

Original Article - Year 2017 - Volume 32 -
Pressure ulcer treatment in the Pediatric Unit of a Rehabilitation Hospital
Tratamento cirúrgico de úlcera por pressão na unidade de Pediatria de hospital de reabilitação
ABSTRACT
INTRODUCTION: Pressure ulcers (PUs), or pressure sores, are among the most common serious complications in patients with spinal cord injury. The incidence and evolution in children and adolescents have specific characteristics. Most prior reports evaluated adults who developed PUs in the hospital. The objective is to describe the outcomes of surgical PU closure in children and adolescents in the Hospital Sarah Brasília pediatric unit.
METHODS: This was a retrospective statistical analysis of patients who underwent surgery for PUs. Statistical analysis of the incidence of PUs was performed using Epi Info version 3.2.2.
RESULTS: Of 116 patients who underwent surgery for PUs at the Hospital Sarah between 2005 and 2010, 20 (17.2%) were admitted to the Pediatric Unit. All 15 (75%) male and 5 (25%) female patients were admitted from a community setting. PUs were located in the ischial region in 60% of patients. The follow-up period was 15 years. Neural tube malformations were present in 70% of patients. We performed surgery for grade III and IV PUs, using gluteal flaps, primary closure and coccygectomy, and tensor fascia lata flaps. Three cases had complications, 65% developed recurrences, and 15% developed new ulcers in the pelvic region.
CONCLUSION: The main cause of PUs in pediatric cases admitted to the rehabilitation hospital was a neural tube malformation (70%) in the ischial region. Despite admission to the rehabilitation program, a high recurrence rate (65%) was observed.
Keywords: Pressure ulcer; Rehabilitation; Pediatrics; Neural tube; Sciatica.
RESUMO
INTRODUÇÃO: A úlcera por pressão (UPP) é uma das complicações mais comuns em portadores de lesão medular, dos mais graves e frequentes problemas destes pacientes. A incidência e evolução depende dos grupos estudados, tendo as crianças e adolescentes características específicas durante o crescimento. A maior parte das descrições na literatura referem-se a adultos que desenvolveram UPP durante internação. O objetivo é descrever os resultados de pacientes operados para fechamento de úlcera por pressão na unidade de Pediatria do Hospital Sarah Brasília.
MÉTODOS: Estudo descritivo, retrospectivo de pacientes operados de 2005 a 2010 devido à lesão por pressão e análise estatística.
RESULTADOS: 116 pacientes foram admitidos para tratamento cirúrgico de UPP no Hospital Sarah, sendo 20 (17,2%) internados na Pediatria; 15 (75%) homens e 5 (25%) mulheres, todos provenientes de ambiente comunitário; 60% localizadas na região isquiática; com seguimento de 15 anos; 70% eram portadores de malformação do tubo neural. Os procedimentos cirúrgicos foram indicados para úlcera por pressão grau III e IV. Utilizou-se retalho do músculo glúteo (3), em ilha (8) ou península (3), fechamento primário e coccigectomia; retalho do músculo tensor da fáscia lata. Três casos apresentaram complicações, 65% evoluíram com recidiva e 15% com surgimento de novas lesões na região pélvica.
CONCLUSÃO: A principal causa de lesão por pressão em Pediatria foi devido à malformação do tubo neural (70%), adquiridas na comunidade, localizadas na região isquiática. Embora estivessem em atendimento no programa de reabilitação, ainda foi observado alto índice de recidivas (65%).
Palavras-chave: Úlcera por pressão; Reabilitação; Pediatria; Tubo neural; Ciática.
Patients with spinal cord injury have many secondary complications. Pressure ulcers, or pressure sores, are among the most common and severe. These are defined as lesions affecting the skin and underlying tissue, and are caused by pressure, friction, and/or a combination of both1,2. Pressure ulcers are graded from I to IV, according to the degree of tissue involvement. It is estimated that 85% of patients with spinal cord injury will experience pressure ulcers during their lifetime.
McKinley et al.3 reported that pressure ulcers were the most common secondary complications in patients with spinal cord injury, with prevalence rates ranging from 15.2% at one year to 29.4% at 20 years after spinal cord injury. The occurrence in hospitalization services of spinal cord injury varies from 5 to 30%. The high medical costs associated with the treatment of pressure ulcers are proportional to their severity, because healing rates are slower for more severe ulcers. Moreover, severe ulcers are more likely to be complicated, requiring surgical procedures and a multidisciplinary team.
Several risk factors for the development of pressure ulcers, as well as preventive measures, have been described in the literature. Risk factors include neurological damage, low weight, anemia, smoking, urinary incontinence, lung disease, hypoalbuminemia, diabetes, impaired cognitive function, decreased mobility, greater age, spasticity, and renal disease, among others.
Despite extensive research and efforts to improve care, pressure ulcers remain an ongoing problem in hospitals. Surgical treatment of pressure ulcers includes debridement of devitalized tissue, primary closure, use of cutaneous grafts, muscle or myofunctional flaps, and the removal of bony prominences or ossifications4-9.
In the last five years, 109 articles were indexed in PubMed with the descriptors "pressure ulcer" and "children." The publications mainly discussed risk scoring for ulcer development, incidence, complications, preventive measures, and treatment options. However, diagnosis and comorbidities in children have specific characteristics, and are influenced by growth and development.
OBJECTIVE
To describe the outcomes of reconstructive surgery for pressure ulcers in the pediatric unit of a rehabilitation hospital.
METHODS
This was a retrospective study of patients who underwent surgery for pressure ulcers in the pediatric unit of the Hospital Sarah Brasília between January 2005 and December 2010. The study was approved by the Ethics Committee of the Hospital Sarah.
Inclusion criteria: age less than 17 years, admitted from a community setting for surgical treatment of pressure ulcers.
Preoperative evaluation
All patients underwent preoperative evaluation by a team of physicians, nurses, nutritionists, and physiotherapists. Sensorimotor mapping, nutritional assessment, renal function and urodynamic testing, liver function testing, imaging (radiography, fistulography, computed tomography, and magnetic resonance imaging), and culture of ulcer exudate with antibiograms were performed.
Functional musculoskeletal evaluation was performed in the movement laboratory, to assess the pattern of ambulation and mobility, and the need for orthoses, canes, or walkers. Overall physical condition, adequacy of physical therapy, and identification of risk factors for injuries were assessed. The need for surgery to correct lower limb deformities was evaluated.
Postoperative care
Supine positioning was performed for 6 weeks, with protection of elbows, hips, knees, ankles, and feet using pillows and mattresses. Physiotherapy was performed during this period to mobilize the knees, ankles, and feet. A bladder catheter was used for 15 days, with subsequent conversion to intermittent catheterization. Surgical drains (for aspiration) were removed after 4-7 days, and sutures were removed at 15 days.
After 6 weeks, patients were permitted to sit up and use a wheelchair, and were fitted for orthoses. They were evaluated for adaptation to new conditions, with instruction in repositioning to relieve pressure every 15 min, change of supine position every 2 h, use of air mattresses and wheelchair cushions, and self-inspection and skin care.
Operative technique
Patients were placed in the ventral decubitus position on an air mattress under general anesthesia. Prophylactic cefazolin and gentamicin were administered for 24 h preoperatively, with dosing according to renal function and/or antibiogram results. Thromboembolism prophylaxis was implemented. All surgeries were performed by a team of plastic surgeons, with assistance by an orthopedic surgeon in some cases. The pressure ulcers were injected with methylene blue and the entire ulcer and associated fistulas, as well as affected granulation tissue, adjacent fibrous tissue, bony prominences and heterotopic ossifications seen on preoperative imaging were excised.
The excision site was closed with muscle or myocutaneous flaps, and sutured in planes with Monocryl or Mono Nylon. A suction drain installation with a counter-opening closed system was applied. Use of latex was avoided in patients with myelomeningoceles or a history of latex allergy.
Variables studied: Sex, age, diagnosis, ulcer grade according to National Pressure Ulcer Advisory Panel criteria, surgical procedure, and postoperative course were recorded.
Statistical analysis: Epi Info 3.2.2. Frequency Analysis software was used.
RESULTS
Of 116 patients who underwent surgery for pressure ulcers at the Hospital Sarah Brasília, 20 (17.2%) were under 17 years old and were admitted to the Pediatric Unit. All 15 (75%) male and 5 (25%) female patients developed pressure ulcers in a community setting; 35% were from the Federal District and 65% from other Brazilian states (Table 1).
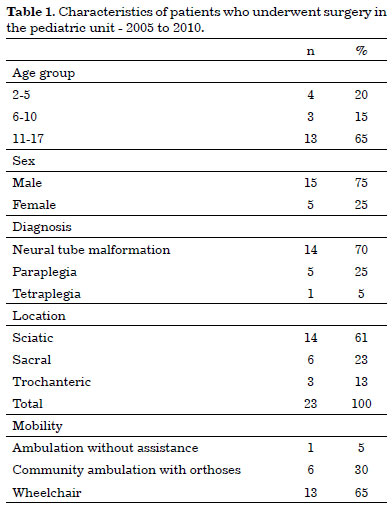
The distribution of the surgical cases is shown in Table 1. 65% were aged 11 to 17 years, 70% had neural tube malformations (lumbar and thoracic myelomeningocele), 25% had paraplegia (T8, 9, 12, and L1 levels), and 5% had spastic droplet tetraplegia. In 61% of cases, the ulcers were located in the sciatic region, with 26% over the sacrum and 13% over the trochanter. One patient was paraplegic, one was tetraplegic, and 3 patients had pressure ulcers in more than one site. A total of 23 procedures were performed for pressure ulcer closure (Figure 1).
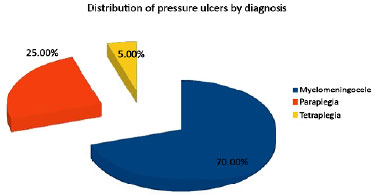
Figure 1. Distribution by diagnosis.
All patients had comorbidities, including neurogenic bladder and bowel, hip, knee, and foot deformities, and ulcers involving the feet and back. One case had heterotopic ossification, 5 had lower limb pressure injuries, and 5 had hip dislocations. All developed pressure ulcers in a community setting.
Mobility was impaired in 95%, with outpatient use of orthoses, canes, and wheelchairs (Table 1). Surgical procedures were performed for pressure ulcer grades III and IV, with prior surgical debridement in 3 cases. A gluteus muscle flap was used for closure in 3 cases, a myocutaneous gluteus island (Figure 2) flap in 8 cases, and a peninsular flap in 3 cases to close ischial pressure ulcers. Close to the muscle Gluteus and coccigectomy for sacral UPP in six and m. Tensor of the fascia lata to trochanteric region in three. Of 3 cases with complications, 2 had small areas of necrosis at the end of the flap, with healing by second intention, and one case developed an infection and subcutaneous fistula that resolved with dressing changes and decubitus care (Table 2).
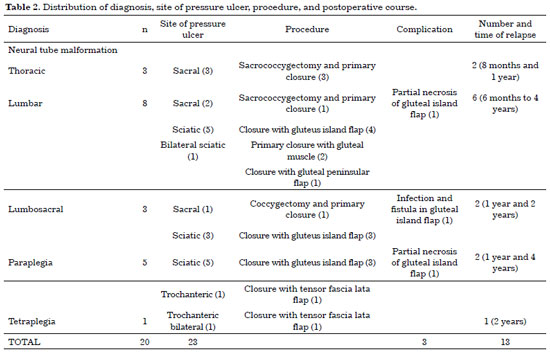

Figure 2. Preoperative appearance of pressure ulcer in the sciatic region; second postoperative week following use of gluteus island flap.
The minimum length of hospital stay for the surgical procedure was 8 weeks, with a maximum of 9 months for a patient with spastic quadriplegia. The mean follow-up time was 15 years. Patients with neural tube malformations admitted by the pediatrics team during the study period had an age range of 1 month to 17 years. These patients were followed up as outpatients, and presented with neurological, cutaneous, orthopedic, intestinal, and urinary disorders.
Orthopedic findings included spinal deformities, hip dislocations, and lower extremity osteoarticular contractures. These patients were evaluated and followed by the orthopedic team. Neurological changes reflected the most common areas of involvement in the lumbar and lumbosacral regions, with altered sensitivity, decreased reflexes and muscle strength, and muscle atrophy.
Of the 20 patients who underwent surgery for pressure ulcer closure, 65% had recurrences 1-4 years after surgery, 4 required reoperation, and 15% developed new pressure ulcers in the pelvic region (Figure 3).
Patients with neural tube defects had undergone prior surgical procedures for hydrocephalus with a ventriculoperitoneal (VP) shunt or medullary approach between 48 h and 30 days of age in another facility (only if neural tube repair was not performed).

Figure 3. Immediate postoperative appearance of pressure ulcer closure with gluteal island flap; relapse after 1 year.
A ventriculoatrial (VA) shunt was placed in 2 patients who lost VP shunts and laminectomy was performed for spinal cord release in 3 patients. Other interventions included treatment of neurogenic bladder, including use of botulinum toxin injections or cystoenteroplasty. Tendon elongation was performed, heterotopic ossifications were excised, and dressing changes and skin prophylaxis were performed in the 10% of patients with knee, calcaneal, and malleolar ulcers (Figure 4).
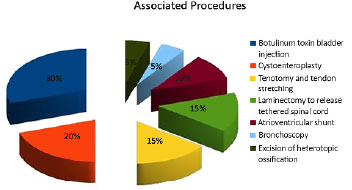
Figure 4. Distribution of associated procedures.
Latex exposure was avoided for those at risk of a reaction (Figura 5). Antibiotics, anticonvulsants, sedatives, anxiolytics, oxybutynin, anticoagulants, and other drugs were used.
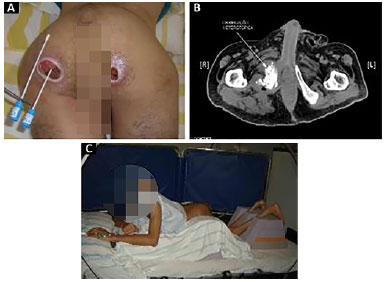
Figure 5. A: Preoperative evaluation of stage 4 pressure ulcer; B: Magnetic resonance imaging showing sciatic pressure ulcer with myositis ossificans; C: Mattress adaptation for postoperative prone positioning.
Patients were admitted to the outpatient clinic and referred to the rehabilitation program, with an emphasis on vesicoureteral reeducation. Urological examination was performed when intermittent bladder catheterization was discussed. Pathology was clarified and education for neurogenic bladder management was provided, followed by actual training in technique.
The rehabilitation nurse was responsible for caregiver education regarding the techniques of intermittent clean bladder catheterization and intestinal reeducation. Intestinal training used an individualized approach based on bowel habits and age and weight, with neurogenic bowel awareness classes, dietary reeducation, daily evacuation (after a large meal), rectal examination, and manual stool extraction.
These orientation classes were provided for the companion/caregiver. Adolescents received training in self-care. The approach to a child or adolescent was based on the age group. Even when a child or adolescent is independent for activities of daily living, the caregivers should remain available, as they are responsible for the supervision and/or completion of the procedure. Longitudinal follow-up was scheduled according to individual need and the availability of the interdisciplinary team, and was performed as an outpatient or during a new hospitalization.
DISCUSSION
Pressure ulcers are a global problem and many patients die from complications. The treatment of pressure injuries is a major healthcare challenge. The incidence, prevalence, and recurrence rate depend on several factors, including the etiology, presence of spinal cord injury, and the association with comorbidities. This study found a higher prevalence of neural tube malformations (70%) in association with comorbidities (100%)1-9.
The analysis of children and adolescents admitted to the rehabilitation hospital for surgical treatment of pressure ulcers found that all lesions had developed in a community setting. The reported annual prevalence rate of pressure ulcers and other types of skin disruption in individuals of all ages with neural tube defects is 15-77%; the rate in adults is 34%, i.e., higher than the rate in the general population10,11. This study only evaluated cases that required surgical closure; these averaged 3 cases per year.
Neural tube malformations are the second most common neurologic disorders in childhood, after cerebral palsy. Their management is complex and requires multidisciplinary follow-up throughout life. Delayed neuropsychomotor development can be assessed early, based on head, chest, and motor development, especially when associated with hydrocephalus, which was present in 60% of the cases in this study, although controlled by the use of shunts.
An estimated 47% of hospital admissions in patients with neural tube malformations are for preventable conditions, such as urinary infections, kidney stones, pressure ulcers, and osteomyelitis. In studies of patients with neural tube defects, neurogenic intestine and bladder were identified as the main reasons for hospitalization, in addition to changes in mobility and the development of pressure lesions10-12.
Neurogenic bladder and neurogenic gut mainly occur in diseases associated with bone marrow injury. Following hospital admission, patients and caregivers were instructed in skin care, intermittent clean bladder catheterization, and bowel evacuation techniques. The manifestations and consequences of neural tube malformations first present in infants and children, depending on the type and level of spinal cord injury.
These are classified as thoracic, lumbar, or lumbosacral malformations, depending on the neurological level, and can present with deformities that define the need for orthoses, canes, or a wheelchair, as observed in 95% of the cases in this study. Orthoses and adaptations should be evaluated regularly during growth, as they may lead to injuries when a child drags the feet or remains in a wheelchair for prolonged periods12-17.
In general, thoracic and lumbar lesions, seen in 11 cases, are generally associated with greater paralysis and sensory loss, which may explain the higher rates of limb deformities, wheelchair use, and the occurrence of pressure injuries with a high recurrence rate, as observed in this study. Wheelchair use, prolonged sitting, immobility, urinary incontinence, and male sex were associated with a higher incidence of pressure ulcers18-21.
Although the children admitted to the hospital rehabilitation program had been followed since infancy for a mean duration of 15 years before the onset of ulcers, they were instructed in skin care and adaptations for locomotion. Patients aged 11 to 17 years (60%) had pressure ulcers requiring surgery. This age group is at high risk for development of pressure ulcers according to the Braden scale22.
The Braden scale comprises 6 dimensions: sensory perception, moisture, activity, mobility, nutrition, and friction and shear forces, all contributing to the development of pressure ulcers. In addition, data from the literature have shown that approximately 50% of young people with chronic disease do not comply with therapeutic recommendations23.
Adolescents with chronic disease need to feel supported by family members, especially when they have associated cognitive deficits, such as those evaluated in this study. Chronic disease permanently affects an adolescent's life and may affect social relationships, school performance, and sexual behavior24.
The great challenge for the plastic surgeon in the multidisciplinary team is to determine the level of the lesion and to determine the feasibility of performing muscle flaps. When the patient is a community ambulator with the use of orthoses, and the gluteus muscle exhibits adequate strength, its use should be avoided, as this may contribute to worsening limb mobility. Interventions throughout the rehabilitation process must include evaluation of positioning and injuries to feet and other locations, dressing placement, the need for debridement, and the timing of surgery.
This study used the gluteus muscle for filling and bone protection, with or without muscle detachment, using an island or peninsular flap. The gluteus was used when no muscle force could be elicited or the patient was not ambulatory. Tensor fascia lata flaps were used in patients with trochanteric pressure ulcers, as observed in paraplegic and quadriplegic patients.
This study observed complications of surgical closure in 15% of cases. Infection and partial flap necrosis mainly occurred after closure of ischial pressure ulcers; these healed with second intention or dressing changes. Figueiras25 described the surgical treatment of pressure ulcers in 17 mainly adult patients, noting that the most prevalent location was the sacrum. These ulcers developed in a hospital setting in 82% of cases, and required a variety of surgical procedures, with a complication rate of 39%.
Souza Filho et al.26 analyzed 38 procedures performed for pressure ulcer closure over a 3-year period. These predominated in the sacral and trochanteric regions. The complication rate due to dehiscence was 36.8%, and 60% of ischial ulcers recurred in paraplegic patients.
Even with care in a rehabilitation center, including positioning, orthopedic and urological procedures, and prophylactic adaptations in all cases, recurrences occurred in 13 (65%) of the cases at 1-4 years after surgery. Four cases underwent reoperation using more complex flaps, and the others were managed with outpatient follow-up, dressings, and positioning.
The reported relapse rate ranges from 20 to 80%, according to the ulcer site and diagnosis, among other factors. In a report from hospitals in the Federal District, among 140 patients who underwent surgery in a 9-year period, 1.5% had an underlying myelomeningocele. Complications included dehiscence in 6%, hematoma in 5%, surgical site infection in 2%, and partial necrosis in 2%; the ulcer recurrence rate was 33.18%27.
Patients with neural tube defects had the highest prevalence of pressure ulcers in this study; the ulcers were acquired in a community setting, and the relapse rate was 65%. Follow-up, evaluation, and intervention in this group are essential, since the mortality due to complications related to neural tube malformations is high in childhood and adolescence; however, 90% of these patients now reach adulthood, thanks to advances in health care16,17.
CONCLUSION
This study observed that pediatric unit admissions accounted for 17% (20) of hospitalizations for pressure injuries in a rehabilitation hospital during a 5-year period. All patients developed pressure ulcers in a community setting and had associated comorbidities, 75% were male, and 70% had neural tube malformations, with pressure lesions located mainly in the sciatic region. Surgical closure was performed using muscle flaps. Lesions recurred in 65% of cases and 15% developed pressure ulcers at new sites in the pelvic region.
It is important to note that despite admission and follow-up in a rehabilitation program since early childhood, the relapse rate was still high. We emphasize the importance of continued follow-up with a multidisciplinary team throughout childhood and adolescence in patients with spinal cord defects.
COLLABORATIONS
KTB Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents.
ICCP Conception and design of the study; writing the manuscript or critical review of its contents.
ACLR Analysis and/or interpretation of data; writing the manuscript or critical review of its contents.
REFERENCES
1. European Pressure Ulcer Advisory Panel. 2007 [acesso 2016 mar 7]. Disponível em: http://www.epuap.org/gltreatment.html
2. Noreau L, Proulx P, Gagnon L, Drolet M, Laramée MT. Secondary impairments after spinal cord injury: a population-based study. Am J Phys Med Rehabil. 2000;79(6):526-35. PMID: 11083303 DOI: http://dx.doi.org/10.1097/00002060-200011000-00009
3. McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ. Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil. 1999;80(11):1402-10. PMID: 10569434 DOI: http://dx.doi.org/10.1016/S0003-9993(99)90251-4
4. Langemo DK, Melland H, Hanson D, Olson B, Hunter S. The lived experience of having a pressure ulcer: a qualitative analysis. Adv Skin Wound Care. 2000;13(5):225-35.
5. Hopkins A, Dealey C, Bale S, Defloor T, Worboys F. Patient stories of living with a pressure ulcer. J Adv Nurs. 2006;56(4):345-53. PMID: 17042814 DOI: http://dx.doi.org/10.1111/j.1365-2648.2006.04007.x
6. Bennett G, Dealey C, Posnett J. The cost of pressure ulcers in the UK. Age Ageing. 2004;33(3):230-5. PMID: 15082426 DOI: http://dx.doi.org/10.1093/ageing/afh086
7. Bergstrom N, Bennett MA, Carlson CE. Treatment of Pressure Ulcers. Clinical Practice Guideline No. 15. Rockville, Md: US Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; 1994. AHCPR Publication No. 95-0652.
8. Allcock N, Wharrad H, Nicolson A. Interpretation of pressuresore prevalence. J Adv Nurs. 1994;20(1):37-45. DOI: http://dx.doi.org/10.1046/j.1365-2648.1994.20010037.x
9. Anthony D. Understanding Advanced Statistics: A Guide for Nurses and Health Care Researchers. Edinburgh: Churchill Livingstone; 1999.
10. Bowman RM, McLone DG, Grant JA, Tomita T, Ito JA. Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg. 2001;34(3):114-20. PMID: 11359098 DOI: http://dx.doi.org/10.1159/000056005
11. Kim S, Ward E, Dicianno BE, Clayton GH, Sawin KJ, Beierwaltes P, et al. Factors associated with pressure ulcers in individuals with spina bifida. Arch Phys Med Rehabil. 2015;96(8):1435-41. DOI: http://dx.doi.org/10.1016/j.apmr.2015.02.029
12. Vogel LC, Krajci KA, Anderson CJ. Adults with pediatric-onset spinal cord injury: part 2: musculoskeletal and neurological complications. J Spinal Cord Med. 2002;25(2):117-23. DOI: http://dx.doi.org/10.1080/10790268.2002.11753611
13. Dalyan M, Cardenas DD, Gerard B. Upper extremity pain after spinal cord injury. Spinal Cord. 1999;37(3):191-5. PMID: 10213328 DOI: http://dx.doi.org/10.1038/sj.sc.3100802
14. Dicianno BE, Kurowski BG, Yang JM, Chancellor MB, Bejjani GK, Fairman AD, et al. Rehabilitation and medical management of the adult with spina bifida. Am J Phys Med Rehabil. 2008;87(12):1027-50. PMID: 18923330 DOI: http://dx.doi.org/10.1097/PHM.0b013e31818de070
15. Shin M, Besser LM, Siffel C, Kucik JE, Shaw GM, Lu C, et al.; Congenital Anomaly Multistate Prevalence and Survival Collaborative. Prevalence of spina bifida among children and adolescents in 10 regions in the United States. Pediatrics. 2010;126(2):274-9. DOI: http://dx.doi.org/10.1542/peds.2009-2084
16. Burke R, Liptak GS; Council on Children with Disabilities Providing a primary care medical home for children and youth with spina bifida. Pediatrics. 2011;128(6):e1645-57. PMID: 22123894 DOI: http://dx.doi.org/10.1542/peds.2011-2219
17. Young NL, Sheridan K, Burke TA, Mukherjee S, McCormick A. Health outcomes among youths and adults with spina bifida. J Pediatr. 2013;162(5):993-8. PMID: 23164316 DOI: http://dx.doi.org/10.1016/j.jpeds.2012.10.042
18. Martins G, Soler ZA, Batigalia F, Moore KN. Clean intermittent catheterization: educational booklet directed to caregivers of children with neurogenic bladder dysfunction. J Wound Ostomy Continence Nurs. 2009;36(5):545-9. PMID: 19752666 DOI: http://dx.doi.org/10.1097/WON.0b013e3181b41301
19. Segal ES, Deatrick JA, Hagelgans NA. The determinants of successful self-catheterization programs in children with myelomeningoceles. J Pediatr Nurs. 1995;10(2):82-8. DOI: http://dx.doi.org/10.1016/S0882-5963(05)80002-8
20. Lindehall B, Abrahamsson K, Jodal U, Olsson I, Sillén U. Complications of clean intermittent catheterization in young females with myelomeningocele: 10 to 19 years of followup. J Urol. 2007;178(3 Pt 1):1053-5. DOI: http://dx.doi.org/10.1016/j.juro.2007.05.071
21. de Azevedo RV, Oliveira EA, Vasconcelos MM, de Castro BA, Pereira FR, Duarte NF, et al. Impact of an interdisciplinary approach in children and adolescents with lower urinary tract dysfunction (LUTD). J Bras Nefrol. 2014;36(4):451-9. DOI: http://dx.doi.org/10.5935/0101-2800.20140065
22. Braden scale for predicting pressure sore risk. [acesso 2016 Jun 1]. Disponível em: http://www.bradenscale.com/images/bradenscale.pdf
23. KyngAs HA, Kroll T, Duffy ME. Compliance in adolescents with chronic diseases: a review. J Adolesc Health. 2000;26(6):379-88.
24. Berntsson L, Berg M, Brydolf M, Hellström AL. Adolescents' experiences of well-being when living with a long-term illness or disability. Scand J Caring Sci. 2007;21(4):419-25. PMID: 18036004 DOI: http://dx.doi.org/10.1111/j.1471-6712.2006.00490.x
25. Figueiras RG. Tratamento cirúrgico de úlceras por pressão: experiência de dois anos. Rev Bras Cir Plást. 2011;26(3):418-27. DOI: http://dx.doi.org/10.1590/S1983-51752011000300010
26. Souza Filho MVP, Cardoso DP, Girão RA. Tratamento cirúrgico das úlceras de pressão com retalhos cutâneos e musculocutâneos. Experiência de três anos no Hospital Geral Dr. Waldemar de Alcântara. Rev Bras Cir Plást. 2009;24(3):274-80.
27. Santos CP, Silva LM, Botelho DL, Silva RV, Machado CR, Almeida FPR. Úlceras de pressão: epidemiologia do Hospital Regional da Asa Norte - Distrito Federal. Rev. Bras Cir Plást. 2011;26(3 Suppl 1):11.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Universidade de Brasília, Brasília, DF, Brazil
3. Hospital Sarah Brasília, Brasília, DF, Brazil
4. Rede Sarah de Hospitais do Aparelho Locomotor, Brasília, DF, Brazil
Institution: Rede Sarah de Hospitais de Reabilitação, Brasília, DF, Brazil.
Corresponding author:
Katia Torres Batista
SMHS - Quadra 301 - Bloco A
Brasília, DF, Brazil - Zip Code 70335-901
E-mail: katiatb@terra.com.br
Article received: November 3, 2016.
Article accepted: September 23, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter