

Articles - Year 2002 - Volume 17 -
Ultrasound-Assisted Liposuction - 348 Cases Analyzed
Lipoaspiração Ultra-sônica - Análise de 348 Casos
ABSTRACT
The authors report their experience in using ultrasound-assisted liposuction in 348 patients in the period between October 1998 and July 2001. The application of ultrasound brought additional benefits to results, such as improved skin accommodation and the treatment of difficult cases, such as, gynecomasty, dorsum and secondary liposuction. The technique was performed in three stages: super-wet infiltration (l.35:1), followed by ultrasound-assisted liposuction and conventional liposuction. The equipment used was a Lisonix 2000 generator at the setting of 5, that is, 50% of the device's power; which proved to be the setting that causes the least secondary effects, such as tissue fibrosis and seroma. This study also considers the history of ultrasound assisted liposuction and focuses on the physical aspects of ultrasound, with a review on the literature on the use of the ultrasound technique.
Keywords: Liposuction; ultrasound; body contour
RESUMO
Os autores mostram a experiência da utilização da lipoaspiração ultra-sônica em 348 pacientes no período de outubro de 1998 a julho de 2001. A aplicação do ultra-som trouxe benefícios adicionais aos resultados, como melhor acomodação da pele e tratamento de áreas difíceis, como ginecomastia, dorso e lipoaspiração secundária. A técnica utilizada em três estágios consistiu de infiltração super-úmida (1,35:1), seguida da lipoaspiração ultra-sônica e lipoaspiração convencional. O equipamento Lisonix 2000 foi utilizado numa amplitude de 5, ou seja, 50% da potência do aparelho, que demonstrou ser a que menor efeito secundário causa, como fibrose tecidual e seroma. São considerados no artigo o histórico da lipoaspiração ultra-sônica e um enfoque na física do ultra-som, com revisão da literatura relacionada à aplicação da técnica ultra-sônica.
Palavras-chave: Lipoaspiração; ultra-sônica; contorno corporal
The development of modern liposuction radically changed plastic surgery as it enabled the removal of localized fat through small incisions. The techniques and the use of traditional liposuction have improved through the introduction of thinner tubes, the use subdermal infiltration, and intermediate and superficial liposuction techniques. The developments of liposuction revolutionized the resulting body contour. From the beginning, when Fischer(1) first described liposuction in 1976, and then later, when Illouz(2) popularized it, it has been possible to follow the birth and growth of a technique that is renowned today.
With technological development, liposuction started to use other methods to remove fat. In 1987, Grippaudo(3) described the first ultrasound-assisted liposuction; then, in 1988 Zocchi(4)improved the technique, and, in 1989, Gasperoni(5) created percutaneous liposuction.
It is worth emphasizing the role wet solutions have played in the progress of liposuction, both in conventional and ultrasound liposuction. In 1983, in the early days liposuction, Fournier(6) used to use the dry method, i.e., without any subdermal infiltration. In 1980, Yves-Gerard Illouz(2), the predecessor of modern liposuction, introduced the use of blunt-tip tubes and the use of infiltration with hialuronidase. The super-wet infiltration technique, i.e., the use of 1.5 ml of solution for every 1 ml fat aspirate was used as of 1986, thanks to the papers published by Fodor(7).
In 1993, Klein(8) suggested the tumescent infiltration technique, consisting of large infiltration of the subdermal tissue, which greatly facilitated liposuction. The ratio infiltrated liquid / aspirated liquid may be summarized in the following manner: dry liposuction = 0/1; wet = l/1; super-wet = 1.5/1; tumescent > 2/1. In that manner, liposuction became a safe and effective procedure. However, the treatment of fibrous cases, such as in the dorsum, gynecomasty and secondary liposuction may beco me difficult with conventional liposuction(9,10).
Ultrasound was first used for liposuction by Kloehn(11), in 1990, with solid cannula. It was reintroduced later in 1996 by Zocchi(12), using hollow tubes for suction.
The ultrasound lipoaspirator involves the displacement of electric power as high frequency sound waves, which are transformed by a hand-piece into mechanical vibration. These mechanical oscillations travel through a titanium cannula that releases the waves on its tip.
The main biological effects of ultrasound are:
Micromechanic effect: the damage produced directly by the unidirectional action of the ultrasonic waves on intracellular organic molecules. These effects are minimal(13).
Cavitation effect: the cavitational mechanism causes significant cellular fragmentation and diffuses the fat matrix into the intercellular space (14).
Thermal effect: caused by acoustic waves, by the friction of the cannula and also by the conversion of ultrasonic waves into heat by the tissues. It should be dissipated by tissue infiltration (12).
The main change in the second generation of equipment was the introduction of hollow cannulas. Both types are made of titanium for greater efficiency in the transmission of energy(15). The advantages of solid tubes include greater cavitation efficiency, because they allow the permanence of the liquid media created by the infiltration, as described by Zocchi(12). Solid tubes seem to cause less trauma, and to last longer. Their disadvantages include a longer learning curve due to the difficulty for the surgeon to assess the efficacy of the ultrasound in the treated areas and the longer surgical time, as all the resulting contents have to be aspirated in a second phase(9). Hollow tubes, on the other hand, require a shorter learning period and shorter surgeries, as all the content resulting from the cavitation may be aspirated through the tube lumen, thus providing the surgeon with visual feedback of the quantity that is being aspirated from each area(16,17).
MATERIAL AND METHODS
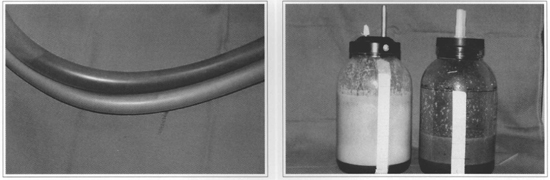
A total of 348 patients underwent ultrasound-assisted liposuction in the period ranging from October 1998 to July 2001. The equipment utilized was Lisonix 2000. This device consists of a generator, a hand piece and the ultrasound cannulas for liposuction (Figs. 1 and 2). The generator converts standard electrical voltage into high frequency power or high voltage signals. These signals are then converted into mechanical vibration at ultrasonic frequency. The power generated by the tip of the cannula causes the fat cells to break down in a process called cavitation(18).

Fig. 1 - Hand-piece of the ultrasound liposuction device.

Fig. 2 - Ultrasound liposuction cannulas.
Ultrasound-assisted liposuction was indicated for patients who presented local fat areas, such as the dorsum, upper and lower abdomen, flanks, thighs, buttocks, arms, and gynecomasty(l9,20,21). Standing patients were marked with circles that identified the areas of greater fat accumulation, deformities and asymmetries.
Of the 348 patients operated on, 97% received epidural anesthesia with sedation and 3% received additional general anesthesia. In 80% of the cases, epidural anesthesia was given between T6 and T12, when the liposuction included the dorsal region, and in 20% of the cases between L1 and L4. Patients were hydrated with 500 ml per hour, and did not need hypervolemic reposition(22,23).
The technique used was three-stage liposuction: infiltration, ultrasound-assisted liposuction, and evacuation through conventional liposuction.
Stage 1: Infiltration with isotonic saline solution with adrenaline 1:500,000 at subdermal level. We currently use the super-wet infiltration method, i.e., 1.35 ml of infiltrated liquid for 1 ml of aspirated liquido. All volumes were recorded for similar infiltration in similar areas. We waited for about 10 minutes for the vasoconstrictive effect of adrenaline.
Stage 2: Making the incisions for the ultrasound liposuction, which are about 3 to 4 mm larger than those used in conventional liposuction. They should be located in such a way so as to allow the treatment of multiple are as through the same incision and in not so apparent places. After the incision, a protector was inserted and wet pads were placed around the site of access in order to avoid skin burns (Fig. 3).

Fig. 3 - During the procedure, protecting the skin with pads.
Figs. 4 and 5 - Difference in bleeding after ultrasound-assisted liposuction and conventional liposuction.
The technique was performed with a Lisonix 2000 generator, with tubes 32 cm long, 3.0 mm in diameter and golf-type tip for deep liposuction and Roma or Bala tips for superficial liposuction(5) (Fig. 2) In the first 6 months the technique was performed at power settings of 5 and 6. As we gained experience, we started to use settings 8 and 9. We noted a greater number of complications and then the setting was lowered to 5(24).
Ultrasound removes fat differently from conventional liposuction. It removes fat through a process called cavitation, which consists of the implosion of adipose cells, or lysis, and emulsification(4,25). The emulsified fat is then removed by the tube. There are two key procedures to prevent thermal injuries. Firstly, ultrasonic energy should be applied only in a wet environment, i.e., after appropriate subdermal infiltration. Gingrass and Kenkel(26) reported temperatures as high as 50 Co in experimental models without infiltration on the subdermal tissue(21,26). Secondly, it is necessary to keep the cannula in constant movement. The repetitive contact of the tip of the cannula with the skin may cause thermal injury, which will manifest itself as erythema, followed by vesicles and finally a lesion affecting the full thickness of the skin, with deformities and scars. The non-dominant hand should be constantly touching the skin to feel the position of the tip of the cannula, which should never be pinched or pressed while the ultrasound is working.
The key elements in defining the completion of the treatment with the ultrasound are the loss of resistance of the tissue to the movement of the cannula and the presence of greater amounts of blood in the aspirated liquid(27). Treatment time and removed volume are also secondarily assessed.
Stage 3: Evacuation with conventional liposuction and final contour. The remaining liquid content was aspirated with 3 or 3.5 mm tubes. It was then that asymmetries, deformities, and bulging areas were treated. Once the emulsion was created, it was removed, as free fatty acids are highly irritant, and may increase the chances of postoperative seroma and inflammation unless they are withdrawn (26). After the end of conventional liposuction, ultrasound liposuction should not be used. After shaping the final contour and pinching the skin fold to evaluate the treated areas, we closed the incisions, with absorbable sutures at the subdermal layer, and non absorbable ones on the skin. A pad dressing was made with bandages and cotton wadding, which was replaced after 24 hours by an elastic garment. Patients were free to exercise after a week, when they were referred for lymphatic drainage.
RESULTS
348 patients (330 women and 18 men) underwent ultrasound-assisted liposuction between October 1998 and July 2001. At the beginning liposuction was indicated for those who needed to have large volumes removed. However, as the technique improved, it started to be used for all the cases referred to liposuction, except for small primary areas. In the cases we studied, the relation infiltrated volume / aspirated volume in the first 3 months was on average 6,350 ml / 3,156 ml, and the ratio infiltrated volume / aspirated volume was 2.01 ml for 1 ml. In the other 7 months, the average changed to 3,009 ml / 2,237 ml, i.e. 1.35 ml for 1 ml, a ratio that remained unchanged in the following months. The tumescent method was used initially for infiltration, i.e., 2 to 3 ml of infiltrated liquid for 1 ml of aspirated liquid. As the technique evolved and we gained confidence, we started to use super-wet infiltration, i.e., more than 1 ml of infiltrated liquid for 1 ml of aspirated liquid. We noted that there was no difference in relation to blood loss or to difticulty in aspiration(22). Quite to the contrary, postoperative edemas became smaller when the super-wet method was used. The total aspirated volume, adding the ultrasound liposuction to conventional liposuction, ranged from 440 to 6,500 ml. The average total volume aspirated by ultrasound-assisted liposuction was 1,245 ml and the average total volume aspirated by conventional liposuction was 1,277 ml.
The average percentage of supernatant liquid, i.e., fat in relation to infranatant, was 75% for ultrasound assisted liposuction and 63% for conventional liposuction.
The areas treated by this method were abdomen (n= 185), dorsum (n=372), flanks (n=536), buttocks (n=250), inner thighs (n=322), arms (n=86), axilla (n=82), knees (n= 138), and gynecomasty (n= 16), where n = number of treated areas, two areas added per bilateral procedure, except for the abdomen (Chart 1).

Chart 1 - Shows the number of areas treated by ultrasound-assisted liposuction + conventional liposuction.
Table I shows the list of treated areas, considering two areas for each bilateral procedure, average ultrasound aspiration time, average infiltration volume and volumes removed by ultrasound-assisted liposuction and by conventional liposuction for each side (except for abdomen).

During the initial months, settings 4 and 5 were used, which meant that the cannula moved at a low speed during the procedure. After one year and based on the studies by Tebbets(24), we started to use setting 8 with the aim of reducing surgical time and possibly using quicker movements during ultrasound-assisted liposuction. We observed an increase in the incidence of pain in the immediate postoperative period, edemas, seromas and fibrosis in the lipoaspirated areas. After using these parameters for 6 months, we went back to lower settings, 5 and 6, which significantly reduced these complications. Whenever ultrasound assisted liposuction was used, it was followed by conventional liposuction. We noticed improvements in body contour after using ultrasound-assisted liposuction as compared to conventional liposuction only. There were very few complications: 12 cases of seroma that required aspiration with syringes and only three cases of superficial burns around the incisions (Figs. 6 to 17).
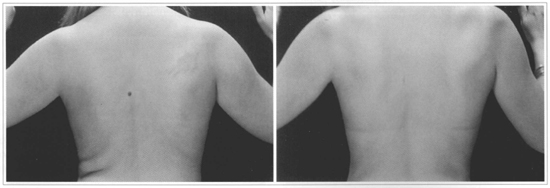
Figs. 6 and 7 - 37-year-old patient who underwent dorsum ultrasound-assisted Liposuction. Pre and 1 year and a half postoperative period.
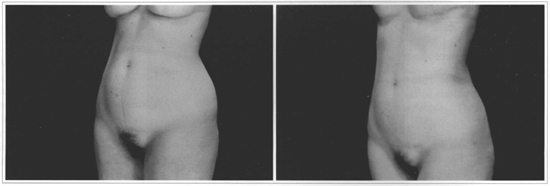
Figs. 8 and 9 - 47 -year-old patient who underwent ultrasound-assisted liposuction on the abdomen and flanks. Pre and 2 years and a half postoperative period.
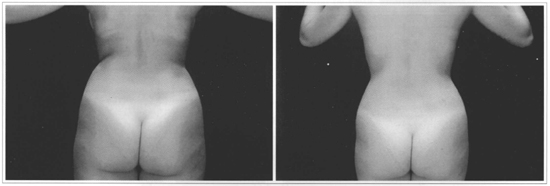
Figs. 10 and 11 - 19 -year-old patient who underwent ultrasound-assisted liposuction on the dorsum and flanks. Pre and 1 year and a half postoperative period.
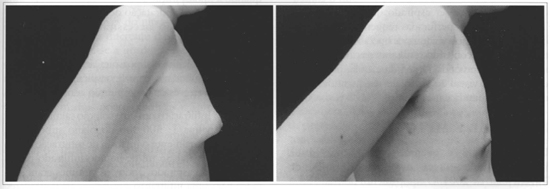
Figs. 12 and 13 - 17 -year-old patient with bilateral gynecomasty. Profile pictures. Pre and 6 months postoperative period.
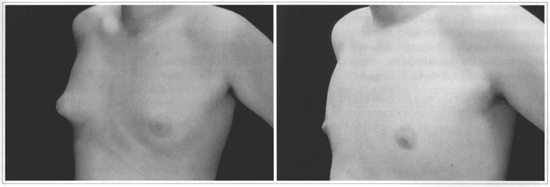
Figs. 14 and 15 - 17 -year-old patient with bilateral gynecomasty. Semi-profile pictures. Pre and 6 months postoperative period.
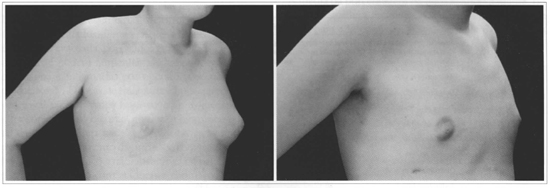
Figs. 16 and 17 - 17 -year-old patient with bilateral gynecomasty. R and L profile and semi-profile pictures. Pre and 6 months postoperative period.
DISCUSSION
Liposuction is one of the methods most widely used by plastic surgeons, and the significant improvement in scientific publications has strengthened the foundations of this technique. The advent of ultrasound assisted liposuction quickly gave rise to countless studies, and today it is used worldwide, with safe and predictable results. The publication of our experience with this method contributes further to the extensive literature by adding our personal approach in the use of the technique.
One of the key factors differentiating ultrasound-assisted liposuction from other liposuction methods is a change in the final level of the postoperative hematocrit. Hetter(28) reports the reduction of one hematocrit degree for every 150 ml of aspirated fat in conventional liposuction; Lewis - 1 degree/300 ml of aspirated fat in liposuction with syringes; Klein/ Hunstad - 1 degree /600 ml in liposuction with infiltration; and this author (Zocchi) found 1 degree / 1,400 ml of aspirated fat in ultrasound liposuction.
In ultrasound-assisted liposuction blood vessels are better preserved and, consequently, there is a smalier decrease in hematocrit levels. Another positive aspect of this technique is the possibility of greater skin retraction in the treated areas, as the increase in local temperature stimulates collagen contraction. Zocchi(4) reports that superficial ultrasound-assisted liposuction may provide up to 40% more skin contraction as compared to other methods.
Another limiting factor, which often prevents the use of ultrasound, is its thermal effects on the skin, vessels and nerves. Howard and Rohrich(29), in 1999, studied the effects of ultrasound at top settings on the sciatic nerve of test animals. The target areas did not suffer any late functional losses at any level of the range. In our experience, we have noticed greater rates of complications when the generator is used at settings 8 and 9, as previously described.
Trott et al., in 1999(30), studied sensorial changes and observed that hypoesthesia was transitory, and longer for the patients who were exposed longer to ultrasound. Maxwell et al.(l7), in 1998, studied the temperature of tis sues during ultrasound application, in a very interesting protocol with sophisticated temperature evaluation devices. They concluded that the method is safe when used within the previous tissue infiltration standards and when the carmula is continually moved. We observed that seroma rates were higher with tumescent infiltration than with the wet infiltration we currently use.
Rohrich et al.(31),in 2000, studied post-liposuction cellular rupture (internal ultrasound - 70 to 90%, conventional - 5 to 25% and external ultrasound- 5 to 20%) using creatinine kinase as a marker. It was 30% greater in ultrasound-assisted liposuction than in conventional liposuction.
Another interesting factor in the development of ultrasound- assisted liposuction is the formation of free H202 in the treated areas, which acts as a bactericide and reduces the chances of infection.
In this study, we were able to observe the uniformity of infiltrated and aspirated volumes, whether by ultrasound-assisted liposuction or conventional liposuction, in all treated areas. Average ultrasound time per treated area was also uniform. The sum of those factors may have led to linear and satisfactory results in the treated patients. Two aspects should be taken into account in relation to the final point of liposuction. The first is the facility with which the ultrasound cannula slides through the tissues and then, when there is no further resistance, this is one of the indications that the final point has been reached(32). One should also note that, if the ultrasound is at a high setting, it is necessary to move the cannula more rapidly. We could, nonetheless, note that intermediate settings are safer and cause less fibrosis and fewer seromas.
We also observed lower incidences of hematomas in the immediate postoperative period, which is explained by the fact that vessels remain untouched during the procedure (Figs. 4 and 5), thus making it possible for patients to resume their regular activities sooner, including physical exercises after the first week.
Ultrasound-assisted liposuction has provided excellent results in cases in which conventional liposuction presents limitations, such as areas of greater fibrosis (secondary liposuction) and in areas such as the dorsum or in gynecomasty.
During the first year we used ultrasound-assisted liposuction, there were 12 cases of seroma. That was explained by the use of tumescent infiltration in the first cases. When we started using super-wet infiltration, we noted a reduction in edemas and seromas.
We also observed that after using higher settings, such as 8 and 9, the rate of seromas, edemas and fibrosis also increased, which made us take the settings back to 5 ar 6.
The disadvantages of using ultrasound-assisted liposuction are longer surgical times and the need to train the surgeon on how to use the technigue and the device. Moreover, the regression of the edema and of the areas of fibrosis reguires longer postoperative lymphatic drainage. In spite of those shortcomings, we observed that there were considerable improvements in long-term postoperative body contour (6 months), when compared to the results of conventional liposuction alone. The positive results were probably due to greater homogeneity in fat removal, higher deep dermis temperatures that stimulated collagen contraction and, conseguently, skin retraction, and to the possibility of removing more fat, thanks to the smaller vascular lesion and consequently less bleeding.
CONCLUSION
Ultrasound-assisted liposuction is a renowned method for fat removal, and many professionals use this technigue in their practices. The latest studies have proven its safety.
In evaluating the 348 consecutive ultrasound-assisted liposuctions, we obtained satisfactory results with proper skin accommodation in the treated areas. That is partly due to the dermis contraction caused by the thermal effect.
The most frequently used type of infiltration was super-wet, i.e., 1.35 ml infiltrated for 1 ml aspirated, which caused the least number of edemas or seromas.
Occasional complications, such as thermal injuries at the site of entrance of the cannula, were not significant and were related to routine care.
The final and long-term analysis showed improved skin accommodation and better effects on the cases difficult to be treated, such as gynecomasty, dorsum, and secondary liposuction.
REFERENCES
1. Fischer A, Fischer GM. Revised technique for a cellulitis fat reduction in riding breeches deformity Bul In Aca Cos Surg. 1977;240.
2. Illouz Y. Bodv Contouring by Lipolysis: A five years experience with over 3000 Cases. Plast Reconstr Surg. 1983;72:591-7.
3. Grippaudo FR, Matarese RM, Macone A, Mazzocchi M, Scuderi N. Effects of Traditional and Ultrasonic Liposuction on Adipose Tissue: A Biochemical Approach. Plast Reconstr Surg. 2000;106: 197-9.
4. Zocchi ML. Basic Physics for ultrasound-assisted lipoplasty Clin Plast Surg. 1999;26:209-20.
5. Gasperoni C, Salgarello M, Gasperoni P. External Ultrasound Used in Conjunction with Superficial Subdermal Liposuction: A safe and effective Technique. Aesth Plast Surg. 2000;24:253-8.
6. Fournier P. Liposculprure. Ma Technique. Paris: Anette; 1989.
7. Fodor PB, Watson J. Wetting solutions in ultrasound-assisted lipoplasty. Clin Plast Surg. 1999;26:289-93.
8. Klein JA. The tumescent technique. Dermatol Clin. 1990;8:425.
9. Grotting J, Beckenstein M. The solid-probe technique in ultrasound-assisted lipoplasry Clin Plast Surg. 1999;26:245-54.
10. Rohrich RI, Beran SI, Kenkel JM, Adams WP, Dispaltro F. Extending the Role of Liposuction in Body Contouring with Ultrasound-Assisted Liposuction. The Am Soc Aesth Plast Surg. Course 511.
11. Kloehn RA. Liposuction with "sonic sculprure": six years experience with more than 600 patients. Aesth Surg. 1996;16: 123-8.
12. Zocchi ML. Ultrasonic assisted lipop lastv.Technical refinernents and clinicai evaluations. Clin Plast Surg. 1996;23: 575-98.
13. Ingra H, Satur N. Tumescem liposuction versus internal ultrasonic-assisted rumescent liposuction. A side-to-side cornparison. Dermatol Surg.1997;23: 1213-8.
14. Lawrence N, Cox SE. The efficacy of external ultrasound-assisted liposuction: a randomized controlled trial. Dermatol Surg. 2000;26:329-32.
15. Thornton LK, Nahai F. Equipment and instrumentation for ultrasound-assisted lipoplasty. Clin Plast Surg. 1999;26:299-304.
16. Maxwell P. Use of hollow canula technology in ultrasound-assisted lipoplasty Clin Plast Surg. 1999;26:255-9.
17. Maxwell p, Ablaza VI, Gingrass MK, Perry LC, Fischer J. Tissue temperatures during ultrasound assisted lipoplasty. Plast Reconstr Surg. 1998;102:534-42.
18. Chang C, Commons GA. Comparison of various ultrasound technologies. Clin Plast Surg. 1999;26:261-8.
19. Rohrich R, Raniere I, Beran S, Kenkel J. Patient evaluation and indications for ultrasound-assisted lipoplasty. Clin Plast Surg. 1999;26:269-78.
20. Rohrich R, Raniere J, Kenkel I, Beran S. Operative principies for optimizing results in circunferencial body contouring with ultrasound-assisted lipoplasty. Clin Plast Surg. 1999;26:305-16.
21. Rohrich R, Beran SI, Fodor PB. The role of subcutaneous infiltration in suction-assisted lipoplasty: a review. Plast Reconstr Surg. 1997;99:514-9.
22. Nahai F. Positioning for ultrasound-assisted lipoplasty. Clin Plast Surg. 1999;26:235-43.
23. Rao RB, Ely SF, Hoffman RS. Deaths related to Liposuction.New Engl J Med. 1999;340:1471-5.
24. Tebbetts JB. Rapid Probe movement ultrasound-assisted lipoplasty Aesth Surg. 1999;19:17-23.
25. Wilkinson TS. External ultrasound-assisted lipoplasty. Aesth Surg. 1999;19:124-9.
26. Gingrass M, Kenkel J. Comparing ultrasound-assisted lipoplasty with suction-assisted lipoplasty Clin Plast Surg. 1999;26:283-8.
27. Mateo M, Pérez V. Sistematic procedure for ultrasonically assisted lipoplasty Aesth Plast Surg. 2000;24:259-69.
28. Hetter GP. The effect of low-dose epinephrine on the hematocrit drop following lipolisis. Aesth PIast Surg. 1984;8:19-22.
29. Howard BK, Beran SI, Kenkel JM, Krueger J, Rohrich RJ. The effects of ultrasonic energy on peripheral nerves: implications for ultrasound-assisted liposuction. Plast Reconstr Surg. 1999;103:984-9.
30. Trott SA, Rohrich RJ, Kenkel JM, Adams WP Jr, Robinson JB Jr. Sensory changes after traditional and ultrasound-assisted liposuction using computer-assisted analysis. Plast Reconstr Surg. 1999;103:2016-25.
31. Rohrich RJ, Morales DE, Krueger JE, Ansari M, Ochoa O et al. Comparative lipoplasty analysis of in vivo-treated adipose tissue. Plast Reconstr Surg. 2000; 105 :2152-8.
32. De Souza Pinto EB, Erazo PI, Muniz AC, Prado MY, Gerent KMM et al. Superficial Liposuction. Aesth Plast Surg. 1996;20:111-22.
I - Senior Member of the Brazilian Society of Plastic Surgery and of the Brazilian Society of Laser Medicine and Surgery. Member of the International Society of Aesthetic Plastic Surgery. Corresponding Member of the American Society for Aesthetic Plastic Surgery. Guest lecturer of the Plastic Surgery Facility of Curitiba's Evangelist University Hospital.
II - Senior Members of the Brazilian Society of Plastic Surgery and of the Brazilian Society of Laser Medicine and Surgery.
III - Member of the Brazilian Society of Plastic Surgery.
IV - Candidate Member of the Brazilian Sociery of Anesthesiology.
Address for correspondence:
Ruth Graf, MD R. Solimões, 1184
80810-070 - Curitiba - PR Brazil
Phone: (5541) 335-7237 - Fax: (55 41) 335-9394
e-mail: ruthgraf@bsi.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter