

Original Article - Year 2017 - Volume 32 -
Umbilicoplasty by vertical incision: description of the technique and assessment of satisfaction
Umbilicoplastia por incisão vertical: descrição da técnica e avaliação da satisfação
ABSTRACT
INTRODUCTION: The abdomen is an important aesthetic functional segment in the characterization of the body contour. In abdominoplasty, the placement and shape of the umbilical scar are important for a satisfactory result. This study aimed to describe the technique of vertical omphaloplasty and to present the results obtained.
METHODS: Retrospective longitudinal descriptive study composed of patients who underwent vertical omphaloplasty during classic abdominoplasty between 2014 and 2017. The technique consists of a vertical transcutaneous incision without removal of the skin spindle and with minimal degreasing of the wall around the umbilicus, followed by the transfixing a point in the lateral portion of the umbilical pedicle, allowing its invagination and fixation close to the aponeurosis of the rectus abdominis.
RESULTS: In the 128 patients evaluated, the patients' age ranged from 25 to 62 years, with a mean of 32 years. The mean time of surgery was 2 h and 33 min. No surgical complications occurred, such as hematoma or abdominal flap necrosis. Two cases of dehiscence, four cases of hypertrophic scar, two cases of stenosis, and one case of umbilical necrosis were observed. In outpatient follow-up, 92.2% of the patients were very satisfied with the final result. The technical analysis presented an 88% degree of satisfaction.
CONCLUSION: The technique described presents satisfactory results, reduces the possibility of the appearance of a cicatricial ring, and allows minimizing one of the stigmas of abdominoplasty, which is a very visible umbilical scar.
Keywords: Umbilicus; Abdominoplasty; Patient satisfaction; Cicatrix, hypertrophic; Abdomen.
RESUMO
INTRODUÇÃO: O abdome é um segmento estético-funcional importante na caracterização do contorno corporal. Na abdominoplastia, o posicionamento e o formato da cicatriz umbilical são importantes para um resultado satisfatório. Este estudo teve como objetivo descrever a técnica de onfaloplastia vertical, bem como apresentar os resultados obtidos.
MÉTODOS: Estudo longitudinal retrospectivo descritivo composto por pacientes submetidos à onfaloplastia vertical durante a abdominoplastia clássica no período de 2014 a 2017. A técnica consistiu em uma incisão linear vertical transcutânea sem retirada de fuso de pele e com mínimo desengorduramento da parede ao redor do umbigo, seguida da confecção de um ponto na porção lateral do pedículo umbilical, transfixante, permitindo sua invaginação e fixação rente à aponeurose do reto abdominal.
RESULTADOS: Do total de 128 pacientes avaliados, a faixa etária variou de 25 a 62 anos, com média de 32 anos. O tempo médio do ato operatório foi de 2 horas e 33 minutos. Não foram observadas complicações cirúrgicas como hematoma ou necrose do retalho abdominal. Foram observados 2 casos de deiscências, 4 casos de cicatriz hipertrófica, com 2 evoluindo para estenose umbilical e 1 caso de necrose umbilical. No seguimento ambulatorial 92,2% dos pacientes mostraram-se muito satisfeitos com o resultado final obtido. A análise técnica apresentou um grau de satisfação de 88,8% dos casos.
CONCLUSÃO: A técnica descrita apresenta resultados satisfatórios, diminui a possibilidade do surgimento do anel cicatricial e permite minimizar um dos estigmas da abdominoplastia, que é uma cicatriz umbilical muito visível.
Palavras-chave: Umbigo; Abdominoplastia; Satisfação do paciente; Cicatriz hipertrófica; Abdome.
The abdomen is an important aesthetic functional segment in the characterization of the body contour. Abdominoplasty is one of the most frequent surgeries among aesthetic procedures, and its performance restores the smoothness and jovial appearance of the abdomen1,2.
The poor preparation of the umbilical scar on the abdominal wall can compromise the result of abdominoplasty, producing visible and unnatural scarring. The purpose of this procedure was to externalize the umbilical scar in the most natural and satisfying way possible3.
The umbilicus has many forms, and the most common is a rounded form, with a deeper portion in the upper part, which is bordered by a cutaneous ridge. In its central portion, pronounced as the nipple or mamelão, is a vestige of the scar of the umbilical cord. Circling the mamelon is a circular depression called the umbilical sulcus4.
Several omphaloplasty techniques are found in the medical literature, and the most important features in the aesthetics of the result include location, shape, size, and scar invisible to the umbilical scar, besides the soft concavity in the periumbilical region, which has an aesthetic importance in the anterior abdominal wall5,6.
OBJECTIVE
Thus, this study aimed to describe the technique of vertical omphaloplasty without skin spindle removal and to present the results obtained with the use of this technique and patient satisfaction with this procedure.
METHODS
This is a longitudinal retrospective descriptive study developed from January 2014 to April 2017 by the Plastic Surgery Service of Daher Hospital in Brasília.
The research project followed the legal procedures determined by Resolution 196/96 of the National Health Council with regard to research involving human beings.
The Informed Consent Term (TCLE) in the study was obtained from all patients who underwent the surgical procedure.
The sample was of the intentional type and based on the profiles of patients who underwent classic abdominoplasty from January 2014 to April 2017 by a single senior surgeon. The database for the development of this research was based on the medical records of the patients and collected by the authors of the study.
The variables evaluated were sex, age, time of surgery, postoperative surgical complications, weight of the surgical specimen, body mass index (BMI), length of hospital stay, and satisfaction of the medical staff and patient with the scars and with the surgical procedure.
All patients undergoing classic abdominoplasty were included during the study period. Patients were submitted to abdominoplasty at anchor and/or who refused to participate in the study.
Surgical technique
The surgical team consisted of the senior surgeon and an assistant surgeon.
The preoperative marking of the abdominoplasty was performed with the patient in an orthostatic position, sitting, and lying in the dorsal position.
Initially, the abdominal flap was infiltrated with a solution of 0.9% saline and adrenaline in a 1:500,000 ratio. Subsequently, classic abdominoplasty was performed with detachments of the dermogordotic flap, release of the umbilical pedicle, and manufacture of the supra-umbilical tunnel until the xiphoid appendix. When indicated, plication of the rectus abdominis muscles was performed, with constant care being taken to preserve the midline umbilical scar.
At the stage of omphaloplasty, the umbilical scar was remodelled, and the surplus skin was removed to leave a vertical skin spindle. Skin could be left in the spindle, depending on the thickness of the adipose tissue of the abdominal flap. The lateral fixation of the umbilicus was performed with a U-shaped, transumbilical suture as in the technique of Chia et al7.
Suturing was performed with a 3-0 nylon thread that included the aponeurosis of the rectus abdominis, on the lateral portion of the umbilical pedicle, followed by transfixation of the inner portion of the umbilicus, and fixation of the aponeurosis of the rectus abdominis contralateral to the beginning of the suture, resuming the same suture steps described above, ending in the same closure to the place of the beginning of the procedure. The purpose of this transfixation point was to create a depth in the umbilical scar and thus establish its concavity by restoring a harmony in the abdominal segment (Figures 1, 2, 3 and 4).
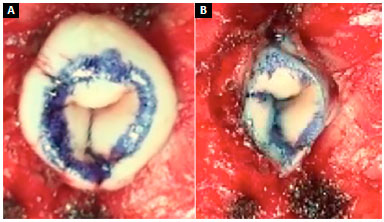
Figure 1. A: Marking for removal of the vertical skin spindle; B: Final appearance.
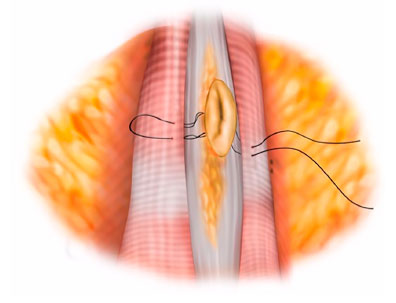
Figure 2. Illustration demonstrating the transfixing "U" suture technique.

Figure 3. Illustration demonstrating the transcutaneous vertical linear incision without skin spindle removal.

Figure 4. Illustration demonstrating the final appearance of the umbilical scar.
To mark the umbilical scar in the rectus abdominis, umbilicus-marking tweezers or digitopression was used to determine its position on the skin. At this site, a 1.5-cm transcutaneous vertical incision was performed without removal of the spindle, which allowed the skin to advance to deepen the scar and make it less apparent.
Another important point was the maintenance of a fat cushion around the incision, which in our understanding helps give depth to this umbilical scar, and its degreasing, as described by other authors, in our opinion can cause a result as an umbilicus. Subsequently, the umbilical pedicle was fixed with sub-dermal suture in the abdominal flap, initially in the cranial and caudal portions of the vertical incision, followed by the umbilical suture with single stitches with a 4-0 nylon thread, which were removed 28 days postoperatively.
Assessment of the satisfaction degree
The evaluation of the degree of satisfaction of the patients with the final result obtained was described in the medical record.
The technical evaluation of the result was performed by a plastic surgeon who was a member of the Brazilian Society of Plastic Surgery (and who had not participated in the surgical procedures) through a comparative analysis of the preoperative and one-year postoperative photographs.
Statistical analysis
The results were organized in Microsoft Excel 2008 spreadsheets and analyzed in Epi Info programs, version 3.5.1. A descriptive analysis of the data was performed, presenting the frequencies.
RESULTS
We analyzed 128 patients who underwent classic abdominoplasty. Of these, 16 were men and 112, women (Table 1).
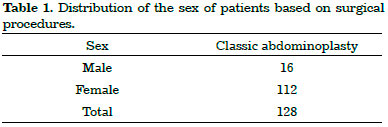
The patients' age ranged from 25 to 62 years, with a mean of 32 years.
The mean BMI of the patients was 26.6 kg/m2.
The mean time of classic abdominoplasty was 2 h and 3 min. The hospitalization time in all cases was 24 h.
The weight of the surgical parts of the abdomen ranged from 680 g to 4.34 kg, with a mean of 3.02 kg.
In our series, we observed two cases of umbilical scar suture dehiscence (treated on an outpatient basis), four cases of hypertrophic scarring (one case surgically corrected) with two cases of stenosis (and one surgically corrected case), and one case of umbilical necrosis.
No surgical complications were observed, such as hematoma or necrosis of the abdominal flap (Table 2).
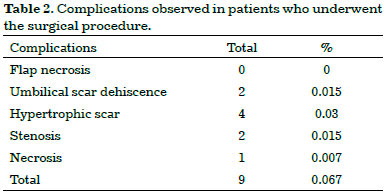
In the outpatient follow-up, 92.2% of the patients were very satisfied with the final result obtained from the omphaloplasty, and did not have complaints regarding the size and position of the scars. The technical evaluation by the evaluating surgeon showed an 88% degree of satisfaction with the final result and the positioning of the scars.
The figures below illustrate some cases of this study (Figures 5, 6, 7, 8, and 9).

Figure 5. A male patient who underwent vertical omphaloplasty. A: Preoperative view; B: 2-year post-operative aspect.
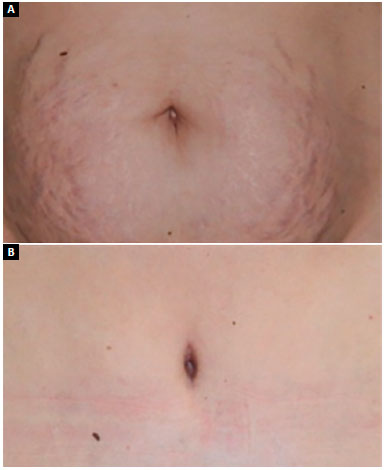
Figure 6. A female patient who underwent vertical omphaloplasty. A: Preoperative view; B: 1-year postoperative view.
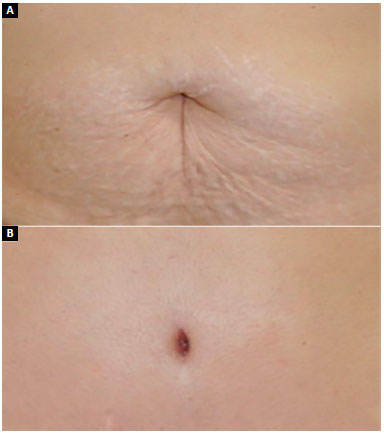
Figure 7. A female patient who underwent vertical omphaloplasty. A: Preoperative view; B: 6-months postoperative view.
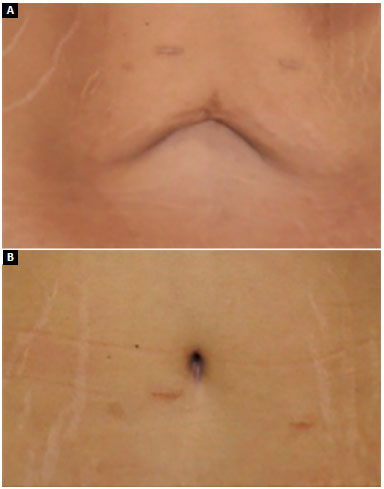
Figure 8. A female patient who underwent vertical omphaloplasty. A: Preoperative view; B: 1-year postoperative view.

Figure 9. A male patient who underwent vertical omphaloplasty presenting stenosis.
DISCUSSION
In abdominoplasty, adequate positioning of the umbilical scar is fundamental for a satisfactory result8.
The first abdominoplasties were performed in 1880, in France, by Demars and Marx. In 1899, Kelly described his technique in the United States. In 1921, Frist performed the first transposition of the umbilicus in abdominoplasty using the circular form for the procedure. Flesch, Thebesius, and Weisheimer, in 1931, retained a triangle of the distal base of the skin at the umbilicus9,10.
Vernon, in 1957, returned to circular forms; however, he obtained many cases of stenosis. Pitanguy, in 1967, advocated a curve incision of the cranial concavity for the treatment of the umbilicus in abdominoplasty. Baroudi published the umbilicoplasties he performed in 1975, and Avelar published in 1976 the three-point star technique to prevent cicatricial retractions with a triangular resected belly button and the incised abdominal "Y" flap. Daher, in 2011, published the minicírculo skin technique, which obtained satisfactory aesthetic results and no case of stenosis11,12.
Several geometric forms in the treatment of the umbilical scar, such as "Mercedes" star, diamonds, ellipses, crosses, clovers, rectangles, shield, symbol of infinity, and double "V," were described by authors, such as Ribeiro, Viterbo, and Saldanha13,14.
However, regardless of the technique chosen for performing omphaloplasty, the umbilicus should have an oval shape, with a vertical orientation similar to the natural umbilicus found in young and non-obese women.
In our series, the systematization of the presented technique has fulfilled the objective of presenting the umbilicus naturally in the postoperative period, which is similar to that of young and non-obese women, obtaining a longitudinal aspect.
According to some authors, the preparation of the "ideal umbilicus" should follow the following precepts: the circular scar should be avoided so that no posterior stenosis occurs and the umbilical peduncle must be fixed to the aponeurosis to conceal the scar and determine a greater depth14,15. In our understanding, one should also preserve the periumbilical fatty cushion to maintain this depth.
In our technique we try to adopt all the necessary precepts for the creation of the "ideal umbilicus." The exteriorization of the neoumbigo by a vertical transcutaneous incision in our series showed satisfactory results both by the patient (92.2%) and by the technical evaluation (88.8%).
The difference of satisfaction between the patient and surgeon may be related to subjective satisfaction by the patients because they are satisfied with the overall aesthetic improvement of the abdomen after abdominoplasty.
The review of the literature showed that non-circular techniques of omphaloplasty prevented the appearance of a scar ring with umbilical scar deformity, whereas circular techniques favored greater stenosis of the neoumbigo16.
In our series, two cases of stenosis (0.015%) were observed using the described technique. We obtained two cases of dehiscence of umbilical scar suture (0.015%), four cases of pathological scarring (0.03%), and one case of umbilicus necrosis, and the results were similar to studies found in the literature.
Vertical omphaloplasty without skin spindle removal represents an intermediate technique between circular and non-circular because its final shape is linear and vertical, reducing the possibility of the appearance of the cicatricial ring, thus it can probably minimize the stigma of the abdominoplasty, with very visible umbilical scar.
Saldanha stated that the non-degreasing of the abdominal wall around the umbilicus prevented the visualization of the umbilical scar, giving the umbilicus a natural appearance17.
We agree with the author; however, we believe that the non-removal of the skin spindle will allow the advancement of the same with the traction of the neoumbigo, thus leaving a deeper and less apparent scar.
CONCLUSION
The results obtained by this technique proved to be satisfactory and reaffirm our intention to hide the scar, keeping it at the bottom of the umbilical depression. The details of obtaining its natural invagination and easy execution were also added.
COLLABORATIONS
DBP Final approval of the manuscript; completion of surgeries and/or experiments.
DASS Statistical analyses; conception and design of the study; writing the manuscript or critical review of its contents.
MCC Analysis and/or interpretation of data.
LMCD Analysis and/or interpretation of data.
MCAG Analysis and/or interpretation of data.
GCS Analysis and/or interpretation of data.
LDPB Analysis and/or interpretation of data.
JCD Final approval of the manuscript.
REFERENCES
1. Dini GM, Ferreira LM. Putting the umbilicus in the midline. Plast Reconstr Surg. 2007;119(6):1971-3. PMID: 17440407 DOI: http://dx.doi.org/10.1097/01.prs.0000259800.70743.3c
2. Vico PG, De Vooght A, Nokerman B. Circumferential body contouring in bariatric and non-bariatric patient. J Plast Reconstr Aesthet Surg. 2010;63(5):814-9. DOI: http://dx.doi.org/10.1016/j.bjps.2009.01.075
3. Schoeller T, Wechselberger G, Otto A, Rainer C, Schwabegger A, Lille S, et al. New technique for scarless umbilical reinsertion in abdominoplasty procedures. Plast Reconstr Surg. 1998;102(5):1720-3. PMID: 9774037 DOI: http://dx.doi.org/10.1097/00006534-199810000-00064
4. Jaimovich CA, Mazzarone F, Parra JFN, Pitanguy I. Semiologia da Parede Abdominal: Seu Valor no Planejamento das Abdominoplastias. Rev Bras Cir Plást.1999;14(3):21-50.
5. Avelar J. Abdominoplasty-Systematization of a technique without external umbilical scar. Aesthetic Plast Surg. 1978;2(1):141-51. DOI: http://dx.doi.org/10.1007/bF01577947
6. Rohrich RJ, Sorokin ES, Brown SA, Gibby DL. Is the umbilicus truly midline? Clinical and medicolegal implications. Plast Reconstr Surg. 2003;112(1):259-63. DOI: http://dx.doi.org/10.1097/01.PRS.0000066367.41067.C2
7. Chia CY, Roxo ACW, Labanca L, Ritter PD. Cirurgia estética e funcional do umbigo: técnica de plicatura transumbilical. Rev Bras Cir Plást. 2011;26(2):293-7. DOI: http://dx.doi.org/10.1590/S1983-51752011000200017
8. Dias Filho AV, Valadão MGC, Guerra Filho TR, Moura RMG. Onfaloplastia: estudo comparativo de técnicas. Rev Bras Cir Plást. 2014;29(2):253-8.
9. Hakme F. Evolução histórica das abdominoplastias e contribuição pessoal. In: Anais do Simpósio Brasileiro de Abdominoplastias. São Paulo: Sociedade Brasileira de Cirurgia Plástica; 1982. p. 3-8.
10. Bozola AR, Bozola AC. Abdominoplastias. In: Mélega JM, ed. Cirurgia plástica: fundamentos e arte. Cirurgia Estética. Rio de Janeiro: Medsi; 2003. p. 609-28.
11. Sinder R. Abdominoplastias. In: Carreirão S, Cardim V, Goldenberg D, ed. Cirurgia Plástica. São Paulo: Atheneu; 2005.
12. Daher JC, Benedik A, Faria CADC, Amaral JDLG, Rodrigues Neto JN, Cosac OM, et al. Umbilicoplastia: experiência com a técnica do minicírculo de pele. Rev Bras Cir Plást. 2011;26(2):302-5.
13. Saldanha OR, De Souza Pinto EB, Mattos WN Jr, Pazetti CE, Lopes Bello EM, Rojas Y, et al. Lipoabdominoplasty with selective and safe undermining. Aesthetic Plast Surg. 2003;27(4):322-7. PMID: 15058559 DOI: http://dx.doi.org/10.1007/s00266-003-3016-z
14. Furtado IR. Onfaloplastia: técnica "infinito". Rev Bras Cir Plást. 2011;26(2):298-301.
15. Mello DF, Yoshino H. Plicatura da base umbilical: proposta técnica para tratar protrusões e evitar estigmas pós-abdominoplastia Rev Bras Cir Plást. 2009;24(4):525-9
16. Malic CC, Spyrou GE, Hough M, Fourie L. Patient satisfaction with two different methods of umbilicoplasty. Plast Reconstr Surg. 2007;119(1):357-61. PMID: 17255693 DOI: http://dx.doi.org/10.1097/01.prs.0000244907.06440.f8
17. Castro DPR, Saldanha OR, Pinto EBS, Albuquerque FM, Moia SMS. Avaliação estética da cicatriz umbilical em duas técnicas de onfaloplastia. Rev Bras Cir Plást. 2014;29(2):248-52.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Daher Lago Sul, Brasília, DF, Brazil
Institution: Hospital Daher Lago Sul, Brasília, DF, Brazil.
Corresponding author:
Diogo Borges Pedroso
SEP SUL, 709/909 LT. A Loja S20, Praça Central, Asa Sul
Brasília, DF, Brazil - Zip Code 70390-095
E-mail: dpedroso@gmail.com
Article received: May 9, 2017.
Article accepted: September 17, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter