

Original Article - Year 2017 - Volume 32 -
Breast reconstruction with reverse mini abdominoplasty
Reconstrução de mama com miniabdominoplastia reversa
ABSTRACT
INTRODUCTION: Mastectomy is very traumatic for women, and breast reconstruction is an essential procedure to improve their psychosocial well-being and quality of life. Most plastic surgeons do not perform breast reconstruction. This practice requires advanced training with a long learning curve. Breast reconstruction using excess flaps in reverse abdominoplasty can be a practical option and of great applicability in carefully selected patients.
METHODS: From August 2014 to June 2016, 12 patients underwent breast reconstruction using the reverse mini abdominoplasty technique. Symmetrization was performed in six patients who underwent unilateral reconstruction, with one case reconstructed bilaterally. The implants were placed in the supra-muscular plane and in a submuscular position in seven and five patients, respectively.
RESULTS: There was one case each of seroma, epitheliolysis, and partial superficial necrosis of the superficial flap, all with favorable evolution. Only one patient underwent implant extrusion.
CONCLUSION: Breast reconstruction using excess flaps in reverse mini abdominoplasty associated with implant placement is a good option for breast reconstruction in selected patients with a low complication rate. Patients with flaccidity and lipodystrophy in the upper abdomen are the ideal candidates for the use of this technique.
Keywords: Reconstructive surgical procedures; Abdominoplasty; Breast; Mammaplasty.
RESUMO
INTRODUÇÃO: A mastectomia é muito traumática para a mulher, sendo a reconstrução mamária um procedimento essencial para melhorar o bem-estar psicossocial e a qualidade de vida destas pacientes. A maioria dos cirurgiões plásticos não realiza reconstrução mamária. Sua prática requer um treinamento avançado com longa curva de aprendizado. A reconstrução mamária, utilizando o retalho excedente da abdominoplastia reversa, pode ser uma opção prática e de muita aplicabilidade em pacientes cuidadosamente selecionadas.
MÉTODOS: No período de agosto de 2014 a junho de 2016, doze pacientes foram submetidas à reconstrução mamária, com a técnica de miniabdominoplastia reversa. A simetrização foi realizada em seis pacientes que fizeram reconstrução unilateral, sendo um caso reconstruído bilateralmente. Em sete pacientes, os implantes foram colocados em plano supra muscular, e em cinco, em posição sub submuscular.
RESULTADOS: Uma paciente apresentou seroma, uma outra teve epiteliólise, um caso de necrose parcial da pele do retalho superficial, todos com evolução favorável. Somente uma paciente teve extrusão do implante.
CONCLUSÃO: A reconstrução mamária com retalho excedente de miniabdominoplastia reversa associada à colocação de implante demonstrou ser uma boa opção de reconstrução mamária para casos selecionados, com baixa taxa de complicações. Pacientes com flacidez e lipodistrofia no abdome superior são as candidatas ideais para utilização da técnica.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Abdominoplastia; Mama; Mamoplastia.
Mastectomy is a highly traumatic procedure for women. Breast reconstruction is a priority in the treatment among women, which could improve their well-being and quality of life1. There are many techniques that can be used with and without implants. The ultimate goal is the best option for each case2.
The earliest reports of breast reconstruction date from the late 19th century3-6.
The use of breast reconstruction for post-mastectomy patients was delayed for a long period. Halstead (1989) believed that the reconstruction interfered in the local control of cancers1.
Louis Ombredanne (1906)1 was the first to describe pectoral muscle flaps for immediate reconstruction of the breast, along with thoracoabdominal skin flaps for patients who had been submitted to radical mastectomy due to cancer.
Distant skin flaps (tubular), which were used initially, were abandoned owing to the necessity of several surgical periods, high rates of complications, and scarring sequelae4.
Breast implants have changed the outcomes of breast reconstruction, since they are widely used and are the basis of late treatment7,8. As a consequence, Radovan used tissue expanders in breast reconstruction in 19829, and Becker (1984)10 developed definitive expanders.
The latissimus dorsi muscle flap, first published in 1939 by Hutchins, is one of the best methods currently used and has been popularized by Olivari (1974)11,12; this should be associated with the implant owing to insufficient tissue volumes, as described by Schneider (1977)13. It is currently one of the most versatile and reliable flaps available for use in reconstructive surgery. It also recommends that total breast reconstructions should be performed in a single surgical period, including restoration of the nipple-areolar complex and contralateral symmetrization13.
Robbins first described transverse rectus abdominis myocutaneous (TRAM) flaps in 1979, which were modified by Hartrampf et al.14 and Gandolfo14 in 1982. Together with latissimus dorsi flaps, these are employed frequently in breast reconstruction. The advantage includes providing enough tissue to cover large defects. The disadvantages are generated owing to the weakness in the abdominal wall and the risk of producing hernias15.
The development of free microvascular flaps described by Holmstrom (1979)15 showed abundant materials for reconstruction; the use of these flaps involves the same area of TRAM flaps, is based on the abdominal perforators and branches of the inferior epigastric muscles, and can involve the rectus abdominis muscles16-18. In 1989, Grotting et al.19 published a study that demonstrated the advantages of this technique, such as improved blood supply, reduced risk of necrosis, and improved functional loss of the abdominal wall.
Other therapeutic possibilities are available, such as the use of inferior epigastric perforator flaps (DIEP and SIEA)20-23, free gluteal artery perforator flaps (SGAP and IGAP)24,25, dermofat flaps26-31, and local fasciocutaneous flaps.
Very large reconstructions can present unsatisfactory aesthetic results, as reported by some authors32.
Currently, there is a tendency of using more conservative mastectomy techniques, facilitating the reconstruction with more favorable aesthetic results4.
Although these have been used for many surgical opportunities33,34, reverse abdominoplasty flaps35 have not been presented as additional tissue thickness of subcutaneous tissue for breast reconstruction, with the purpose of protection of silicone prostheses. In 1992, Berrino et al.36 compared different reconstructive techniques for type II deformities, one of them being a flap obtained from reverse abdominoplasty, but without presenting major findings or going into details over the technique.
In 2009, Deos et al.37 reinvestigated reverse abdominoplasty35 and implemented new concepts, correcting the disadvantages of the original technique, with strategic planning from the marking, fixing of the flap, and maintenance of a stable scar; they consequently called it "tensioned reverse abdominoplasty."
The excess flap from reverse abdominoplasty38 can be a practical option and highly applicable in breast reconstruction in carefully selected patients.
OBJECTIVE
The objective of this study is to present the author's experience in the reconstruction of the breasts, unilaterally and bilaterally, using the reverse mini abdominoplasty technique.
METHODS
From August 2014 to June 2016, 12 patients underwent breast reconstruction using the reverse mini abdominoplasty technique. The age ranged between 41 and 63 years, with a mean of 52.8 years. The surgeries were performed in the clinic of the author and the Hospital Guilherme Álvaro located in the city Santos, state of São Paulo.
The inclusion criteria were as follows: late reconstruction, unilateral or bilateral mastectomy, abdominal flaccidity, and lipodystrophy in the upper abdomen.
Symmetrization was performed in six patients who had unilateral reconstruction, with bilateral reconstruction in one patient.
The study followed the Declaration of Helsinki principles and used an Informed Consent Form.
Surgical technique
The demarcation of the reverse abdominoplasty was performed, starting in the contralateral breast and following the line of the mastectomized breast scar (Figure 1). In cases of bilateral reconstruction, the incision line bilaterally followed the scars of the mastectomies (Figure 2). In both situations, the incision lines were in the midline at the height of the xiphoid appendix. After the incision and reverse detachment of the supraumbilical abdomen, the flap was incised in the midline, biparting it into two lower base triangular flaps (Figures 3 and 4).
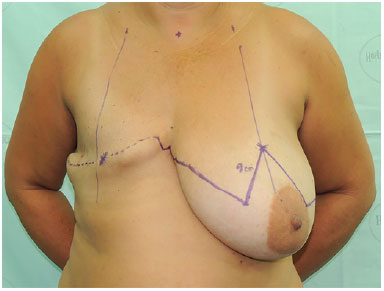
Figure 1. Marking - starts in the contralateral breast, following the line of the scar of the mastectomized breast.
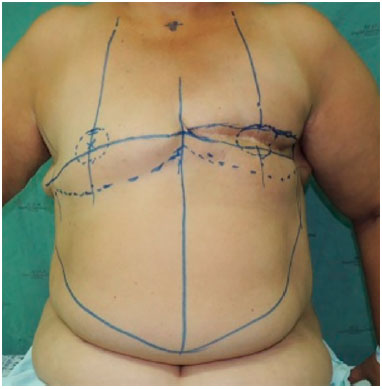
Figure 2. The incision line follows the scars of mastectomies D and E bilaterally.
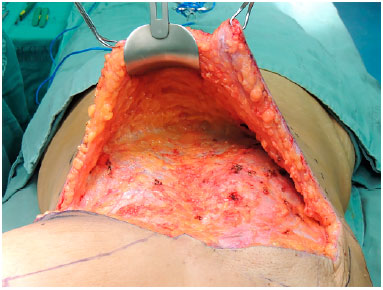
Figure 3. Reverse detachment of the supraumbilical abdomen.
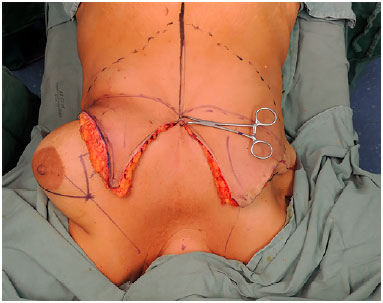
Figure 4. The flap is incised in the midline, biparting it into two lower base triangular flaps.
Next, the abdominal flap was fixed using adhesion sutures, followed by five traction lines, attaching it to the muscular fascia to avoid sliding downwards (Figure 5). The triangular flap was tractioned in the cephalic direction and the medial portion attached to the edge of the upper incision of the xiphoid appendix. The superior detachment was performed in the supra- or inframuscular plane, depending on the need and existence of the pectoralis major.
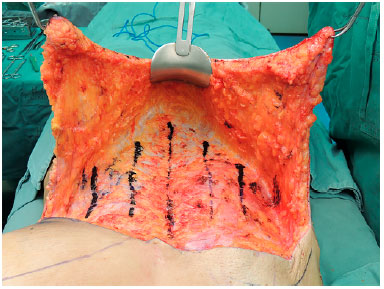
Figure 5. The abdominal flap is fixed with adhesion sutures, following five traction lines, attaching it to the muscular fascia.
When needed, the upper portion of the flap was decorticated and invaginated under the skin of the upper pole to provide better coverage (cushion) to the associated implant (Figures 6 and 7). The lower portion of the flap served to rebuild the lower pole. In unilateral cases, the contralateral flap was discarded, and the border was accommodated to the mammary sulcus. In cases of bilateral reconstruction, both flaps were used for reconstruction.

Figure 6. When necessary, the upper portion of the flap is decorticated, while invaginating it under the skin of the upper pole.

Figure 7. When necessary, the upper portion of the flap is decorticated and invaginated under the skin of the upper pole.
The breast implant was placed supra- or infra-muscularly, depending on the need for greater protection and presence after the mastectomy.
The new groove was formed using fixation sutures to the ribs, usually to the fifth and sixth ribs (Figure 8).

Figure 8. Fixing the flap to the rib for formation of the mammary groove.
Continuous aspiration drains were used and removed on the fourth to fifth postoperative days.
Suturing was performed using monocryl sutures (4-0) in the subcutaneous tissue and subdermis (Figure 9). When used, the "interrupted" sutures were removed on the seventh postoperative day.

Figure 9. Suture and immediate final result.
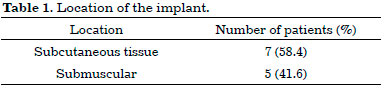
The implants were placed in the subcutaneous plane and in a submuscular position in seven and five patients, respectively (Table 1).
Seven right breasts were constructed, four left breasts and one case of bilateral reconstruction (Table 2).
RESULTS
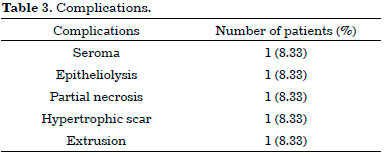
One patient presented seroma on the 10th postoperative day, requiring three sessions of aspiration, removing 40, 30, and 10 mL, and showing good evolution.
One bilateral reconstruction patient presented extrusion of the implant on the left breast on the 45th postoperative day (in the area corresponding to the post-mastectomy radiotherapy), requiring removal of the implant. The right breast implant was also removed for suspected contamination owing to the contiguity of the surgical pockets.
One patient had epitheliolysis, with debridement and good evolution, without the need to remove the implant.
One case of partial necrosis occurred on the contralateral areola, which progressed satisfactorily after debridement.
One patient presented hypertrophic scar, requiring revision of the scar after 8 months.
Table 3 shows the complications.
Some pre- and postoperative images are shown in Figures 10 A-B; 11 A-B; 12 A-B, and 13 A-B).
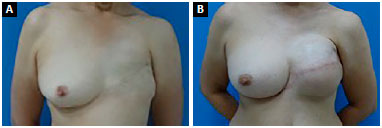
Figure 10. A: Pre- and postoperative - Frontal view; B: Pre- and postoperative - Frontal view.
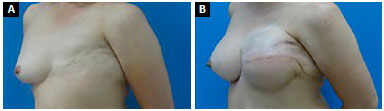
Figure 11. A: Pre- and postoperative - Oblique view; B: Pre- and postoperative - Oblique view.
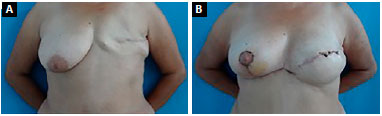
Figure 12. A: Pre- and postoperative - Frontal view; B: Pre- and postoperative - Frontal view.
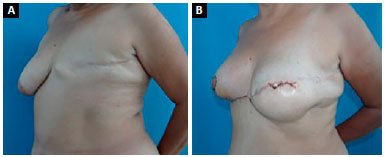
Figure 13. A: Pre- and postoperative - Oblique view; B: Pre- and postoperative - Oblique view.
DISCUSSION
Mastectomy is highly traumatic for women, and breast reconstruction is an essential procedure to improve their psychosocial well-being and quality of life1.
Conservative techniques associated with breast prostheses9,10 have changed the evolution of breast reconstruction and introduced modern techniques. The diversity of breast reconstruction techniques allows for an adequate selection for each specific case, offering better results.
The majority of breast reconstruction procedures offer sufficient coverage and volume1,6,9,14; however, breast prostheses are essential for the complementation of breast volume and shape, offering better results6,10.
Several procedures use local flaps of the upper abdominal region for breast reconstruction29,36.
Most plastic surgeons do not perform breast reconstruction. This practice requires an advanced training with a long learning curve. The techniques are very elaborate, and specialized training is mandatory. The ideal planning of mastectomized breast reconstruction requires planning that involves the time prior to mastectomy, during the preoperative step with the mastologist.
The development of less invasive and easily reproducible techniques is a fundamental step in addressing the demand and defense of the specialty.
A large number of patients present with flaccidity and lipodystrophy in the upper abdomen; thus, the technique of using excess flaps in reverse mini abdominoplasty38, with a short learning curve, may be another option for either single or bilateral breast reconstruction. The reconstruction with this procedure promotes an important aesthetic result in the upper abdomen, reflecting on the patients' psychological comfort, which already presents an impairment in quality of life.
This procedure prevents scars outside the area to be reconstructed, can be performed in bilateral reconstructions, and presents satisfactory aesthetic results, besides the benefit of supraumbilical abdominoplasty.
This technique has a reduced surgical period, good vascular support of the flap, and low rate of complications. In this study, there was one case each of seroma, epitheliolysis, and superficial necrosis; only one patient who underwent bilateral reconstruction required removal of implants.
This study needs continuity with a multicenter study for better observations and greater precision in the indications of the technique.
CONCLUSION
Breast reconstruction using excess flaps in reverse mini abdominoplasty associated with the placement of implants is a good option for breast reconstruction for selected cases, with a low rate of complications.
Patients with flaccidity and lipodystrophy in the upper abdomen are the ideal candidates for this technique.
COLLABORATIONS
ORSF Analysis and/or interpretation of data; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
OS Final approval of the manuscript; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
EC Statistical analyses; final approval of the manuscript; critical review of its contents.
MRM Final approval of the manuscript; critical review of its contents; completion of surgeries and/or experiments.
DC Final approval of the manuscript; critical review of its contents; completion of surgeries and/or experiments.
ACC Completion of surgeries and/or experiments.
FFG Completion of surgeries and/or experiments.
LG Completion of surgeries and/or experiments.
REFERENCES
1. Wilkins EG, Cederna PS, Lowery JC, Davis JA, Kim HM, Roth RS, et al. Prospective analysis of psychosocial outcomes in breast reconstruction: one-year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2000;106(5):1014-25. DOI: http://dx.doi.org/10.1097/00006534-200010000-00010
2. Munhoz AM, Montag E, Arruda E, Pellarin L, Filassi JR, Piato JR, et al. Assessment of immediate conservative breast surgery reconstruction: a classification system of defects revisited and an algorithm for selecting the appropriate technique. Plast Reconstr Surg. 2008;121(3):716-27. PMID: 18317121 DOI: http://dx.doi.org/10.1097/01.prs.0000299295.74100.fa
3. Wickman M. Breast reconstruction--past achievements, current status and future goals. Scand J Plast Reconstr Surg Hand Surg. 1995;29(2):81-100. DOI: http://dx.doi.org/10.3109/02844319509034325
4. Goldwyn RM. Vincenz Czerny and the beginnings of breast reconstruction. Plast Reconstr Surg. 1978;61(5):673-81. PMID: 347474 DOI: http://dx.doi.org/10.1097/00006534-197805000-00003
5. Teimourian B, Adham MN. Louis Ombredanne and the origin of muscle flap use for immediate breast mound reconstruction. Plast Reconstr Surg. 1983;72(6):905-10. PMID: 6359197 DOI: http://dx.doi.org/10.1097/00006534-198312000-00037
6. Maxwell GP. Iginio Tansini and the origin of the latissimus dorsi musculocutaneous flap. Plast Reconstr Surg. 1980;65(5):686-92. DOI: http://dx.doi.org/10.1097/00006534-198005000-00027
7. Cronin TD, Gerow F. Augmentation mammaplasty: a new "natural feel" prosthesis. In: Broadbent TR, ed. Transactions of the third international Congress of Plastic surgery. Amsterdam: Excerpta Medica; 1964. p. 41-9.
8. Jarrett JR, Cutler RG, Teal DF. Subcutaneous mastectomy in small, large, or ptotic breasts with immediate submuscular placement of implants. Plast Reconstr Surg. 1978;62(5):702-5. PMID: 715020 DOI: http://dx.doi.org/10.1097/00006534-197811000-00006
9. Radovan C. Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg. 1982;69(2):195-208. PMID: 7054790 DOI: http://dx.doi.org/10.1097/00006534-198202000-00001
10. Becker H. Breast reconstruction using an inflatable breast implant with detachable reservoir. Plast Reconstr Surg. 1984;73(4):678-83. PMID: 6709750 DOI: http://dx.doi.org/10.1097/00006534-198404000-00031
11. Brantigan OC. Evaluation of Hutchins' modification of radical mastectomy for cancer of the breast. Am Surg. 1974;40(2):86-8. PMID: 4810635
12. Olivari N. The latissimus flap. Br J Plast Surg. 1976;29(2):126-8. PMID: 776304 DOI: http://dx.doi.org/10.1016/0007-1226(76)90036-9
13. Schneider WJ, Hill HL Jr, Brown RG. Latissimus dorsi myocutaneous flap for breast reconstruction. Br J Plast Surg. 1977;30(4):277-81. DOI: http://dx.doi.org/10.1016/0007-1226(77)90117-5
14. Hartrampf CR, Scheflan M, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg. 1982;69:216-25. PMID: 6459602 DOI: http://dx.doi.org/10.1097/00006534-198202000-00006
15. Holmström H. The free abdominoplasty flap and its use in breast reconstruction. An experimental study and clinical case report. Scand J Plast Reconstr Surg. 1979;13(3):423-7.
16. Futter CM, Webster MH, Hagen S, Mitchell SL. A retrospective comparison of abdominal muscle strength following breast reconstruction with a free TRAM or DIEP flap. Br J Plast Surg. 2000;53(7):578-83. PMID: 11000074 DOI: http://dx.doi.org/10.1054/bjps.2000.3427
17. Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987;40(2):113-41. PMID: 3567445 DOI: http://dx.doi.org/10.1016/0007-1226(87)90185-8
18. Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994;32(1):32-8. PMID: 8141534 DOI: http://dx.doi.org/10.1097/00000637-199401000-00007
19. Grotting JC, Urist MM, Maddox WA, Vasconez LO. Conventional TRAM flap versus free microsurgical TRAM flap for immediate breast reconstruction. Plast Reconstr Surg. 1989;83(5):828-41. DOI: http://dx.doi.org/10.1097/00006534-198905000-00009
20. Cunha MS, Munhoz AM, Sturtz G, Montag E, Ferreira MC. Avaliação da Perfusão do Retalho de Perfurante da Artéria Epigástrica Inferior Microcirúrgico Aplicado em Reconstrução Mamária. Rev Bras Cir Plást. 2006;21(4):191-5.
21. Munhoz AM, Arruda E, Montag E, Aldrighi C, Aldrighi JM, Gemperli R, et al. Immediate skin-sparing mastectomy reconstruction with deep inferior epigastric perforator (DIEP) flap. Technical aspects and outcome. Breast J. 2007;13(5):470-8. DOI: http://dx.doi.org/10.1111/j.1524-4741.2007.00467.x
22. Arnez ZM, Khan U, Pogorelec D, Planinsek F. Breast reconstruction using the free superficial inferior epigastric artery (SIEA) flap. Br J Plast Surg. 1999;52(4):276-9. DOI: http://dx.doi.org/10.1054/bjps.1999.3100
23. Chevray PM. Breast reconstruction with superficial inferior epigastric artery flaps: a prospective comparison with TRAM and DIEP flaps. Plast Reconstr Surg. 2004;114(5):1077-83. DOI: http://dx.doi.org/10.1097/01.PRS.0000135328.88101.53
24. Allen RJ, Levine JL, Granzow JW. The in-the-crease inferior gluteal artery perforator flap for breast reconstruction. Plast Reconstr Surg. 2006;118(2):333-9. PMID: 16874198 DOI: http://dx.doi.org/10.1097/01.prs.0000227665.56703.a8
25. Granzow JW, Levine JL, Chiu ES, Allen RJ. Breast reconstruction with gluteal artery perforator flaps. J Plast Reconstr Aesthet Surg. 2006;59(6):614-21. PMID: 16716955 DOI: http://dx.doi.org/10.1016/j.bjps.2006.01.005
26. Mendes F, Figueiredo JC, Pereira WB, Mélega JM. Reconstrução mamária: uma revisão e classificação de técnicas. In: Tournieux AA, Curi MM, ed. Atualização em cirurgia plástica - SBCP. São Paulo: Robe Editorial; 1996. p. 341-51.
27. Longracre JT. The use of local pedicle flaps for reconstruction of the breast after subtotal or total extirpation of the mammary gland and for the correction of distortion and atrophy of the breast due to excessive scar. Plast Reconstr Surg (1946). 1953;11(5):380-403. DOI: http://dx.doi.org/10.1097/00006534-195305000-00008
28. Baroudi R, Pinotti JA, Keppke EM. A transverse thoracoabdominal skin flap for closure after radical mastectomy. Plast Reconstr Surg. 1978;61(4):547-54. PMID: 345306 DOI: http://dx.doi.org/10.1097/00006534-197804000-00008
29. Pinto EBS, Muniz AC, I PE, Cação EG, Abdalla PCSP. Reconstrução Mamária: Princípios Geométricos dos Retalhos Cutâneos em Duplo V. Rev Bras Cir Plást. 1998;13(3):19-42.
30. Holmström H, Lossing C. The lateral thoracodorsal flap in breast reconstruction. Plast Reconstr Surg. 1986;77(6):933-43. PMID: 3714889 DOI: http://dx.doi.org/10.1097/00006534-198606000-00010
31. Pitanguy I, Caldeira AM, Alexandrino A, Trevino MN, Calixio CA. Retalho braquial fasciocutâneo - técnica de Pitanguy para deformidade infraclavicular pós-mastectomia. Rev Bras Cir. 1984;74(6):349-60.
32. Cosac OM, Camara Filho JPP, Cammarota MC, Lamartine JD, Daher JC, Borgatto MS, et al. Reconstrução mamária de resgate: a importância dos retalhos miocutâneos. Rev Bras Cir Plást 2013;28(1):92-9. DOI: http://dx.doi.org/10.1590/S1983-51752013000100016
33. Zienowicz RJ, Karacaoglu E. Augmentation mammaplasty by reverse abdominoplasty (AMBRA). Plast Reconstr Surg. 2009;124(5):1662-72. PMID: 20009853 DOI: http://dx.doi.org/10.1097/pRS.0b013e3181babd02
34. Baroudi R, Keppke EM, Carvalho CG. Mammary reduction combined with reverse abdominoplasty. Ann Plast Surg. 1979;2(5):368-73. DOI: http://dx.doi.org/10.1097/00000637-197905000-00002
35. Rebello C, Franco T. Abdominoplastia pela incisão sub-mamária. Rev Bras Cir. 1972;7:249-52.
36. Berrino P, Campora E, Leone S, Santi P. Correction of type II breast deformities following conservative cancer surgery. Plast Reconstr Surg. 1992;90(5):846-53. PMID: 1410038 DOI: http://dx.doi.org/10.1097/00006534-199211000-00019
37. Deos MF, Arnt RA, Gus EI. Tensioned reverse abdominoplasty. Plast Reconstr Surg. 2009;124(6):2134-41. PMID: 19952671 DOI: http://dx.doi.org/10.1097/pRS.0b013e3181bf8353
38. Saldanha OR, Urdaneta FV, Llaverias F, Saldanha Filho OR, Saldanha CB. Reconstrução de mama com retalho excedente de abdominoplastia reversa. Rev Bras Cir Plást. 2014;29(2):297-302.
1. Clinica Saldanha, Santos, SP, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
3. Hospital São Lucas, Serviço de Cirurgia Plástica Osvaldo Saldanha, Santos, SP, Brazil
Institution: Hospital São Lucas, Serviço de Cirurgia Plástica Osvaldo Saldanha, Santos, SP, Brazil.
Corresponding author:
Osvaldo Ribeiro Saldanha Filho
Avenida Washington Luiz, 142 - Encruzilhada
Santos, SP, Brazil - Zip Code 11050-200
E-mail: drosvaldo@saldanhafilho.com.br
Article received: July 15, 2016.
Article accepted: September 19, 2016.
Conflicts of interest: none.



 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter