

Original Article - Year 2017 - Volume 32 -
Epidemiological profile of patients with orofacial cleft treated by a reference surgical team in the State of Amazonas, Brazil
Perfil epidemiológico dos pacientes portadores de fissuras labiopalatinas atendidos por equipe cirúrgica de referência no Estado do Amazonas
ABSTRACT
INTRODUCTION: Orofacial clefts are congenital malformations with an estimated occurrence of 1:650 births in Brazil. The most widely adopted classification system in that country is the method developed by Spina, and cheiloplasty and palatoplasty are the main surgeries performed.
METHODS: This was a retrospective descriptive study using data collected from the Smile Train Express organization regarding patients with orofacial clefts treated by a reference surgical team between March 1, 2014 and December 1, 2016.
RESULTS: A total of 477 patients were identified, predominantly male and in the first two years of life at admission. The most prevalent type of malformation was left unilateral transforamen cleft. The most frequent surgical treatment was cheiloplasty.
CONCLUSIONS: The epidemiological pattern is consistent with the findings described in the national literature.
Keywords: Orofacial cleft; Cleft lip; Maxillofacial abnormalities; Epidemiology; Classification.
RESUMO
INTRODUÇÃO: As fissuras labiopalatinas são malformações congênitas e, no Brasil, estima-se a ocorrência de 1:650 nascimentos. A classificação adotada é a de Spina. A queiloplastia e a palatoplastia são as principais cirurgias executadas.
MÉTODOS: Estudo retrospectivo descritivo com obtenção de dados a partir do sistema Smile Train Express referente a pacientes com fissura labiopalatina atendidos por equipe cirúrgica de referência entre 1 de março de 2014 e 1 de dezembro de 2016.
RESULTADOS: Foram identificados 477 pacientes, predominando o sexo masculino e os dois primeiros anos de vida na admissão. A fissura mais prevalente foi transforame e unilateral esquerda. O tratamento cirúrgico mais frequente foi a queiloplastia.
CONCLUSÕES: O padrão epidemiológico está em consonância com a literatura nacional.
Palavras-chave: Fissura palatina; Fenda labial; Anormalidades maxilofaciais; Epidemiologia; Classificação.
Orofacial clefts (OFCs) are congenital malformations that occur between the 4th and 12th weeks of the embryonic period owing to lack of fusion of the maxillary and mid-nasal processes1. These malformations are attributed to genetic and environmental factors, which can act alone or in combination. More than half of individuals with a cleft have relatives who also have the malformation. The most frequently associated environmental factors are: maternal stress; medication use; ionizing radiation; nutritional, toxic, and infectious agents; and smoking during fetal development2.
OFCs are the most frequent facial malformations, with an estimated occurrence on the order of 1 in 650 births in Brazil2,3. Most individuals with OFC do not present with any other abnormalities (non-syndromic OFC), but a significant proportion (30 to 50%) manifest other malformations and may exhibit a particular syndrome (syndromic OFC)4.
Several proposed classifications have been developed that are based on morphological and/or embryonic aspects. The most widely used in Brazil is the Spina Classification, divided into four groups: incisional pre-foramen cleft or, simply, cleft lip (CL), incisional post-foramen cleft or palatine fissures (PF), transforamen cleft or orofacial cleft (OFC), and rare clefts of the face (Figure 1).

Figure 1. Classification of the types of orofacial cleft, according to Spina.
The Spina Classification is based on the embryological theory that recognizes the independent developmental mechanisms of the anterior structures (originating from the primary palate) and those posterior to the incisive foramen (originating from the secondary palate), with this anatomical reference point chosen for this particular classification. The current limited knowledge in the field regarding the etiology of OFC hinders even the descriptions and distinctions of the various forms of presentation of these malformations5.
OFCs have a significant impact on speech, hearing, and appearance, as well as a major influence on the health and social integration of a patient, owing not only to morbidity, but mainly to emotional disturbances, stigmatization, and social exclusion, as these malformations interfere with the development of self-esteem, interpersonal relations, and incorporation into the socioeconomic and cultural environment6.
It is important for the individual with a cleft to undergo early follow-up, performed by a multiprofessional team, with an interdisciplinary approach, as well as integral treatment, continuing from birth to adulthood, providing the individual with the necessary tools for adjustment to society.
Cheiloplasty and palatoplasty are the initial reparative plastic surgeries performed during the long and complex treatment of OFC. For the child who is born with an OFC, reconstructive surgery is a challenge not only aesthetically, but mainly functionally. Cheiloplasty consists of reconstructive surgery of the cleft lip, and palatoplasty is the reconstruction of the cleft palate7.
The treatment protocol most often used, including by the team currently working in Manaus, is closure of the lip at 3 months of age, and closure of the palate, in a single procedure, at 1 year of age. Alveolar bone graft is performed in patients between 7 years and 9 years of age, when the canine teeth are close to eruption. Orthognathic surgery is performed in patients older than 15 years of age. The final surgery of the patient with a cleft is a secondary rhinoplasty, to correct any residual nasal deformity8.
In 2014, the State Health Secretariat of Amazonas (SUSAM) signed an agreement with Smile Train Express9, an international non-governmental organization, founded in 1999, which aims to provide comprehensive treatment to patients with OFCs around the world. With this partnership, the surgical team became a reference for patients diagnosed with OFCs in the State of Amazonas. Surgeries for OFC are performed in the Dr. Fajardo Children's Hospital; in addition, there are corrective surgeries to treat this malformation performed as part of a yearly communal work effort in the city of Manaus.
OBJECTIVE
The purpose of this study was to present the main epidemiological features of OFC in the population of patients treated by a reference surgical team for OFC in the State of Amazonas.
METHODS
This was a retrospective descriptive study performed at the Dr. Fajardo Children's Hospital, in Manaus, AM, with data acquired from the Smile Train Express9 organization regarding patients with a diagnosed OFC treated and operated on by a reference surgical team in Amazonas between March 1, 2014 and December 1, 2016. The Research Ethics Committee of the Adriano Jorge Hospital Foundation approved this research under opinion number 1,899,716/2017.
Data from a total of 477 patients were collected, with the following analysis variables: cleft types according to the Spina Classification5, sex, origin, age, and surgical condition at hospital admission, as well as the surgical treatment performed. Regarding surgical condition at admission, any history of previous surgical treatment was analyzed and, in case of previous surgery, an attempt was made to identify the type of surgery performed.
RESULTS
During the study period, 477 patients with OFC who underwent surgery performed by the reference surgical team were identified. There was a slight male predominance of 52%.
Table 1 shows the distribution of these patients regarding age at admission to the service. The minimum age was 17 days and the maximum age was 47 years.
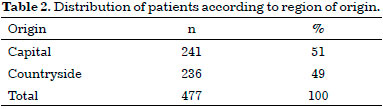
Almost half of the patients studied came from the interior of Amazonas, as shown in Table 2.
Regarding the type of cleft, the most prevalent was incisive transforamen (60%), followed by incisive pre-foramen fissure (24%), and, finally, incisive foramen cleft (15%). There were five cases in which patients had pre- and post-foramen (1%) fissures, concomitantly. There was a predominance of left side clefts. Table 3 shows that the types of OFC were regrouped into: pre-foramen cleft (complete and incomplete/right, left, and bilateral), 113 cases; post-foramen cleft (complete and incomplete), 68 cases; pre- and post-foramen cleft (right and left), 5 cases; and transforamen cleft (right, left, and bilateral), 291 cases. All transforamen clefts affect the incisive foramen and all pre- and post-foramen clefts do not.
As shown in Figure 2, half of the patients with a cleft had undergone previous surgery, with cheiloplasty (65%) the most frequent, followed by cheiloplasty and palatoplasty (25%) and, finally, palatoplasty (10%).
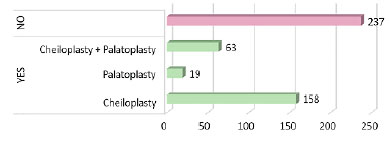
Figure 2. Distribution of clefts according to surgical condition at admission to the referral service in the State of Amazonas.
The surgical treatments performed in these patients are detailed in Figure 3, with cheiloplasty being the most frequent (35%), followed by palatoplasty (27.5%). Procedures for correction of previous surgeries (secondary surgeries) were also performed, and 11.5% of patients underwent simultaneous surgeries ("combo").
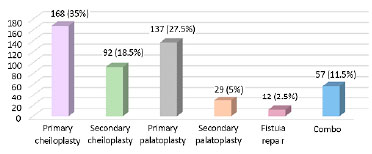
Figure 3. Distribution of surgeries performed in patients with orofacial cleft.
DISCUSSION
During the study period, 477 patients were attended to by a reference surgical team in the State, and a total of 495 procedures were performed.
The present study shows that, among the analyzed patients, OFCs were more frequent among the male sex (52%); and although the difference was not significant, this finding is consistent with most national statistics10-14.
The most frequent age at admission of patients in the referral service was between one month and two years (35%), which was considered adequate; this time frame is compatible with the chronology of primary lip and palate surgeries and allows early treatment, especially in cases of bilateral transforamen cleft, since the structures involved and the extent of the lesion result in greater complexity, requiring a longer duration of treatment15.
Another study finding was that an approximately equal number of individuals with OFC came from the countryside and the capital of the State of Amazonas. It is necessary to take into account that at various times, communal chirurgical efforts were undertaken in some municipalities, such as Tefé, Parintins, Itacoatiara, Tabatinga, Eirunepé, and Benjamin Constant, and that most municipalities have geographical peculiarities that result in difficulties in access to specialized services for the population. Therefore, it is not possible to state that the numbers obtained in this study represent the reality for the entire state.
In most published national studies12-16, the percentage of individuals with transforamen cleft has been higher when compared to cleft lip or cleft palate alone, as in our case series (60% vs. 24% pre-foramen vs. 15% post-foramen). Spina's rank5 allows the identification of mixed forms (pre-foramen and post-foramen clefts in the same carrier), which occur during different periods of embryological development. We found this type of fissure in 1% of cases in our study.
In the present study, the OFCs were unilateral in most cases, with the left side more commonly affected, as described in the national literature11,13,14. The reason for this predilection is not understood. Patterns of laterality defects are known to be observed in various types of anomalies. Groups of genes expressed asymmetrically during the early stages of embryonic development may contribute to this preference, but this hypothesis has not yet been demonstrated by any study17.
According to the anatomical extension, clefts can be subclassified as complete or incomplete, with the rupture or non-rupture of the incisive foramen as a reference. Such subclassification is only used for pre- or post-foramen clefts5. This understanding is necessary for the elaboration of a therapeutic plan, because the greater the extent of the fissure, the greater the functional impairment and, therefore, the greater the resources required for the total recovery of the patient.
In the present study, incomplete clefts (80%) predominated, among those classified as pre- or post-foramen, as in the findings of Gardenal et al.13. On the other hand, if we add the transforamen clefts to the set, we can observe a predominance of complete fissures (70%), since all the transforamen clefts affect the incisive foramen.
Cheiloplasty and palatoplasty are the first restorative surgeries performed during the long process of treatment of OFCs. In the studies of Alonso et al.10, Gardenal et al.13, and Moura18, the majority of patients with OFCs had not undergone a previous surgical procedure to correct this malformation at the time of admission to the service (70%, 80%, and 90%, respectively).
In our study, we did not obtain the same results, since 49.5% of the patients had already undergone some type of primary corrective surgery. According to Gardenal et al.13, this condition is considered unfavorable since multidisciplinary care is usually not delivered after the surgical steps, particularly following cheiloplasty.
Finally, the main surgical modalities (cheiloplasty and palatoplasty) for the treatment of OFC were subdivided into primary and secondary. We observed that, in both cases, cheiloplasty was the procedure with the highest prevalence.
CONCLUSION
Based on the results of this study, we infer that OFCs are more frequent in the male sex, with a predominance in the first two years of life at the time of admission to the surgical service and an equal distribution in origin in these patients. Transforamen and left unilateral cleft were the most prevalent types. Among those classified as pre- or post-foramen, incomplete clefts predominated. Half of the study patients had undergone previous surgery, and cheiloplasty was the most commonly performed surgery, both as a primary and secondary procedure.
COLLABORATIONS
KMGA Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
AJAS Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript.
REFERENCES
1. Moore KL, Persaud TVN. Embriologia clínica. 5a ed. Rio de Janeiro: Guanabara Koogan; 1995. 360 p.
2. Modolin MLA, Cerqueira EMM. Etiopatogenia. In: Altmann EBC, org. Fissuras Labio-palatinas. 4a ed. Carapicuíba: Pró-Fono; 1997. p. 25-30.
3. Capelozza Filho L, Silva Filho OG. Fissuras Lábio-palatais. In: Petrelli E, org. Ortodontia para Fonoaudiologia. Curitiba: Lovise; 1992. p. 195-239.
4. Stoll C, Alembik Y, Dott B, Roth MP. Associated malformations in cases with oral clefts. Cleft Palate Craniofac J. 2000;37(1):41-7. PMID: 10670888 DOI: http://dx.doi.org/10.1597/1545-1569(2000)037<0041:AMICWO>2.3.CO;2
5. Spina V, Psillakis JM, Lapa FS, Ferreira MC. Classificação das fissuras lábio-palatais: sugestão de modificação. Rev Hosp Clin Fac Med São Paulo. 1972;27(1):5-6.
6. Amaral VLAR. Aspectos psicológicos, problemas sociais e familiares associados às fissuras lábio-palatinas. In: Carreirão S, Lessa S, Zanini AS, eds. Tratamento das fissuras labiopalatinas. Rio de Janeiro: Revinter; 1996. p. 19-23.
7. Biazon J, Peniche ACG. Retrospective study of postoperative complications in primary lip and palate surgery. Rev Esc Enferm USP. 2008;42(3):519-25. DOI: http://dx.doi.org/10.1590/S0080-62342008000300015
8. Alonso N, Tanikawa DYS, Lima Junior JE, Rocha DL, Sterman S, Ferreira MC. Fissuras labiopalatinas: protocolo de atendimento multidisciplinar e seguimento longitudinal em 91 pacientes consecutivos. Rev Bras Cir Plást. 2009;24(2):176-81.
9. Smile Train Express Database. [acesso 2016 Dez 5]. Disponível em: https://smiletrainexpress.org
10. Alonso N, Tanikawa DYS, Lima Junior JE, Ferreira MC. Avaliação comparativa e evolutiva dos protocolos de atendimento dos pacientes fissurados. Rev Bras Cir Plást. 2010;25(3):434-8. DOI: http://dx.doi.org/10.1590/S1983-51752010000300006
11. Souza J, Raskin S. Clinical and epidemiological study of orofacial clefts. J Pediatr (Rio J). 2013;89(2):137-44. DOI: http://dx.doi.org/10.1016/j.jped.2013.03.010
12. Martelli DR, Machado RA, Swerts MS, Rodrigues LA, Aquino SN, Martelli Júnior H. Non syndromic cleft lip and palate: relationship between sex and clinical extension. Braz J Otorhinolaryngol. 2012;78(5):116-20. PMID: 23108830
13. Gardenal M, Bastos PRH, Pontes ERJC, Bogo D. Prevalência das fissuras orofaciais diagnosticadas em um serviço de referência em casos residentes no estado de Mato Grosso do Sul. Arq Int Otorrinolaringol. 2011;15(2):133-41. DOI: http://dx.doi.org/10.1590/S1809-48722011000200003
14. Cymrot M, Sales FCD, Teixeira FAA, Teixeira Junior FAA, Teixeira GSB, Cunha Filho JF. Prevalência dos tipos de fissura em pacientes com fissuras labiopalatinas atendidos em um Hospital Pediátrico do Nordeste brasileiro. Rev Bras Cir Plást. 2010;25(4):648-51. DOI: http://dx.doi.org/10.1590/S1983-51752010000400015
15. Silva Filho OG, Freitas JA, Okada T. Fissuras lábio- palatais: diagnóstico e uma filosofia interdisciplinar de tratamento. In: Pinto VG, ed. Saúde bucal coletiva. São Paulo: Santos. 4a ed. São Paulo: Santos; 2000. p. 480-527.
16. Freitas JA, Dalben Gda S, Santamaria M Jr, Freitas PZ. Current data on the characterization of oral clefts in Brazil. Braz Oral Res. 2004;18(2):128-33. DOI: http://dx.doi.org/10.1590/S1806-83242004000200007
17. Paulozzi LJ, Lary JM. Laterality patterns in infants with external birth defects. Teratology. 1999;60(5):265-71. PMID: 10525204 DOI: http://dx.doi.org/10.1002/(SICI)1096-9926(199911)60:5<265::AID-TERA7>3.0.CO;2-H
18. Moura JR. Perfil clínico-epidemiológico dos portadores de fissuras orofaciais em residentes do estado da Bahia: um estudo descritivo [Dissertação de mestrado]. Feira de Santana: Universidade Estadual de Feira de Santana; 2014. 90 p.
1. Fundação Hospital Adriano Jorge, Manaus, AM, Brazil
2. Hospital das Clínicas de São Paulo, São Paulo, SP, Brazil
Institution: Hospital Infantil Dr. Fajardo, Manaus, AM, Brazil.
Corresponding author:
Karla Melina Gonzales Alarcón
Alameda A, Quadra C, Número 15, Conjunto Álvaro Neves, Dom Pedro II
Manaus, AM, Brazil - Zip Code 69042-221
E-mail: kmga1104@hotmail.com
Article received: January 27, 2017.
Article accepted: August 17, 2017.
Conflicts of interest: none.




 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter