

Case Report - Year 2017 - Volume 32 -
Retrograde flow medial plantar artery flap reconstruction for defects of the dorsal metatarsophalangeal region
Retalho plantar medial de fluxo retrógrado para reconstrução de defeitos de dorso de pé
ABSTRACT
INTRODUCTION: Complex reconstructions of the foot region are planned based on the anatomical subunits affected by the etiological factors of lesions. We have several options for covering defects of the back of the feet, from the simpler ones, such as local graft and local flap at random and locoregional pedicled flaps, to the more complex ones, such as free flaps. Here, we report a case in which an unpublished technique using a retrograde flow medial plantar flap in the reconstruction of dorso-distal structures of the foot was used. Its originality consisted in the passage of the flap of the plant to the back through the first intermetatarsal space.
METHODS: The patient was a 20-year-old woman who had a motorcycle accident, wherein she sustained foot trauma with loss of back substance at the first to fifth metatarsal level, with bone and tendon exposure, and retrograde flow medial plantar flap was used, with transposition to the back of the foot.
RESULTS: The reconstruction of the distal region of the forefoot and fingers is a challenge. Grafts are not ideal for deep defects and exposure of noble structures. Local flaps are inaccessible for finger defects. Furthermore, the free flaps are well indicated for large defects. The flaps of the medial plantar artery are indicated and consecrated to the forefoot region, and some authors have modified to the dorsum region of the first metatarsal.
CONCLUSION: This flap is useful for reconstruction of feet with dorsal lesions through this new technique that is unpublished in the literature, with the originality of the passage of the pedicle from the plant to the back through the first intermetatarsal space.
Keywords: Perforator flap; Surgical flaps; Foot injuries.
RESUMO
INTRODUÇÃO: As reconstruções complexas da região do pé são planejadas com base nas subunidades anatômicas acometidas e pelo fator etiológico da lesão. Para coberturas de defeitos de dorso de pé, temos várias opções, desde as mais simples como enxertia local e retalhos locais ao acaso e retalhos pediculados locorregionais e as complexas com retalhos livres. Este trabalho tem por objetivo relatar um caso, cuja tática cirúrgica inédita na literatura utilizou um retalho plantar medial de fluxo retrógrado na reconstrução dorso-distais do pé. Sua originalidade consiste na passagem do retalho da planta para o dorso através do primeiro espaço intermetatársico.
MÉTODOS: Paciente 20 anos, sexo feminino, vítima de acidente de moto com trauma no pé, com perda de substância de dorso ao nível de 1 ao 5 metatarso, com exposição de osso e tendão. Foi utilizado um retalho plantar medial de fluxo retrógrado, com transposição para o dorso do pé.
RESULTADOS: A reconstrução da região distal do antepé e dedos são desafios. Os enxertos não são ideais para defeitos profundos e com exposição de estruturas nobres. Retalhos locais não são acessíveis para defeitos de dedos. E os retalhos livres são bem indicados para defeitos grandes. Os retalhos de fluxo reverso da artéria plantar medial está indicado e consagrado para a região do antepé e alguns autores modificaram para região de dorso do primeiro metatarso.
CONCLUSÃO: Este retalho se mostra útil também para lesões de dorso de pé por meio dessa nova tática cirúrgica inédita na literatura, com a originalidade da passagem do pedículo da planta para o dorso através do primeiro espaço intermetatársico.
Palavras-chave: Retalho perfurante; Retalhos cirúrgicos; Traumatismos do pé.
Complex reconstructions of the foot region are planned based on the anatomical subunits affected by etiological factors of lesions1.
We have several options for covering defects of the back of the feet, from the simpler ones, such as local graft and local flanks at random and locoregional pedicled flaps, to the more complex, such as free flaps1.
Factors that determine the technique to be used depend on the extent of the wound and the noble structures that are exposed, such as muscle, tendon, vessels, and nerves.
In the medial retromalleolar space, approximately 3 cm distal to the top of the medial malleolus, the posterior tibial artery splits into the medial and lateral plantar arteries. The division of the posterior tibial artery occurs distal to the tibial nerve division in 87% of cases, proximal to division in 2% of cases, and at the same time in 11% of cases2.
The medial plantar artery generally has a smaller caliber than the lateral plantar artery (81% of cases), but may have a larger caliber (3% of cases) or be of the same caliber (16% of cases)2.
After emerging from the posterior tibial artery, the medial plantar artery enters the plantar compartment under the abductor muscle of the hallux.
Below this muscle, at the height of the talus-navicular joint, the medial plantar artery divides into superficial and deep branches. The distance between the origin of the medial plantar artery and the dividing point of its branches (superficial and deep) is 2.5 to 3 cm.
The superficial branch of the medial plantar artery continues distally in the muscular septum between the abductor muscle of the hallux and the short flexor of the fingers. Approximately three to four septocutaneous branches are sent to nourish the skin of the region, thus forming the anatomical base of the medial plantar flap2.
The medial plantar artery (APM) presents three branching patterns: a) Type A (54%) with the APM dividing into two branches with predominance of superficial; B) Type B (38%) with absence of deep branches and the APM remaining as a single artery (superficial APM); and Type 3 (9%) with a deep branch of a larger caliber reaching the hallux and a superficial branch of a smaller caliber2.
If we lacquer the medial plantar artery proximally, the blood flow to the plantar hollow comes through its anastomosis with the deep plantar arch and lateral plantar artery.
Distal dissection of the medial plantar artery determines the pivotal point for flap mobilization2. The retrograde flow medial plantar flap supplies the skin and subcutaneous cellular tissue from the plantar socket for reconstructions in the plantar region of the forefoot2,3-10.
OBJECTIVE
This paper aimed to report a case in which an unpublished technique using a retrograde flow medial plantar flap in the reconstruction of dorso-distal structures of the foot was used. The technique's originality consisted in the passage of the flap of the plant to the back through the first intermetatarsal space.
METHODS
This work was based on a case report with a chart review of a case in which an unpublished technique using a retrograde flow medial plantar flap in the reconstruction of dorso-distal structures of the foot was used.
RESULTS
The patient was a 20-year-old woman who had a motorcycle accident, wherein she sustained foot trauma with loss of back substance at the level of the first to fifth metatarsus, with bone and tendon exposure (Figure 1) and fracture of the fourth and fifth orthopedically treated metatarsus (Figure 2).

Figure 1. Defect of the dorsum of the foot from the first to the fifth metatarsals and transposition of the flap pedicle from the distal plantar flow to the dorsum through the first intermetatarsal space.

Figure 2. Fracture of the fourth and fifth metatarsals treated with fixation.
In this patient, a medial plantar flap with retrograde flow was used, based on the ligation of the proximal medial plantar artery with transposition to the dorsal region through the intermetabaric space (Figures 1 and 3).
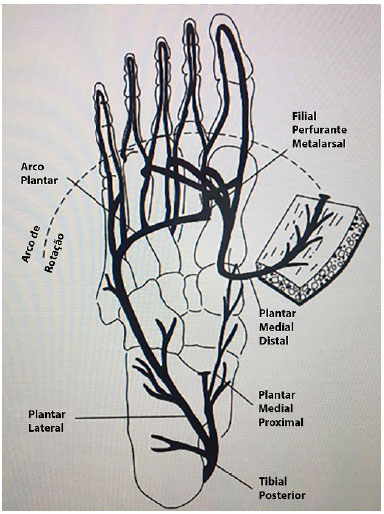
Figure 3. The vascular anatomy and the organization of the medial reverse plantar flap. Source: (fasciocutaneous island flap based on the medial plantar artery: clinical applications for leg, ankle, and forefoot. Baker GL, Newton ED, Franklin JD. Plast Reconstr Surg. 1990;85(1):47-58).
After isolation of the pedicle, a tunnel was created through the first intermetatarsal space to perform the transposition of the flap from the plantar region to the dorsal region and the first to fifth metatarsals (Figure 4).

Figure 4. Flap interposed and fixed on the dorsum of the foot.
Subsequently, the skin was grafted in the inguinal region to cover the donor area of the plantar cavus with a brown bandage for 5 days (Figure 5).

Figure 5. Fixation of the total skin graft on the donor area of the flap.
The evolution of the flap occurred without complications and without intercurrence approximately 1 year postoperatively with mild cicatricial retraction of the fifth metatarsal (Figures 6, 7, and 8).

Figure 6. Late postoperative aspect of the donor area of the flap with graft.

Figure 7. Late postoperative aspect of the flap on the dorsum of the foot.

Figure 8. Late postoperative aspect of the flap on the dorsum of the foot.
DISCUSSION
Wrists on the back of the feet are caused by trauma and infections or as a result of chronic vasculopathies due to smoking and systemic diseases, such as diabetes or hypertension3-5.
Moreover, the initial treatment of these wounds begins with clinical treatment in a sequence of surgical debridements, and the wound is better in appearance if the surgical process includes coverage with grafts, local flap or free flaps.
Reconstruction of the distal region of the forefoot and fingers is a challenge. Grafts are not ideal for deep defects and exposure of noble structures. Local flaps inaccessible for finger defects. Furthermore, free flaps are well suited for large defects.
The medial plantar flap is used for defects of the foot plantar region, particularly the heel region. Although reverse flow flaps are based on the retrograde blood flow from the distal medial plantar artery to the dorsal artery of the foot through the communicating (perforating) vessels of the first dorsal metatarsal vessels This type of flap is indicated for the reconstruction of distal defects of the plantar region in the metatarsal heads.
Based on the retrograde flow, the flap is consecrated to the forefoot region, and some authors have modified the dorsum region of the first metatarsal5-9.
Oberlin et al.9 described the extension of the pedicle with the ligature immediately after the bifurcation of the posterior tibial artery to the lateral and medial plantar arteries, which allowed to almost doubling the length of the pedicle and the arc of rotation to cover the defects of the plantar and dorsal regions of the foot.
Butler and Chevray10 recommended the following to improve the execution of this flap: confirming the retrograde flow before splitting the vessels proximally, considering performing supercharged retail or free flap conversion, preserving the perivascular fat of the pedicle, not performing compression in the grafting area of the flap donor area, and flexion foot fixation to decrease pedicle tension.
The disadvantages of the retrograde medial plantar flap are shown by the lack of sensitivity, risks of insufficient arterial supply and venous congestion, and poor aesthetic outcome of the flap donor area10.
Bertelli and Duarte11 recently described that the septal plantar artery is a good option for defects in the first metatarso-phalangeal area, although it is technically more difficult owing to limited blood supply.
Tsai et al.12 described two cases wherein the same flap was used to cover the back of the defects in the metatarsus region, through tunneling of the medial border of the foot, different from the unpublished technique of this case, which can cover defects of the first to fifth metatarsal dorsum through the transposition of the pedicle by the first intermetatarsal space.
CONCLUSION
The importance of this report is to demonstrate that the modified retrograde medial plantar flap being used for the treatment of forefoot injuries as described and consecrated in the literature by most authors. The application of this new technique is also useful, with the originality of the passage from the flap of the plant to the back through the first intermetatarsal space to cover lesions of the first to fifth metatarsus with the dorsal foot.
COLLABORATIONS
AVRFN Writing the manuscript or critical review of its contents.
AAS Completion of surgeries and/or experiments.
JLSM Final approval of the manuscript.
SCR Analysis and/or interpretation of data.
GDC Statistical analyses.
HGY Conception and design of the study.
REFERENCES
1. Barreiro GC, Batista RR, Busnardo F, Fereira MC. Reconstrução de planta de pé de acordo com o conceito das subunidades anatômicas. Rev Bras Cir Plast. 2010;25(3Suppl.1):81.
2. Macchi V, Tiengo C, Porzionato A, Stecco C, Parenti A, Mazzoleni F, et al. Correlation between the course of the medial plantar artery and the morphology of the abductor hallucis muscle. Clin Anat. 2005;18(8):580-8. DOI: http://dx.doi.org/10.1002/ca.20147
3. Karp NS, Kasabian AK, Siebert JW, Eidelman Y, Colen S. Microvascular free-flap salvage of the diabetic foot: a 5-year experience. Plast Reconstr Surg. 1994;94(6):834-40. PMID: 7972430 DOI: http://dx.doi.org/10.1097/00006534-199411000-00013
4. Amarante J, Martins A, Reis J. A distally based median plantar flap. Ann Plast Surg. 1988;20(5):468-70. DOI: http://dx.doi.org/10.1097/00000637-198805000-00012
5. Pallua N, Di Benedetto G, Berger A. Forefoot reconstruction by reversed island flaps in diabetic patients. Plast Reconstr Surg. 2000;106(4):823-7. PMID: 11007395 DOI: http://dx.doi.org/10.1097/00006534-200009020-00011
6. Coruh A. Distally based perforator medial plantar flap: a new flap for reconstruction of plantar forefoot defects. Ann Plast Surg. 2004;53(4):404-8. DOI: http://dx.doi.org/10.1097/01.sap.0000112287.56354.f8
7. Miyoshi T, Kura H, Usui M, Okamura K, Ishii S, Yamashita T. A retrograde medial plantar flap with the common plantar digital artery to the second toe. Plast Reconstr Surg. 2005;115(5):1445-7. PMID: 15809631 DOI: http://dx.doi.org/10.1097/01.PRS.0000157619.37978.43
8. Uygur F, Duman H, Ulkür E, Noyan N, Celiköz B. Reconstruction of distal forefoot burn defect with retrograde medial plantar flap. Burns. 2008;34(2):262-7. DOI: http://dx.doi.org/10.1016/j.burns.2007.02.010
9. Oberlin C, Accioli de Vasconcellos Z, Touam C. Medial plantar flap based distally on the lateral plantar artery to cover a forefoot skin defect. Plast Reconstr Surg. 2000;106(4):874-7. DOI: http://dx.doi.org/10.1097/00006534-200009020-00020
10. Butler CE, Chevray P. Retrograde-flow medial plantar island flap reconstruction of distal forefoot, toe, and webspace defects. Ann Plast Surg. 2002;49(2):196-201. DOI: http://dx.doi.org/10.1097/00000637-200208000-00014
11. Bertelli JA, Duarte HE. The plantar marginal septum cutaneous island flap: a new flap in forefoot reconstruction. Plast Reconstr Surg. 1997;99(5):1390-5. DOI: http://dx.doi.org/10.1097/00006534-199705000-00029
12. Tsai J, Liao HT, Ulusal BG, Chen CT, Lin CH. Modified retrograde-flow medial plantar island flap for reconstruction of distal dorsal forefoot defects--two case reports. Microsurgery. 2010;30(2):146-50.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Sociedade Brasileira de Microcirurgia, Brasília, DF, Brazil
3. Hospital Regional da Asa Norte, Brasília, DF, Brazil
4. Universidade de Brasília, Brasília, DF, Brazil
Institution: Hospital Regional da Asa Norte, Brasília, DF, Brazil.
Corresponding author:
Altino Vieira de Rezende Filho Neto
SMAS trecho 1, lote c Bl J, apt 703, ed living park Guara -Park Sul
Brasília, DF, Brazil - Zip Code 71218-010
E-mail: altinofn@hotmail.com
Article received: May 12, 2017.
Article accepted: September 23, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter