

Articles - Year 2002 - Volume 17 -
Concepts on Mammaplasties and Mastopexies
Conceituação sobre as Mamaplastias e Mastopexias
ABSTRACT
Many techniques have been described for reduction mammaplasty and mastopexy. The techniques for reduction mammaplasty and mastopexy combine the resection of skin and breast tissue. The assessment of excess skin and quantity of tissue to be removed is a key element in mammaplasties. The format of the skin differs from patient to patient, depending on the quality of the skin and its relation with the glandular tissue. The principies described in this paper have been used in more than 4,000 patients. Long-term course has shown satisfactory results. Scars are a problem that seems to concern surgeons more than patients themselves. It is concluded that patients who undergo mammaplasty are aware that there will be a scar after the surgery. However, how the scar looks is more important than how long it is.
Keywords: Mammaplasty; breast reduction; mastopexy; breast plastic surgery
RESUMO
Muitas técnicas têm sido descritas para a mamaplastia redutora e para a mastopexia.
As técnicas para a mamaplastia redutora e para a mastopexia combinam a ressecção de pele e tecido mamário. A avaliação do excesso de pele e da quantidade de tecido a ser removido é elemento decisivo nas mamaplastias. O formato da pele difere de paciente para paciente, dependendo da qualidade da pele e da relação desta com o tecido glandular.
Os princípios descritos neste trabalho foram utilizados em mais de 4.000 pacientes. A evolução a longo prazo mostrou resultados satisfatórios. A cicatriz é um problema que incomoda mais ao cirurgião que às pacientes.
Conclui-se que a paciente ao submeter-se à mamaplastia sabe que portará cicatriz após a operação. Contudo, a aparência da cicatriz é mais importante que seu comprimento.
Palavras-chave: Mamaplastia; redução mamária; mastopexia; cirurgia plástica das mamas
Techniques for reduction mammaplasty and mastopexy have been developed gradually, as have their philosophical concepts. Reduction mammaplasty is successful when it provides good appearance, and adequate consisteney, size, and shape, with the smallest sear possible.
Every breast surgery involves the resection of skin and breast tissue, but not all patients should have the same type of reseetion of skin and breast tissue.
When a patient wants to undergo mammaplasty, it is because she is not happy with how her breasts look. She is mueh more worried with how they will look after surgery than with the sear. It makes no sense to make an incision in the breast without attaining the best possible shape, merely to reduee the size of the future scar.
The aim is to provide the best results, rather than merely improve appearance. A final result with a small sear and poor shape will be questioned by the patient. If the result is a long and discreet sear, but with good appearance of the breasts, the patient will be happy. To undergo breast surgery is to substitute breasts whose shape the patient does not like for breasts with an excellent shape, aspect and consistency - but with a scar. Good surgery norrnally leaves barely visible scars.
Every patient who wants to have mammaplasty knows beforehand that such surgery will leave a scar. Breasts are different from each other, and thus, surgeries will also be different and, consequently, every scar will differ in quality and appearance, while their lengths do not matter much. It is the aspect of the scar that matters rather than its size.
PLANNING THE MAMMAPLASTY
When planning for a mammaplasty, many factors have to be taken into account: a) the size and a consistency of the breasts; b) the degree of ptosis; e) the distance between the sternal furcula and nipples; d) the quality of the skin; and, most importantly, e) the relation between the breast and skin tissue. Depending on these variables, we think: that each breast should have its won marking (rather than standard) and tissue resection should be individualized(1). In short, the greater the excess skin in relation to breast tissue, the greater will be the quantity of skin removed. The quantity of resected skin determines the length of the inframammary scar, depending on the size of the breasts and chiefly on the relation between skin and breast tissue.
When we try to reduce the length of the scar, the shape and appearance of the breasts are often affected.
We will first address the types of skin marking, and then go on to describe the forms of tissue resection.
SURGICAL MARKING - SKIN RESECTION
Firstly, a hemiclavicular line is drawn to the submammary sulcus through the nipple. A point is marked on the projection of this line the submammary sulcus. This point, called "A", corresponds to the future position of the mammilary-areolar complex. This point may be positioned a little lower in cases in which difficulty to lift the nipples is expected. After determining the position of point "A", the most important maneuver takes place, which is marking points "B" and "C" (Figs. 1a-e). The definition of these points depends on the relation between skin and breast tissue, as well as on the experience and sensitivity of the surgeon. Points "B" and "C" define the new shape aod consistency of the breast, which should not go further than 7 cm beyond point "A" because, if these lines are too long, the distance of the lower end of the areola to the submammary projection will have to be extended and, in the long term, the appearance of the breasts will not be good. These lines may be more or less curved, depending on the excess skin(2). Points "B" and "C" will later be connected to the lateral and medial ends of the inframammary projection (Figs. 2a and b). The length of the inframammary scar depends on the size of the breast and on the relation between skin and breast tissue.
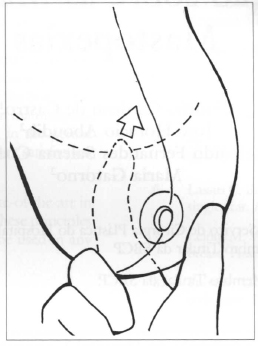
Fig. 1a - Schematic representation of marking point "A".

Fig. 1b - Transoperative view.
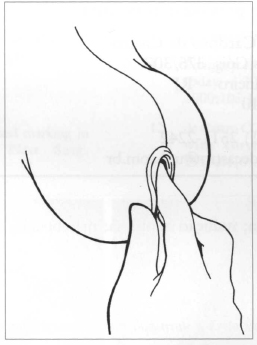
Fig. 1c - Evaluation of the location of points "B" and "C".

Fig. 1d - Transoperative view.

Fig. 1e - Another transoperative view of the marking of points
"B" and "C".
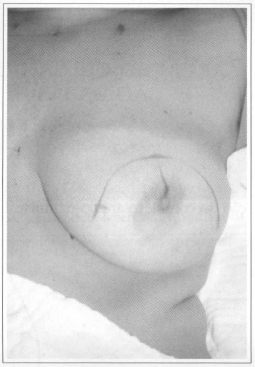
Fig. 2a - Point "A" linked to points "B" and "C". These lines may be more or less eurved, depending on breast flaccidity. These lines should not exceed 7 cm.
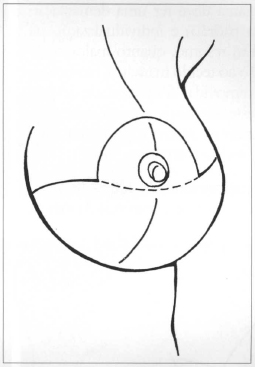
Fig. 2b - Points "B" and "C" are connected to the ends of the mammary sulcus.
Bearing Pitanguy's principles (5,11) in mind, there are three different types of skin markings, that result in three different types of scar (Fig. 4): a) classical inverted "T" (Figs. 5a-d); b) inverted "T" with small compensation (Figs. 6a-d); and c) vertical scar (Figs. 7a-d). All these techniques leave a periareolar scar.
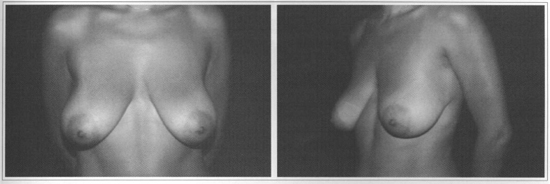
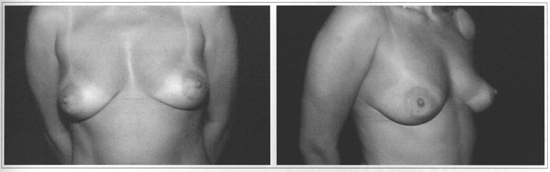
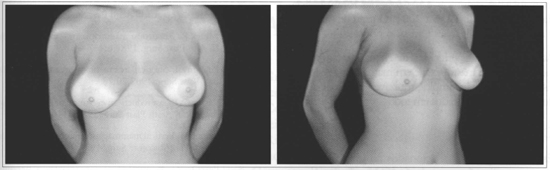
Figs. 3a and 3b - Preoperative view of a patient with mammary ptosis. There is no tissue on the upper mammary pole. Voluminous skin excesses.
Figs. 3e and 3d - One year after mastopexy. Only skin was removed. No scars are noticeable.

Fig. 4 - Schematic representation of three different types of skin marking.
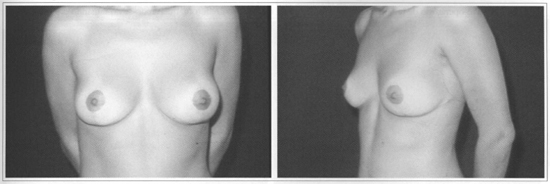
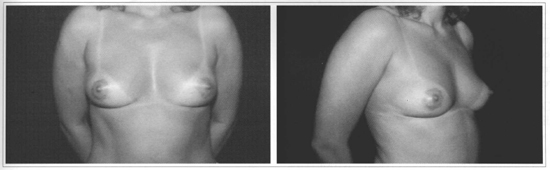
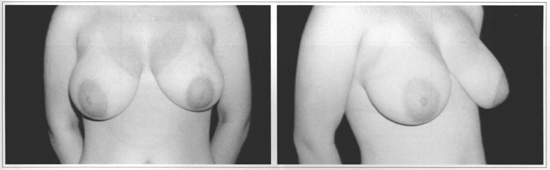
Figs. 5a and 5b - Preoperative view of patient with indication for reduction mammaplasty, who complained of the size of her breasts.
Figs. 5c and 5d - Eight years after reduction mammaplasty. During that period, the patient gave birth and breastfed normally. The shape, size and consistency were maintained.
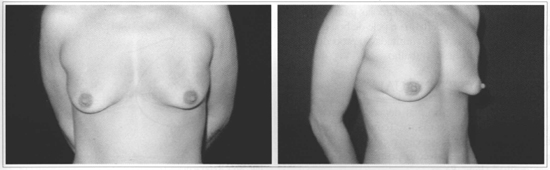
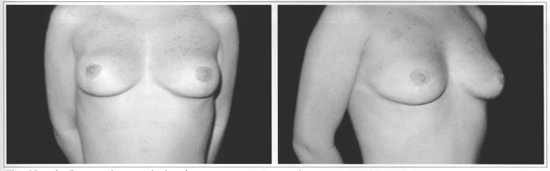
Figs. 6a and 6b - Patient with mild hypertrophy and good quality skin.
Figs.6c and 6d - Six months after mastopexy. Vertical scar and small scar in the subrnammary sulcus.
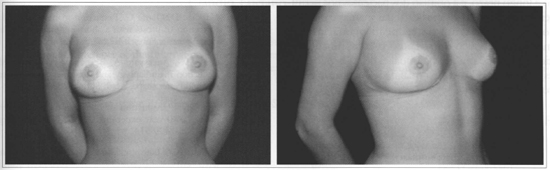
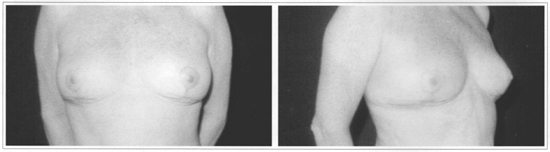
Figs.7a and 7b - 37 year-old patient with mammary ptosis. Good qualiry skin.
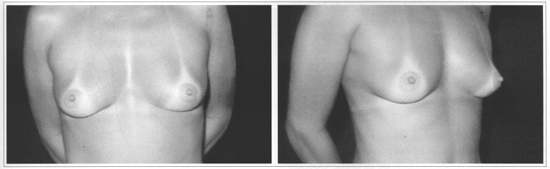
Figs.7c and 7d - 3 years after vertical mastopexy.
We have been using a periareolar approach for selected cases (slight hypertrophy and good quality skin). As indications are limited, this procedure will not be discussed in this papelr.
TISSUE RESECTION
The type of tissue resection depends on the size, consistency and shape of the breast. We have been using three different types of resection of breast tissue: a) plane resection; b) posterior resection; c) u-shape resection (Figs. 8a-c).
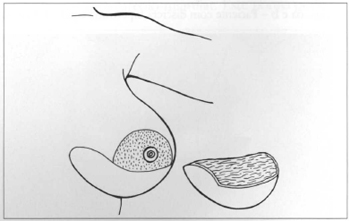
Fig. 8a - Scheme of plane resection.
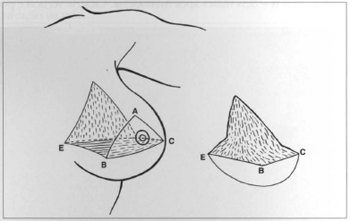
Fig. 8b - Schematie representation of posterior rescetion.
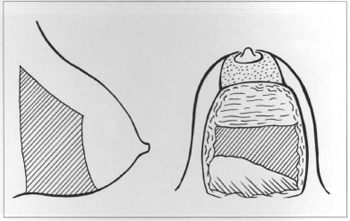
Fig. 8c - "u-shape" resection.
Plane resection has been recommended for hypertrophies in which the upper pole is flat (Fig. 9). Posterior resection provides good results io hypertrophies with excess tissue on the upper pole (Fig. 1a). U-shape resection is the best choice for breast reduction in general.
Figs. 9a and 9b - Patient with mammary hypertrophy. There is no tissue on the upper pole.
Figs. 9c and 9d - 1 year after mammaplasty with plane resection.
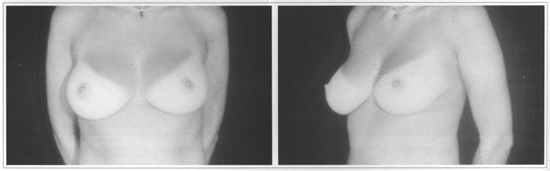
Figs. 10a and 10b - 25 year-old patient with mammary hypertrophy.
Figs. 10e and 10d - 5 years after reduction mammaplasty with posterior resection.
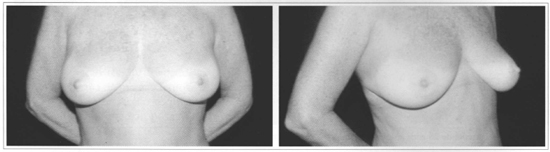
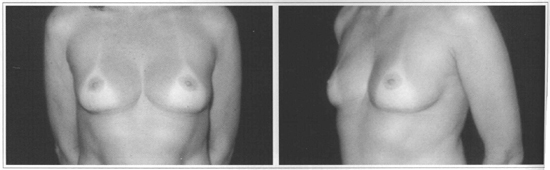
Figs. 11a and llb - Mammary hypertrophy and ptosis in a 37-year-old patient.
Figs. 11c and 11d - 4 years after reduction mammaplasry with "u-shape" resection.
DISCUSSION
There is a prevailing trend to reduce the final scar in mammaplasty. Plastic surgeons avoid long scars in any rype of surgery. When a woman asks for breast surgery, she wants to improve her appearance, and is not concerned about scars. They have never asked me about the length of the scar, but I have often been asked about its guality. Sometimes patients complain about the size or shape of their breasts. If it is necessary to increase the scar in order to have a better shape for the breasts, we should not worry about that, as no patient will ever complain. Every breast has the scar it deserves. In the plastic surgery clinic of the Hospital of the State University of Rio de Janeiro, over 4,000 reduction mammaplasties and mastopexies have been carried out in the period between 1974 and 2001. There is a high level of satisfaction and there have been few complaints.
We believe that Pitanguy's principles are state-of-the-art in mastopexy and in reduction mammaplasty. These principles are simple, feasible, easy to learn and may be used in any type of breast.
CONCLUSION
Frequent studies of levels of satisfaction, to complications, to changes in short and long-term results, and the opinion of patients allow us to say that the final aspect of the breasts is the most important requirement for breast reduction and mastopexy, while the length of the scar hardly matters (so long as it is of good quality). Patients are concerned with the guality of the scar rather than with its length.
REFERENCES
1. de Castro CC. The value of non-prefixed marking in reduction mammoplasty, Aesth Plast Surg. 1984;8(4):237-41.
2. de Castro CC. Mammaplasty with curved incisions. Plast Reconstr Surg. 1976;57(5):596-60
3. Aboudib Jr JH, de Castro CC. Mammaplasty utilizing the periareolar approach. Aesth Plast Smg. 1998;22:51-7.
4. Pontes R. Reduction mammaplasty - variations I and II. Ann Plast Surg. 1981;6:437-44.
5. Pitanguy L Surgical treatment of breast hypertrophy: Br J Plast Surg. 1967;20:78.
6. Lassus C. Breast reduction: evolution of a technique - a single scar. Aesth Plast Surg. 1987;11107-14.
7. Lejour M. Vertical mammaplasty and liposuction ofthe breast. Plast Reconstr Surg. 1994;94: 100-14.
8. Peixoto G. Reduction mammaplasty: a personal technigue. Plast Reconstr Surg. 1980;65:217.
9. Marchac D, Olarte G. Reduction mammaplasty and correction of ptosis with a short inframammary scar. Plast Reconstr Surg. 1982;69:45-54.
10. Graf MG, Auersvald A, Bernardes A, Biggs TM. Reduction mamrnaplasry and mastopeÀ)' with shorter scar and better shape. Aesth Surg J. 2000;20:99-106.
11. Pitanguy L. Evaluation of body conrouring surgery today: a 30-year experience. Plast Rcconstr Surg. 2000;105: 1499-514.
12. de Castro Cc. Late results after reduction mammaplasry with curved incisions. Plast Recoristr Surg. 1978;61(6) :862-7.
I - Associate Professor and Head of Plastic Surgery of the Hospital Pedro Ernesro of the Universidade do Estado do Rio de Janeiro. Senior Member of SBCP.
II - Master in Plastic Surgery Senior Member of SBCP.
Study performed at Hospital Universitário Pedro Ernesto - Universidade do Estado do Rio de Janeiro
Address for correspondence:
Claudio Cardoso de Castro, MD
R. Carlos Góis, 375/307
22440-040 - Rio de Janeiro - RJ Brazil
Phone: (5521) 2511-2242
e-mail: cdecastro@uol.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter