

Original Article - Year 2018 - Volume 33 -
Breast reconstruction in young women and their peculiarities
Reconstrução mamária em mulheres jovens e suas peculiaridades
ABSTRACT
INTRODUCTION: To evaluate the main features and methods used in breast reconstruction in young women considering their unique characteristics.
METHODS: A retrospective records review of patients who underwent mastectomy followed by breast reconstruction between January 2008 and December 2015 was conducted, selecting those reconstructions that were performed in women younger than 40 years.
RESULTS: Forty-three patients were selected. The average age was 33.86 years. Many had some comorbidities, the most common being overweight and anxiety/depressive disorder. Fourteen patients had a family history of the disease. Most were diagnosed with invasive ductal carcinoma. Additional cancer treatments were administered in most cases. All patients underwent a full mastectomy in the breast with cancer, and in 16, there was the option of contralateral risk-reducing mastectomy. Of the 43 reconstructions, 36 were immediate and 7 were delayed, and 17 involved use of implants, 13 involved use of tissue expanders, 4 involved the TRAM, and 9 involved the GD. We observed 15 complications; the most severe were infection with reconstruction loss in one patient and areola necrosis in another.
CONCLUSIONS: Young women undergoing breast reconstruction represent a population subgroup with its own characteristics. The tumors and personal and social patterns differ, and based on this long list of variables, treatment options are diverse. In our series, breast implants and tissue expanders were often most used.
Keywords: Breast neoplasms; Mastectomy; Mastectomy, radical; Young adult; Mammaplasty; Postoperative complications.
RESUMO
INTRODUÇÃO: O objetivo do trabalho foi avaliar as principais características e métodos utilizados na reconstrução mamária de mulheres jovens, considerando suas peculiaridades.
MÉTODOS: Foi realizada uma revisão retrospectiva dos prontuários das pacientes submetidas à mastectomia seguida de reconstrução mamária no período de janeiro de 2008 a dezembro de 2015, sendo selecionados aqueles cuja reconstrução foi realizada em mulheres de até 40 anos de idade.
RESULTADOS: 43 pacientes foram selecionadas. A média de idade foi de 33,86 anos. Grande parte possuía alguma comorbidade, sendo as mais comuns o sobrepeso e o transtorno ansioso/depressivo. Quatorze pacientes tinham história familiar da doença. A maioria obteve o diagnóstico de carcinoma ductal invasor. Tratamentos oncológicos complementares foram realizados em grande parte dos casos. Todas as pacientes foram submetidas à mastectomia total na mama portadora da neoplasia, sendo que em 16 houve a opção pela mastectomia redutora de risco contralateral. Do total de 43 reconstruções, 36 foram imediatas e 7 tardias; sendo 17 reconstruídos com implantes mamários, 13 com expansores teciduais, 4 com TRAM e 9 com GD. Houve 15 complicações, sendo as mais graves um caso de infecção com perda da reconstrução e um caso de necrose de aréola.
CONCLUSÕES: Mulheres jovens submetidas à reconstrução mamária representam um subgrupo populacional com características próprias. Os padrões tumorais, pessoais e sociais diferem e, com base nesta imensa lista de variáveis, as possibilidades de tratamento são diversas. Em nossa casuística, o emprego de implantes mamários e expansores teciduais foi realizado com maior frequência neste subgrupo de pacientes.
Palavras-chave: Neoplasias da mama; Mastectomia; Mastectomia radical; Adulto jovem; Mamoplastia; Complicações pós-operatórias.
The World Health Organization estimates that more than a million new cases of breast cancer occur each year, making it more common among women (except for non-melanoma skin cancers)1,2. Statistics show that one in nine women will develop the disease at some time in their life2 and that about 1-7% of these diagnoses affect young women2-5.
Breast neoplasia in this population tends to present more aggressively, with a greater chance of recurrence and death2,4,5. Young women with breast cancer are also more commonly submitted to complementary treatments, such as radiotherapy, chemotherapy, and contralateral prophylactic mastectomy when compared to those of more advanced age5.
Breast reconstruction in this population subgroup presents certain peculiarities in relation to the standard subgroup.
The impacts of mastectomy are usually more pronounced in these women, which affects repair strategies5. In addition, young women tend to present a different body constitution from older women, a greater concern with abdominal wall morbidity, ongoing or future motherhood, return to usual activities, and sexuality5. The literature, although controversial, indicates a greater trend of reconstruction using implants and expanders in this population subgroup, while repair with isolated autologous flaps is employed less frequently5.
OBJECTIVE
The objective of this study was to evaluate the main characteristics and methods used in breast reconstruction in young women, considering their unique characteristics.
METHODS
A retrospective review of the medical records of patients who underwent mastectomy (due to the diagnosis of breast cancer) followed by breast reconstruction was carried out from January 2008 to December 2015, and reconstructions that were performed in women up to 40 years of age were selected.
All patients signed an informed consent term authorizing the use of their records and information about their treatment, as well as their photographs, for scientific purposes.
This work followed the principles of the Declaration of Helsinki, adopted by the 18th World Medical Assembly, Helsinki, Finland, in June 1964, and corrected by the 29th Medical Assembly, Tokyo, Japan, on October 1975, and 35th World Medical Assembly Venice, Italy, on October 1983, and by the 41st Hong Kong World Medical Assembly, on September 1989.
The data analyzed were personal characteristics (such as age and presence of comorbidities), family history, tumor characteristics, oncological treatment adopted, moment and method of breast reconstruction performed, and observed complications.
The oncological treatment was defined by the mastologist and/or clinical oncologist based on the histological, immunohistochemical, and staging characteristics of each patient.
All breast reconstructions were performed by the same surgeon. The reconstruction method was chosen based on the careful analysis of the case by the assistant plastic surgeon along with the personal preference of the patient.
All patients underwent postoperative follow-up of at least 6 months.
RESULTS
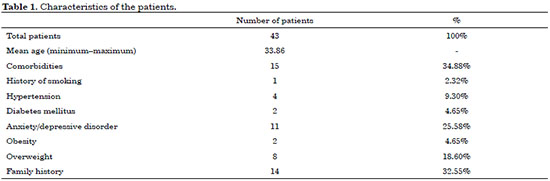
During the period covered, 43 patients were selected from a total of 436 patients who underwent breast reconstruction, corresponding to 10% of the sample. The mean age of the patients was 33.86 years, the youngest patient being 23 years old. A large proportion had comorbidities, the most common being overweight and anxiety/depressive disorder at the time of reconstruction. Fourteen patients (32.55%) had a family history of breast neoplasia. Table 1 presents the characteristics of the patients studied.
Using the chi-square test, we did not observe statistical significance when analyzing the relation between family history of breast cancer and unilateral or bilateral mastectomy (Table 2).
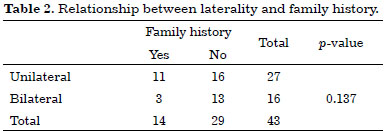
Most patients (97.67%) were diagnosed with invasive ductal carcinoma (ICD). In most cases, complementary treatments were performed. All patients were submitted to total mastectomy in the breast bearing the neoplasia, and in 16, there was still the option for contralateral risk-reducing mastectomy. Of the total of 43 reconstructions, 36 (83.7%) were performed at the same time as the mastectomy (immediate), and in 7 (16.3%), the breast was reconstructed late. Table 3 details the treatments adopted.
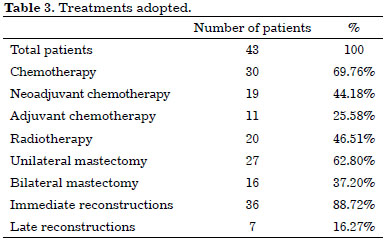
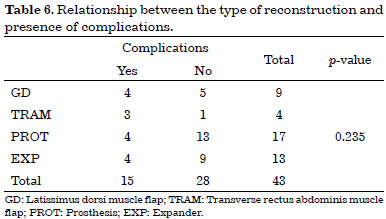
As shown in Table 4, of the 43 cases studied, 17 were reconstructed with breast implants (Figure 1), 13 with tissue expanders (Figure 2), 4 with myocutaneous flaps of the rectus abdominis muscle (TRAM) (Figure 3), and 9 with myocutaneous flaps of the dorsal muscle associated with the breast implant (GD) (Figure 4). We obtained 15 complications, the most serious being infection with loss of reconstruction in one patient and areola necrosis in another.
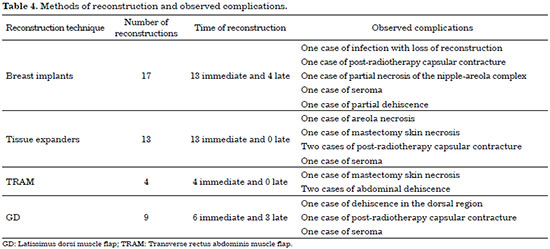
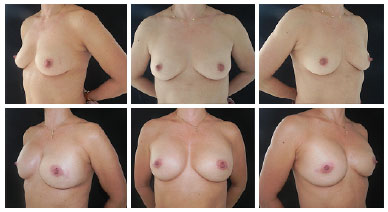
Figure 1. The upper panels show preoperative images. The lower panels show the aesthetic results after 6 months of bilateral mastectomy and immediate reconstruction with prosthesis.

Figure 2. The upper panels show preoperative images. The middle panels show the aesthetic results after 4 months of mastectomy of the left breast and immediate reconstruction with expander. The lower panels show the aesthetic results after 6 months of the second stage of breast reconstruction and symmetrization.
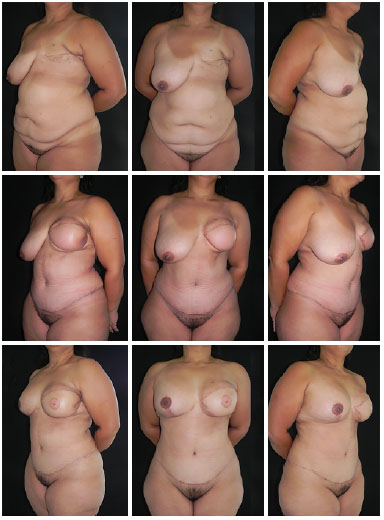
Figure 3. The upper panels show preoperative images. The middle panels show the aesthetic results after 4 months of late breast reconstruction using a transverse flap of the rectus abdominis muscle. The lower panels show the aesthetic results after 6 months of the second stage of breast reconstruction and symmetrization of the contralateral breast.
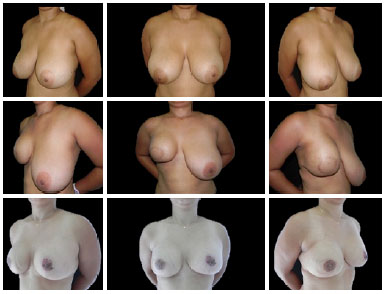
Figure 4. The upper panels show preoperative images. The middle panels show the aesthetic results after 5 months of mastectomy, followed by immediate breast reconstruction using a flap of the latissimus dorsi muscle, and placement of silicone prosthesis. The lower panels show the aesthetic results after 8 months of the second stage of breast reconstruction and symmetrization of the contralateral breast.
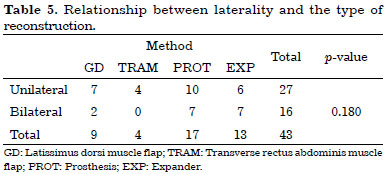
Using the chi-square test, we did not observe statistical significance when analyzing the relationship between unilateral or bilateral mastectomy and the type of reconstruction performed (Table 5), nor when we studied the relationship between the type of reconstruction performed and the occurrence of postoperative complications (Table 6).
DISCUSSION
This is a novel national study that evaluated breast reconstruction in young women.
When searching for articles of other nationalities on the subject, we note that the definition of young women in this area is variable. Most authors use the age of up to 35 or 40 years to refer to this population3,6. We chose to use in this study the age of up to 40 years because we consider this subgroup more homogeneous than when it was extended to later ages.
This population group has tumor, physical, psychological, and social characteristics different from those of patients commonly affected by breast neoplasia3,7. The disease, disease perception, and treatment strategies are different in this population.
Regarding tumor characteristics
The literature indicates that women under the age of 35 years have a lower rate of ductal carcinoma in situ3. This fact is probably due to a detection bias, since women in this age group do not usually undergo mammograms and, when they do, the sensitivity is lower because of the high breast density3.
The prevalent disease type in this age group is ICD, which occurs in more than 85% of patients2. The other histological types occur in the minority of cases. In our series, 97.67% of the diagnoses were of ICDs and 2.32% of invasive lobular carcinomas (ILC). We call attention to the fact that the ILC patients in this age group were all subjected to radical treatments - bilateral mastectomy - since the chance of recurrence and contralateral disease is increased many times in them compared to the general population.
In addition, the literature reveals that tumors in young women usually present negative estrogen and progesterone receptors2,3, which corroborates to a worse prognosis, due to the lack of targeted treatments and the possibility of hormonal blockade as a protective factor of minimizing relapse.
Concerning the presentation of the disease
Although some authors have a considerable sensitivity of mammography and ultrasonography for young patients with breast cancer (around 85% and 88%, respectively)4, these patients are not in the age range of population screening. As they do not undergo screening tests (unless the patient already knows from the family history that they may have an increased risk of developing cancer), tumors of a younger age are usually only discovered when palpable (in the breast or armpit) or when the patient presents symptoms, indicating, therefore, a more advanced stage3,4,6.
These tumors also tend to be more associated with vascular invasion and involvement of locoregional lymph nodes2, besides being more aggressive and with a greater chance of recurrence and death2-4,8.
Regarding cancer treatment
It is known that the surgical treatment of breast neoplasia can be categorized into 2 alternatives: conservative surgeries or total mastectomy. Factors that direct the decision to one or another approach include tumor size and type, multicentricity, breast volume, family history, and/or genetic predisposition to the disease9.
Although some historical studies suggest that there is no significant difference in survival between patients who underwent total mastectomy and those who underwent conservative procedures, some authors suggest that there is a higher rate of local recurrence in the latter group when there is a long follow-up3,6,10.
A portion of scholars argue that young women treated with conservative breast surgery have a risk of tumor recurrence up to nine times higher than women over the age of 60 years3,4. Other authors suggest that conservative procedures in women with stage I or II breast cancer could be offered as the first choice, since it would not affect survival, despite the risk of increased recurrence10.
By our own clinical practice, we noticed that there is, among this population, a relevant concern with the occurrence of a new diagnosis of breast cancer in the future, in both the breast bearing the neoplasia and the contralateral breast. This concern also extends to some mastologists because of the possible genetic origin of the tumor and the many years of life that these patients will still face if they are cured in this episode.
In our series, all 43 patients underwent total mastectomy in the breast bearing the neoplasia. In 16 patients, there was also the option for contralateral risk-reducing mastectomy. However, despite these observed occurrences (and observed more notably in the literature in recent years), most studies on the subject are not clear in demonstrating whether there is actually a survival gain with the use of these methods3,6.
The cancer treatment in this age group is usually multidisciplinary. The literature suggests that combination with radiotherapy, chemotherapy, and hormone therapy should be strongly considered in young women3. In our series, this fact was also noticed, with the majority of the patients being submitted to complementary oncological treatments.
Regarding the impacts of mastectomy
We know that the impacts of a mastectomy are more damaging in younger than older women3,7,8. This concerns financial, family, personal, and emotional aspects.
Studies show that young women tend to have greater problems in their career and financial lives after the diagnosis of breast cancer7, probably related to time away from work.
The literature also shows that young women with breast cancer are more likely to have a partner than older women7. However, although they theoretically have the husband's company to support them, they are also more likely to have difficulties in their relationships because of the disease7, mainly related to the disorders of acceptance of their own body image and dysfunctions of sexuality3,5.
While older women typically have a large family network (because of their offspring, children, grandchildren, and close relatives) to help with care and postoperative returns, we note that younger women usually attended consultations, alone or with friends (since they do not have children of ages who can help them, and although they usually have a partner, he often worked at the time of the appointment). It should also be pointed out that many had not yet formed a family and that the treatment of the disease itself could make it impossible to do so.
As for the psychological aspect, we know that the breasts are of great importance for the preservation of the psychological integrity of the woman and that the idea of amputation has devastating sequels. This fact is even larger in younger women3,9. We observed that a significant proportion of our patients started psychiatric treatment concomitantly with cancer treatment and had a high rate of depressive disorder (25%). This fact was also found in the literature3.
Regarding the idea of plastic surgery and choice/role of the surgeon
It is well known that women at this age are more amenable to the idea of reconstructive plastic surgery in general. Studies show that they are also more likely to undergo breast reconstruction after mastectomy5,7,8. We found that only those patients in whom the mastologist contraindicated the reconstruction underwent the procedure late - only 16%. However, we have noticed that younger patients usually present more distress and anxious about the idea of reconstruction and its physical, emotional, and aesthetic implications.
Due to the greater access to the information of this population subgroup, which have several sources of consultation, many visited the clinics already aware of the alternatives of reconstruction and advantages and disadvantages of each method.
Some previous studies have shown that young women seek information about the disease more frequently (mainly on the Internet) and adopt a more active position in the treatment itself when compared to the older women7. We had the same observations, noting also a tendency of the plastic surgeon to leave the position of mere presenter and occupy that of a debater, interacting much more in the consultation with these patients.
We observed that the information available on the Internet (and even on the plastic surgeon's own website), recommendation of known patients who have already undergone the same disease, and catalog of the agreement were the main factors that led the patients to visit that clinic.
Regarding the choice of technique
Literature shows that young women are more concerned about their appearance and sexuality than older women7. Since we are in a tropical country, where body exposure is clearly more prevalent, we believe that these values are even more prominent in the present.
We know that the expectations of breast reconstruction are specifically related to the symmetry of the breasts, in addition to the shape and size of the breasts.
Studies in the literature and our own clinical practice indicate that most breast augmentation procedures are performed in younger women6,7, which would suggest that such patients may be more interested than those of older ages in breast augmentation at the time of breast reconstruction7. Regarding this last observation, we noticed that the majority of the younger age group sought larger breasts, contrary to what is usually observed in older women, who usually request smaller breasts.
Some presented at the initial consultation the desire for breast reconstruction using the abdominal musculature, aiming to eliminate the protruding abdomen and excess skin. This notion reinforces the idea of the aesthetic concern previously mentioned. However, this option ended up being discarded by the absence of a donor area (attending gymnasiums, doing physical exercises, among others), which made it impossible to choose the option of reconstruction with the use of autologous flaps alone. The future desire to become pregnant was another factor considered, which made reconstruction with the TRAM method a relative contraindication, performed in only 4 patients.
In our study, TRAM reconstruction was used mainly performed in overweight patients, including 2 obese women (body mass index of 35.26 kg/m2 and 31.83 kg/m2). All were already mothers and, because of previous pregnancies, had associated skin flaccidity.
The option for the reconstruction method was also influenced by the period of postoperative recovery, which would influence the time of return to work and care of the still small children. This fact was also found in the literature7,11. The woman showed up, even at the time of her own illness, a concern for the well-being of the offspring and that of her family.
We observed that the majority of the patients of this age group did not present rejection to the silicone implant (which occasionally occurs in more advanced age groups). Some had even previously placed silicone implants for aesthetic reasons.
Many have opted for reconstruction with silicone implants or tissue expanders, more than 50% in our series, due to these factors already mentioned. The literature, although controversial, points to this trend, which is even more relevant in bilateral reconstructions5.
We know that in cases of bilateral reconstructions, a similar procedure when employed on both sides makes the possibility of symmetrical results easier8, which made the reconstruction option of prostheses and expanders even more meaningful. In addition, the amount of tissue capable of being mobilized using autologous flaps alone did not allow the reconstruction of breasts of satisfactory size to that requested by the majority of patients (even more so in bilateral cases).
Regarding the results and complications
Although they are usually the carriers of more aggressive illnesses and experience more broadly (both physically and psychologically) the effects of treatment, young women are usually healthier and have fewer comorbidities than older women11. For these reasons, they tend to present lower rates of postoperative complications and lesser severity, providing better and faster results.
In our analysis, we could verify this fact. We observed that most of the complications were of smaller scope and easily treated. We obtained 15 complications, the most significant being infection with loss of reconstruction in one patient and necrosis of the areola (just one of the breasts in which a prophylactic mastectomy was performed). There were three cases of capsular contracture (all after adjuvant radiotherapy) that were properly treated with fat graft in neomama (in small cases) or with capsulotomy and breast implant replacement (in the most severe case). There were also two cases of mastectomy skin necrosis, one of seroma in the neomama region and three occurrences of small dehiscences in donor regions, all treated with minor procedures in the clinic.
We found that the level of demand is usually higher in this subgroup of patients than in patients with more advanced age. In many cases, the satisfaction of the patient was not only complete with the first stages of reconstruction, and additional surgical times were more commonly employed, aiming for greater symmetrization and better aesthetic result.
CONCLUSION
Young women subjected to breast reconstruction represent a population subgroup with their own characteristics.
Our work reveals interesting differences between the characteristics of the disease and treatment strategies between this population and the standard subgroup. Tumor and personal and social patterns differ, and based on this huge list of variables, the treatment possibilities are diverse.
Young women have a different body constitution. They present more aggressive tumors and are more likely to undergo complementary treatments, such as radiotherapy, chemotherapy, and contralateral prophylactic mastectomy. Usually, they tend to opt for breast reconstruction. Due to the scarcity of donor areas and future aspirations (both maternal, as well as professional and aesthetic), breast implants and expanders was used more frequently in this subgroup of patients in our series.
Further studies are needed to better characterize these patterns and make a more detailed analysis of the picture in this population subgroup. Our work is the basis for further studies on the subject.
We conclude that the individualization of the patient is the key to the success of breast reconstruction in this population and an essential tool to meet the expectations and wishes of the patient after the mastectomy. Each reconstructive technique has its indications, advantages, and limitations, which must be widely discussed with the patient for the best possible result.
COLLABORATIONS
MCC Final approval of the manuscript; completion of surgeries and/or experiments.
GCS Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; writing the manuscript or critical review of its contents.
JCD Final approval of the manuscript.
BPE Analysis and/or interpretation of data.
LDPB Analysis and/or interpretation of data.
DASS Analysis and/or interpretation of data.
IRJ Analysis and/or interpretation of data.
MCAG Writing the manuscript or critical review of its contents.
FTM Statistical analyses.
REFERENCES
1. Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Instituto Nacional de Câncer. Controle do câncer de mama: Documento de consenso. Brasília: Ministério da Saúde; 2004. 36 p.
2. McAree B, O'Donnell ME, Spence A, Lioe TF, McManus DT, Spence RA. Breast cancer in women under 40 years of age: a series of 57 cases from Northern Ireland. Breast. 2010;19(2):97-104. DOI: http://dx.doi.org/10.1016/j.breast.2009.12.002
3. Gabriel CA, Domchek SM. Breast cancer in young women. Breast Cancer Res. 2010;12(5):212. DOI: http://dx.doi.org/10.1186/bcr2647
4. Liukkonen S, Leidenius M, Saarto T, Sjöström-Mattson J. Breast cancer in very young women. Eur J Surg Oncol. 2011;37(12):1030-7. PMID: 21937191 DOI: http://dx.doi.org/10.1016/j.ejso.2011.08.133
5. Vogel JE, Chu C, McCullough M, Anderson E, Losken A, Carlson GW. Breast cancer in women under age 40 years: treatment by total mastectomy and reconstruction. Ann Plast Surg. 2011;66(5):557-60. PMID: 21451370 DOI: http://dx.doi.org/10.1097/SAP.0b013e318216b648
6. Cardoso F, Loibl S, Pagani O, Graziottin A, Panizza P, Martincich L, et al.; European Society of Breast Cancer Specialists. The European Society of Breast Cancer Specialists recommendations for the management of young women with breast cancer. Eur J Cancer. 2012;48(18):3355-77. DOI: http://dx.doi.org/10.1016/j.ejca.2012.10.004
7. Lee CN, Foster RD. Breast reconstruction after mastectomy in young women. Breast Dis. 2005-2006;23:47-52. PMID: 16823166 DOI: http://dx.doi.org/10.3233/BD-2006-23107
8. Marín-Gutzke M, Sánchez-Olaso A. Reconstructive surgery in young women with breast cancer. Breast Cancer Res Treat. 2010;123 Suppl 1:67-74.
9. Piñero Madrona A. Surgical treatment of breast cancer in young women. Breast Cancer Res Treat. 2010;123 Suppl 1:21-4.
10. Mahmood U, Morris C, Neuner G, Koshy M, Kesmodel S, Buras R, et al. Similar survival with breast conservation therapy or mastectomy in the management of young women with early-stage breast cancer. Int J Radiat Oncol Biol Phys. 2012;83(5):1387-93. PMID: 22300561 DOI: http://dx.doi.org/10.1016/j.ijrobp.2011.10.075
11. Ellsworth WA, Bass BL, Skoracki RJ, Heller L. Breast reconstruction in women under 30: a 10-year experience. Breast J. 2011;17(1):18-23. DOI: http://dx.doi.org/10.1111/j.1524-4741.2010.01020.x
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Daher Lago Sul, Brasília, DF, Brazil
3. Sociedade Brasileira de Anestesiologia, Rio de Janeiro, RJ, Brazil
Institution: Hospital Daher Lago Sul, Brasília, DF, Brazil.
Corresponding author:
Marcela Caetano Cammarota
SMHN, Quadra 2, Bloco C, Ed Crispim, sala 1315
Brasília, DF, Brazil - Zip Code 70710-149
E-mail: marcelacammarota@yahoo.com.br
Article received: January 16, 2017.
Article accepted: October 19, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter