, the results were of good quality, without significant residual ptosis and distortion of the areola, achieving a cone shape.
CONCLUSION: L-mammoplasty is a good technique, but it should be limited to cases with AM flaccidness below 7 cm and good skin quality.
Keywords: Mammaplasty; Breast implantation; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: O autor preconiza redução da dimensão das cicatrizes nas mamoplastias às menores possíveis, utilizando cicatrizes em L como uma das táticas. Estabelece limites no seu uso, baseando as ressecções dos excedentes de pele na medida da ptose mamária. O objetivo é determinar os limites da mamoplastia em L.
MÉTODOS: Descreve a implantação das mamas no tórax, as linhas mamárias guias para qualquer mamoplastia, as mamas anatomicamente perfeitas e bonitas. Classifica o que denomina de "patologias estéticas" das mesmas, a maneira de quantificar a ptose em centímetros e escolhe a tática cirúrgica do L baseado nela, e suas limitações. Como reduzir e modelar as mamas hipertróficas e ptóticas conforme a classificação proposta. As manobras de suturar as incisões em "ponto e vírgula" partindo da lateral do sulco submamário para medial, depois para cima em direção ao ponto A, terminando em sutura vertical, V-Y ou "bolsa areolar de compensação circular", conforme o excedente de pele na região periareolar. Manobra que reduz a extensão da cicatriz horizontal, ao máximo de AM mais 2 cm.
RESULTADOS: Quando a medida da ptose mamária foi menor que 7 cm, os resultados foram de boa qualidade, sem ptose residual importante, sem distorções da aréola e do cone obtido.
CONCLUSÃO: A mamoplastia com cicatriz em L é boa tática, mas deve limitar-se a casos com flacidez de medida AM abaixo de 7 cm e pele de boa qualidade.
Palavras-chave: Mamoplastia; Implante mamário; Procedimentos cirúrgicos reconstrutivos.
In 1990, mammoplasty was described1 with "L-scars," classifying the mammary hypertrophies according to projection and base1-3, making a skin resection marking based on the measurement of ptosis, describing different ways of treating the mammary tissue of each group, and giving them adequate shape and volume and "L-scar."
In mammoplasties, a smaller possible scar is to be obtained without or with minimal flaccidity, with 1/1 continent content relation. The shape and volume of the breast have nothing to do with the extent of the scars. It is obtained independently of the skin; the binomial scar versus form has no meaning. Each breast will have scars compatible and directly proportional to the degree of ptosis, which does not affect the volume removed. Correct diagnosis is necessary in using the appropriate techniques that the scars as small as possible, without residual ptosis, with shape, extension, quality, and adequate positions.
Excessive skin restraints lengthen the horizontal scar. Insufficient resections leave them shorter, with residual ptosis. The exact quantification of the removal of the excess skin is a key point to obtain satisfactory, homogeneous results for each case. Skin quality determines primary and residual flaccidity. Proportional shape, volume, areola-papilla, axillary extensions, and pectoral abutments are other factors necessary for the diagnosis of "esthetic pathologies" to be treated.
Studies described techniques to obtain good results considering forms of skin marking and resection of breast tissue, such as inverted T-mammograms4-9, with vertical10-12 and periareolar scars13-21. Others proposed "L-scars" to remove excess skin1-3,22-28, none of which described the indications and limitations of this technique.
To understand the three-dimensional shape of the breasts, volume, and "esthetic pathologies"3, flaccidity should be quantified to define the extent and possible shape of the final scars of a mammoplasty, indications, and technique with "L-limitations."
OBJECTIVE
To determine the extent of breast ptosis where mammoplasty can be performed with L-scars.
METHODS
The observation period was from 2010 to 2016, in private practice at Base Hospital of São José do Rio Preto, SP, following the principles of the Declaration of Helsinki. All patients signed an informed consent form.
Anatomically perfect breast and classification of breast hypertrophies
Breast implantation in the thorax
In the frontal view of the thorax, we draw a horizontal line joining the anterior axillary folds, obtaining the highest horizontal breast line (HHBL), as far as the upper mammary pole. Another horizontal line joins the two submammary grooves in the meridian of the breast, thus obtaining the lowest horizontal breast line (LHBL) (Figure 1).
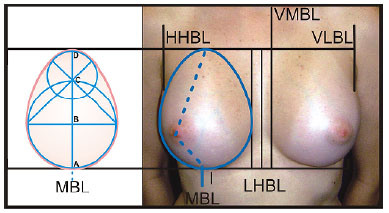
Figure 1. Front view of the anatomically perfect breast.
The vertical lateral breast line (VLBL) descends in the thorax at the anterior axillary fold of each side (anterior axillary), and two vertical lines parallel to the median line, on the external and 1 to 1.5 cm lateral to it (vertical breast meridian line, VMBL), complete two quadrilaterals, where the breasts are implanted in the thorax. Two vertical lines divide each of them, (breast meridian lines, BML). When they cross the lower horizontal mammary line, they determine points I (Figure 1). Breasts with volumes lateral to the VLBL present axillary extensions, medially to MVBL, sinmastia, superolateral horizontal columns.
The projection and position of these quadrilaterals determine the positioning of the breast implant base. Absence of pectoral muscles or excessive lateral curvature of the ribs (pectus carinatum) causes the mammary cone to deviate laterally. Pectus excavatum diverts it medially (Figure 2). Scoliosis tilts this plane anteriorly - anterior to less than normal (18°) and the breasts may appear ptotic.

Figure 2. Pectum excavatum altering the breast implant base and consequent projection.
Knowledge of three-dimensional feature of the perfect breast is necessary and serves as a parameter for surgeons to "copy" the ideal form when dealing with existing "esthetic pathologies."
Frontal view: A good breast is a "golden ovoid," whose lower part touches the LHBL, the upper part with the HHBL, the lateral with the VMBL, and the medial with the MVBL (Figure 1)3. Thus, its vertical diameter is the result of two overlapping circles, determined as 1:1.618 ratio, recognized as Phi (golden or divine) proportion. According to some authors, it stimulates cerebral limbic systems as a pattern of beauty and efficiency3-29.
Lateral view: (Figure 3) the breast resembles a "golden triangle" whose base angle is divided by two that determines on the contralateral side two segments with the ratio Phi between them. This inclined 18º in the sagittal plane, determined by the external bone, Louis angle, and ribs, is similar to the perfect breast3 (Figure 3). From the apex of the cone to the mammary groove on MBL, adequate breast volume and shape measure between 7 and 12 centimeters and from the apex to the HHBL, with 1.6 as the lowest measurement.
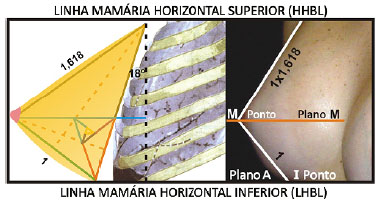
Figure 3. Side view of the perfect breast.
This Phi ratio does not need to be exact to obtain a perfect breast; a 1:1.5 ratio is still beautiful. The measurement varies for each country or people with different concepts of volume, not shape. Larger breasts reach the lines, and smaller ones fall short of them; they may be small or large, but still beautiful in shape. All breasts without flaccidity is above the horizontal plane (A) coincident with the LHBL.
Vertical view: (Figure 4) by joining five golden triangles at the sides, we will obtain a "pentagonal" shape, when turned on its axis makes a "golden cone," similar to the breast seen vertically, when the patient was looking at it3. The surgeon at the end of the operation can the result vertically from top to bottom and vice versa while the patient is still lying at the surgical table.
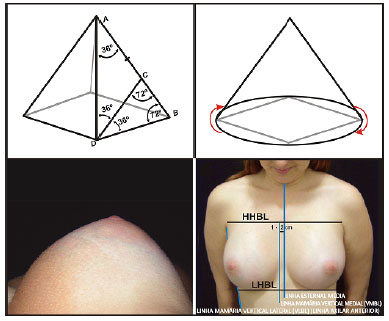
Figure 4. Vertical view of the perfect breast.
Classification of "esthetic pathologies" of the breasts: shape and volume
Group I (GI): Shape and proportions are described. Volume occupying the thoracic base within the four breast lines to be demonstrated in a model (Figure 5).
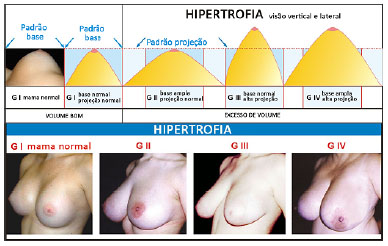
Figure 5. Classification of the hypertrophies by the base and projection of the cone determining "esthetic pathologies" of the breasts.
Group II (GII) hypertrophy: The base exceeds the mammary lines and small projection with excess volume.
Group III (GIII) hypertrophy: The base does not reach the mammary lines, and projection is larger than the GI, with excess volume.
Group IV hypertrophy: It is the sum of GII plus GIII, which is the most common to be operated on. Hypomastia is classified identically and contrarily by the lack of volume and different forms3 (GII-GIII-GIV hypomastia). Post-mastectomy mastitis are of the IVM hypomastia.
Knowledge of the form and volume of "esthetic pathologies" is necessary to plan for surgical treatment. Hence, excess glandular tissues can be removed or added when missing, eliminating attempts at performing unnecessary procedures.
Quantification of ptosis and choice of surgical skin resection techniques
During puberty, the breast grows into the thoracic space, and its volume will increase due hormonal and genetic stimuli (Figure 6A). It will be more or less projected, depending on the variation of skin resistance. Resistant dermis will tend to have breasts of GII and fine dermis of GIII.
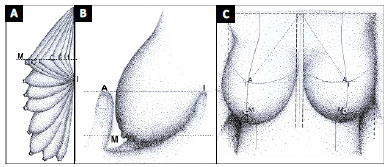
Figure 6. A: Breast growing, projecting into space during evolution in time and bad weather; B: Point I projected on the breast determining point A; C: Front view of points and guide lines.
Initially, the breasts lie above the LHBL and point I; however, the skin or factors (environmental weather, sun, smoke, large weight variations, pregnancy, bariatric surgery, age progression, systemic diseases, volume and mammary forms) reduce their resistance progressively through its apex, passing the LHBL downwards, and then reaching point I (Figure 6A).
It either traipses the areola-papilla complex or not. If the vertical diameter reduces, the horizontal increases, and the upper mammary pole empties. A perfect breast has "vertical" alignment. Point I never changes with the eventual sagging, and it is projected horizontally on the breast, with volume below the LHBL; its meridian determines point A (Pitanguy)4 (Figures 6B and C). The tip of the mammary cone on the meridian determines point M and does not always refer to the papilla, which may be ectopic in relation to it, above, below, lateral, or medially.
The measurement between points A and M quantifies the extent of skin to be removed to correct ptosis above LHBL and point I (Figure 6B). When AM is less than 3 cm, it is possible to perform "vertical mammoplasty" using vertical skin spindle and periareolar resections. With AM between 3 and 7 cm, it is possible to remove excess skin with vertical spindle and lateral hemifusion, called L-mammoplasty. With AM greater than 7 cm, skin resections fall on the vertical and horizontal spindles, or T-mammoplasty. Compared with T-mammoplasty, skin adjustment in L-mammoplasty is more difficult and requires an understanding of the methodology, indications, and limits to obtain satisfactory results.
Surgical technique of L-mammoplasty
Skin marking
HHBL, LHBL, VLBL, VMBL, and BML and points I, A, and M are labeled with the patient standing (Figure 7A, B, C). In the horizontal dorsal decubitus position, with arms abducted at 90º, the flat hand of the surgeon gently pushes the breast and rectifies the BML. With a skin-marking pen and a bidirectional handle, a line is marked from the apex of the breast using the fingers as guide to obtain the AM measurement. A semicircle is drawn at the upper part with a point of rotation in M, passing through A (Figure 8A). From point I, upward, and on the meridian is marked AM. From this end, a medial circle arc is drawn (Figure 8B). From point I to the lateral border of the mammary cone is marked AM horizontally, raising its extremity by 1 to 1.5 cm (Figure 8C).
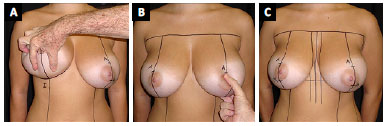
Figure 7. A and B: Point I to point A; C: Point M, greater projection of the cone, ectopic in relation to the papilla. Lines and points obtained with patient standing.
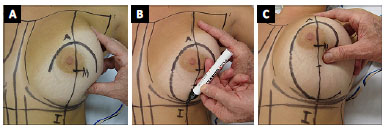
Figure 8. A, B and C: Marking of skin resections based on AM.
Then, determine the base diameter of the new breast by reducing the volume of the breast be operated on. From the horizontal AM going toward point A, pull the breast slightly towards the outer furcula, and an oblique mark is obtained (Figure 9A). In straight lines, the medial and lateral superior and inferior lateral margins are united, obtaining the basic marking of the skin for resection.
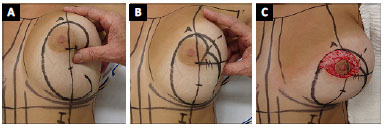
Figure 9. A, B and C: Conclusion of periareolar marking and desepidermization.
During closure, a sub-areolar strangulation is possible, with flattening of this area, which in the long-term disappears at the expense of enlargement of the upper vertical scar. If this can be avoided, "safety triangle" of skin is obtained by marking a horizontal line that passes through point M, forming a 90º angle with BML. At the upper lateral angle, the bisector is traced until it reaches the lateral marking. From it, it stretched toward point M marked at 1.5 to 2 cm with two curved lines, joining this point to the lateral marking (Figure 9B).
Breast Cone Modeling
The breast cone model was made according to hypertrophy classification. The periareolar area is cleared (Figure 9C). In GIV, glandular resection is performed at the ptotic part, which will be below point I with the patient standing (Figures 10A-B and 11A), accompanying the skin marking of the lateral and medial slopes. Whether considered together or not, the wedge is dries by reducing the lateral-lateral diameter of the cone (Figures 10B and 11A). Then, the medial base (Figure 11B-C) and lateral colonnades (Figure 11D) are reduced, thereby reducing the projection. A lower mini-flap is always preserved at point I to recompose the lower pole by rounding it (Figure 11C), even with raising of arms. The lateral and medial colonnades are sutured with stitches necessary to structure the breast, before suturing the skin. The uppermost point of the proximal base of the HHBL is fixed together with the aponeurosis of the pectoralis muscle, preventing upper lateral slippage of the breast.
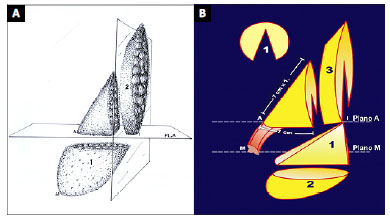
Figure 10. A and B: Scheme of GIV breast tissue removals. (1) wedge reducing the lateral-lateral diameter, (2) ptosed volume, (3) resection of the base reducing projection. The rest are shape, volume, and proportions that fit within the mammary lines and the areolar pedicle.
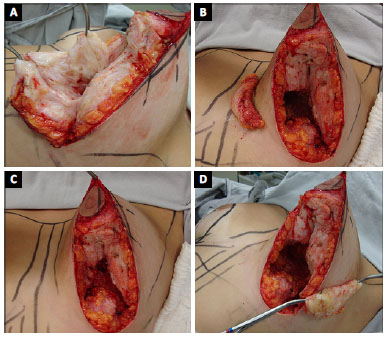
Figure 11. A: Resection of ptosis and wedge (GIV), or leaving it all or part as a lower pedicle flap (GI); B: Medial base resection (GIII and GIV); C: Lower pedicle miniflap left in GII, GIII, and GIV; D: Lateral base resection (GIII and GIV).
If the areolar pedicle is long and thick, the suture of the colonnades should not be made to its end so that it enters between them ("intussusception") and does not hinder its ascent to point A. In these case, the tip of the cone becomes more rounded.
In GI, the shape was altered by flaccidity, the vertical and horizontal axes were inverted, the first reduced, the second increased, and the upper pole was emptied. The breast has become horizontal. To correct the shape, a lower pedicle flap is made containing the central part of the volume that passed below the LHBL and point I (Figures 10B and 11A). The vertical central portion of the breast is withdrawn at its meridian, and this flap is vertically sutured to the aponeurosis of the pectoral muscle, attempting to reach the HHBL. The lateral and medial colonnades are sutured together on this flap, completing the formation of the mammary cone. The vertical and horizontal axes are corrected, and the upper pole is filled30. This flap may have its skin removed; its vascular pedicle is axial from the intercostal space above point I.
In GII, the base of the breast is enlarged, and a vertical wedge is removed accompanying the mammary meridian, from point I to where necessary for convenient reduction of the lateral-lateral diameter (Figure 10B). When necessary, the ptosed volume below point I is removed together with the wedge. This process like doing the GI flap but resecting it. The lateral and medial colonnades should be detached from the thorax and sutured together, thereby increasing their projection.
In GIII, the breast projection is increased, and resections of the excess volume are done by resection of the base of the lateral and medial colonnades (Figures 11B-D). The subcutaneous of the resected areas should be preserved at the same thickness of the subcutaneous tissue of the underlying thorax. In small GIII hypertrophies, instead of amputating the base, the inverted wedge is inverted with a subareolar base, and the end of the base only touches the pectoral aponeurosis. Even in large hypertrophies of this group or GIV, this inverted wedge6 improves the rise of the areola to its new position and leaves the breast more conical when suturing the colonnades to each other.
Skin suture
Suturing starts from lateral to medial at the angle formed by the horizontal and oblique AM, confronting the two skin incisions up to point I, or slightly more medial (Figure 12A). Thus, the vertical slopes of the incisions should be adjusted with the suture starting from point I upward toward point A. As the medial slope is longer than the lateral slope (Figure 12A), the maneuver of adjusting them is to take the points of suture in the medial aspect as a line parallel to the incision and in the lateral aspect as point, that is, "point and comma suture" (Figure 12B).
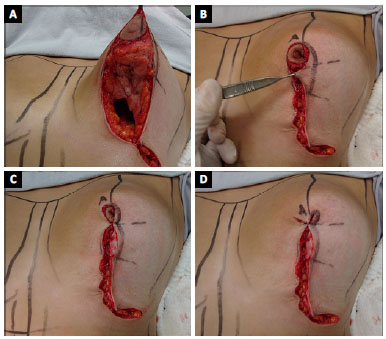
Figure 12. A: Beginning of lateral to medial suture; B: From point I to the areolar region in "semicolon" with of the safety triangle of the skin; C: Termination in vertical suture; D: V-Y.
The difference between the extension of the medial skin and the lateral one determines the limitation of L-mammoplasty. It is not appropriate to compensate with an AM measurement above 7 cm.
With the vertical suture approaching the subareolar region, the need to use the "safety triangle" of peleno adjustment is evaluated by resecting part of it above, below, or totally (Figure 12B).
At the end of the cone, there may be variable skin excess, which will define the type of finalization in the periareolar region. Without the excess skin, the areolar site is demarcated with the open-topped area. In minimal quantity, the vertical suture continues until the end of the de-epidermized area (Figure 12C), small excess ends in V-Y (Figure 12D). If it is medium or large, it concludes with either a closed "circular areolar" bag or not (Figure 13A). The areolar site is sutured (Figure 13B): vertical suture, or VY, or the pouch is removed, and the marked area is de-epidermized, and the areola is sutured to the new site with intradermal points including the subareolar muscle (Figure 13C).

Figure 13. A: Termination in closed "areolar circular compensation bag," with large skin excess; B: Areolar site marking; C: Sutures completed, maximum horizontal scar equal to AM+2 cm, vertical equal to the height of the mammary cone.
Before the skin sutures are made, the subcutaneous strands are sutured, compensating them in the same way as the skin ("point and comma"), facilitating and undoing tensions that widen scars, thereby improving the resulting form.
The flattened hand pushes the breast in the cranial-caudal direction and corrects the position of the lateral horizontal incision upward toward the glandular border, slightly elongating that incision and scar. The L-mammoplasty described will have a horizontal scar at the maximum of AM plus 2 cm (Figure 13C).
RESULTS
The results obtained, with the mammary ptosis smaller than AM-7 cm, were of good quality without distortion of the mammary cone or the areola and little or no residual ptosis (Figures 14, 15 and 16). By contrast, cases of AM ptosis greater than 7 cm showed difficulties in adjusting the lateral and medial slopes of the vertical incisions and late results, leaving residual ptosis, periareolar skinfolds, distortions of the mammary cone, and horizontal scars surpassing the side of the line anterior axillary. In private practice, in the last 100 cases operated on, 59% concluded the operation with L-scars. In the University Hospital of São José do Rio Preto, in the last 50 cases, 18% was concluded with L-scars.

Figure 14. Front an oblique and profiles at pre- and postoperative GIV mammoplasty.
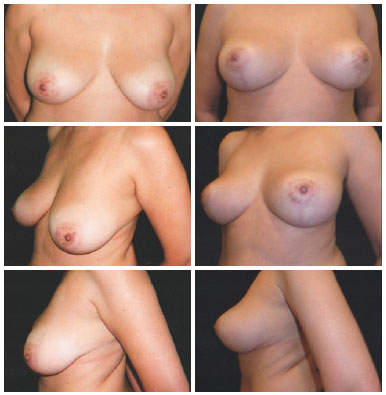
Figure 15. Front and oblique profiles and pre- and postoperative GIV mammoplasty

Figure 16. Front and right oblique and profiles of unilateral mammoplasty copying the contralateral breast.
DISCUSSION
In cases of GII, GIII, and GIV, the small flap of the inferior pedicle at point I recomposes the lower pole of the breast, reduces its slip towards the point I, and consequently emptying the upper pole, inverting the vertical and horizontal diameters of the base and illusionary elevation of the areola. It is the breast scale, which is lower than the lower pole and empties higher.
The intention is to make a perfect cone, structured with sutures of the mammary tissue, before the closure of the skin, in the described three-dimensional proportions, adequate volume, and within the four breast lines. These breasts will never change their shape in the future, only progressive sagging by the aging of the skin.
By attempting to use L-mammoplasty beyond the limits proposed by this technique, instead of achieving shorter scars, the results may be inadequate, with distortions of shape, areolae, and residual flaccidity. Using techniques that obtained L-scars, with the horizontal line going beyond the VLBL, leave the scars visible and of poor quality. The movements of the upper limbs enlarge them, even at rest for months.
Maintenance of the subcutaneous thickness of the thorax underlying the breast tissue resections of the base preserves vessels and main nerves, thereby avoiding vascular and sensitivity changes. The breast is ectodermal.
Achieving and maintaining a cone of ideal proportions described is a difficult task. The spatially designed breast needs rugged skin and consistent breast tissue for maintainability, without sagging. The tendency is to empty the upper pole and rounded base. However, appropriate skin-independent modeling keeps the long-term results, without distortion of shape. Breasts with a predominance of fatty tissue do not retain their shape in the long run.
Sometimes, small incisions are necessary in the lateral de-epidermal dermis or medial to the areola, facilitating elevation to its new site. The narrower side of the de-epidermization should be the chosen one.
Areolar suture, vertical suture, or V-Y suture should not be performed under excessive skin tension; it should be distributed naturally with medium traction. Compensations from the lateral to medial and from there to the apex of the cone is called inverse skin compensation, consuming it in several small periareolar "ears", without lengthening the scars. It also facilitates the elevation of the areola, without complementary procedures. In case of horizontal and vertical sutures, there may be a small pleating of the skin on the medial side, which disappears in 60 days.
The greater the volume removed, the more extensible and flaccid the skin is, and the more difficult the compensations will be using the L-mammoplasty, even with AM measurement less than 7 cm. This technique requires experience in handling them between the vertical incision of the skin strands. The final extension of the scars of the submammary sulcus is directly proportional to the amount of ptosis and minimally to the volume removed.
With the parameters defined, it is possible to calculate and mark the maximum extension of the horizontal scar, that is, AM plus 2 cm.
CONCLUSION
Mammoplasty with L-scars is a good technique, which is limited to cases with an AM measurement smaller than 7 cm and requires greater care in skin adjustments.
COLLABORATIONS
ARB Analysis and/or interpretation of data.
ACB Analysis and/or interpretation of data.
REFERENCES
1. Bozola AR. Breast reduction with short L scar. Plast Reconstr Surg. 1990;85(5):728-38. DOI: http://dx.doi.org/10.1097/00006534-199005000-00013
2. Bozola AR. Reduction Mammaplasty: Preferred Techniques. In: Goldwyn RM. Reduction Mammaplasty. Boston: Litlle Brown; 1990. p. 407-37.
3. Bozola AR, Longato FM, Bozola AP. Análise geométrica da forma da beleza da mama e da forma de prótese baseado na proporção Phi: aplicação prática. Rev Bras Cir Plást. 2011;26(1):94-103. DOI: http://dx.doi.org/10.1590/S1983-51752011000100019
4. Pitanguy I. Mammaplastias. Rev Latinoam Cir Plast. 1963;7:139.
5. Pontes R. A technique of reduction mammaplasty. Br J Plast Surg. 1973;26(4):365-70. PMID: 4759977 DOI: http://dx.doi.org/10.1016/S0007-1226(73)90042-8
6. Lima JC. Breast Reduction: New Method and refinements. In: Transactions of the Seventh International Congress of Plastic Reconstrutive Surgery; 1979 May 20-25; Rio de Janeiro, RJ, Brasil. 1979. p. 518-21.
7. Peixoto G. Reduction mammaplasty: a personal technique. Plast Reconstr Surg. 1980;65(2):217-26. DOI: http://dx.doi.org/10.1097/00006534-198002000-00015
8. Strombeck JO. Mammaplasty: report of a new technique based on the two-pedicle procedure. Br J Plast Surg. 1960;13:79-90. PMID: 13835285 DOI: http://dx.doi.org/10.1016/S0007-1226(60)80014-8
9. McKissock PC. Correction of Macromastia by the Bipedicle Vertical Dermal Flap. In: Goldwyn RM, ed. Plastic and Reconstructive Surgery of the Breast. Boston: Litlle Brown; 1976. p. 215-29.
10. Ariê G. Una nueva técnica de mastoplastia. Rev Latinoam Cir Plast. 1957;3:23-31.
11. Ribeiro L. The Lozenghe Technique. In: Goldwyn RM, ed. Reduction Mammaplasty. Boston: Little Brown; 1990.
12. Bozola AR. Mamoplastia - técnica de Ariè invertida (nota prévia). In: Anais da 1 Jornada Sul Brasileira de Cirurgia Plástica. Florianópolis; 1984. p.157-60.
13. Andrews JM, Yshizuki MM, Martins DM, Ramos RR. An areolar approach to reduction mammaplasty. Br J Plast Surg. 1975;28(3):166-70. PMID: 1191858 DOI: http://dx.doi.org/10.1016/0007-1226(75)90122-8
14. Martins PDE. Mamaplastia periareolar com transposição de retalhos. Rev Soc Bras Cir Plast. 1986;6:1-10.
15. Benelli L. A new periareolar mammaplasty: the "round block" technique. Aesthetic Plast Surg. 1990;14(2):93-100. PMID: 2185619 DOI: http://dx.doi.org/10.1007/BF01578332
16. Bustos RA. Periareolar mammaplasty with silicone supporting lamina. Plast Reconstr Surg. 1992;89(4):646-57. DOI: http://dx.doi.org/10.1097/00006534-199204000-00008
17. Góes JC. Periareolar mammaplasty: double skin technique with application of polyglactine or mixed mesh. Plast Reconstr Surg. 1996;97(5):959-68. PMID: 8618999
18. Aboudib JH Jr, Cardoso de Castro C. Mammaplasty utilizing the periareolar approach. Aesthetic Plast Surg. 1998;22(1):51-7. DOI: http://dx.doi.org/10.1007/s002669900166
19. Ribeiro L, Canzi W, Buss A Jr, Accorsi A Jr. Tuberous breast: a new approach. Plast Reconstr Surg. 1998;101(1):42-50. DOI: http://dx.doi.org/10.1097/00006534-199801000-00008
20. Fayman MS, Potgieter E, Becker PJ. Outcome study: periareolar mammaplasty patients' perspective. Plast Reconstr Surg. 2003;111(2):676-84. DOI: http://dx.doi.org/10.1097/01.PRS.0000041391.44262.E2
21. Bozola AR. Periareolar breast reduction. Aesthetic Plast Surg. 2009;33(2):228-34. PMID: 19123019 DOI: http://dx.doi.org/10.1007/s00266-008-9296-6
22. Horibe K, Spina V, Lodovici O. Mammaplastia redutora: Nuevo abordaje del metodo lateral-obliquo. Rev Latino Am Cir Plast. 1956;2:7.
23. Dufourmentel C, Mouly R. Plastie mammaire par la méthode oblique. Ann Chir Plast. 1961;6(1):45-58.
24. Elbaz JS, Verheecke G. La cicatrice en L dans le plasties mammaires. Ann Chir Plast. 1972;17(4):283-8.
25. Meyer R, Kesselring UR. Reduction mammaplasty with an L-shaped suture line. Development of different techniques. Plast Reconstr Surg. 1975;55(2):139-48. PMID: 1090944 DOI: http://dx.doi.org/10.1097/00006534-197502000-00002
26. Regnault PCI. Reduction Mammaplasty by B Technique. In: Goldwyn RM, ed. Plastic and Reconstructive Surgery of the Breast. Boston: Little Brown; 1976. p. 269-83.
27. Sepúlveda A. Assimetria mamária: tratamento cirúrgico. Rev Bras Cir. 1981;71(1):11-8.
28. Chiari Júnior A. The L short-scar mammaplasty: a new approach. Plast Reconstr Surg. 1992;90(2):233-46. DOI: http://dx.doi.org/10.1097/00006534-199290020-00011
29. Ricketts RM. The biologic significance of the divine proportion and Fibonacci series. Am J Orthod. 1982;81(5):351-70. PMID: 6960724 DOI: http://dx.doi.org/10.1016/0002-9416(82)90073-2
30. Ribeiro L, Accorsi A Jr, Buss A, Marcal-Pessoa M. Creation and evolution of 30 years of the inferior pedicle in reduction mammaplasties. Plast Reconstr Surg. 2002;110(3):960-70. PMID: 12172167 DOI: http://dx.doi.org/10.1097/00006534-200209010-00038
Faculdade de Medicina de São José do Rio Preto, São José do Rio Preto, SP, Brazil
Institution: Faculdade de Medicina de São José do Rio Preto, São José do Rio Preto, SP, Brazil.
Corresponding author:
Antonio Roberto Bozola
Av. Brigadeiro Faria Lima, 5416 - Vila São Pedro
São José do Rio Preto, SP, Brazil - Zip Code 15090-000
E-mail: ceplastica@hotmail.com
Article received: July 20, 2017.
Article accepted: October 11, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter