

Case Report - Year 2017 - Volume 32 -
Late reconstruction of a traumatized hand with loss of multiple fingers
Reconstrução tardia na mão traumatizada com perda de múltiplos dedos
ABSTRACT
Mutilating hand injuries are a challenge to both the hand surgeon and the patient. The surgeon must make decisions ranging from the initial debridement to which fingers and joints will be preserved and the appropriate use of the parts to be removed. Late reconstruction constitutes the second part of this difficult task. The difficulty attributed to the characteristics of each lesion, the large number of treatment possibilities, and the different levels of complexity must be adapted to the personal needs and motivation of each patient. This case report describes a late hand reconstruction with index and middle finger loss, using metacarpophalangeal joint transplantation of the index finger to gain the proximal interphalangeal function of the middle finger.
Keywords: Microsurgery; Hand joint; Finger joints; Acquired hand deformities; Hand deformities; Hand trauma.
RESUMO
As lesões mutilantes de mão são um desafio para o cirurgião de mão e o paciente. O cirurgião deve tomar decisões desde o debridamento inicial, escolhendo quais dedos e articulações serão preservadas e uso apropriado das partes a serem retiradas. A reconstrução tardia é a segunda parte dessa difícil tarefa. Dificuldade que se atribui à particularidade de cada lesão, do grande número de possibilidades de tratamento e seus diversos níveis de complexidade que devem ser adequados à necessidade e motivação pessoal de cada paciente. Este relato de caso apresenta uma reconstrução tardia de mão com perda de indicador e dedo médio com transplante de articulação metacarpofalângica de indicador para função de interfalangeana proximal de dedo médio.
Palavras-chave: Microcirurgia; Articulação da mão; Articulações dos dedos; Deformidades adquiridas da mão; Deformidades da mão; Traumatismos da mão.
Mutilating hand injuries are a challenge to both the hand surgeon and the patient. The surgeon must make decisions ranging from the initial debridement to which fingers and joints will be preserved and the appropriate use of the parts to be removed.
Late reconstruction constitutes the second part of this difficult task. The difficulty attributed to the characteristics of each lesion, the large number of treatment possibilities, and the different levels of complexity must be adapted to the personal needs and motivation of each patient.
CASE REPORT AND DISCUSSION
A 61-year-old, right-handed male sustained trauma to the left hand, caused by a circular saw. This resulted in the amputation of the 2nd and 3rd fingers (F) and an injury at the base of the 4th finger. The patient was initially managed by another service, where he underwent surgical debridement and stabilization of the 2nd finger at the base of the middle phalanx and the 3rd finger at the distal third of the proximal phalanx (Figure 1). He was referred to our service due to motor and sensory deficits of the 4th finger.

Figure 1. X-ray after stabilization.
Superficial and deep flexor radial band tenorrhaphy was performed, in addition to radial digital nerve neurorrhaphy and A2 pulley reconstruction.
One year after surgery, the patient presented with restricted range of motion (ROM) of the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints, with 10-60 and 40-50 degrees of flexion, respectively. In addition, he complained of radial side hypoesthesia and pain while moving the 4th finger. He had difficulty with thumb-index finger pinch, which was very limited despite normal range of motion (ROM), and thumb-4th finger pinch, due to residual dysfunction.
The patient underwent joint transfer of the index finger MCP to gain the PIP function of the middle finger in the following stages (Figures 2 to 5):
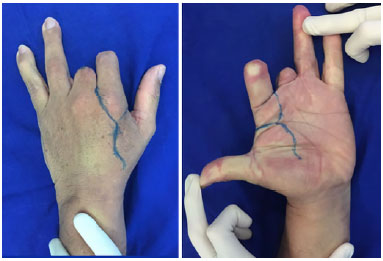
Figure 2. Design of skin flaps.
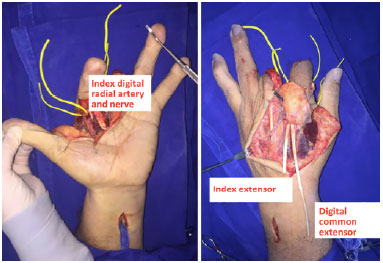
Figure 3. Isolated structures.
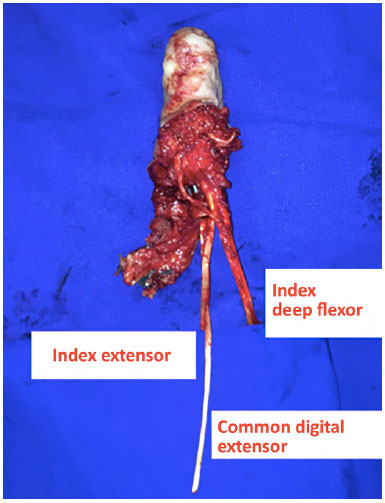
Figure 4. Isolation of the transplant.
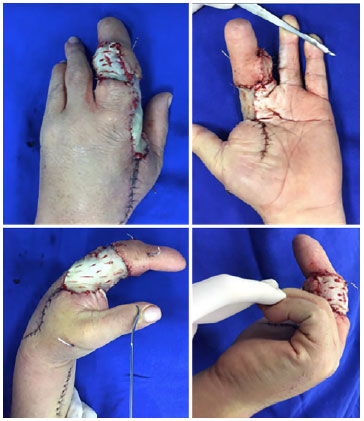
Figure 5. Final appearance after partial coverage with skin graft.
Osteosynthesis of the 2nd metacarpal to the proximal phalanx of the 3rd finger with 1.5 mm Kirschner wire;
• First flexor digitorum superficialis tenorrhaphy using the 3rd flexor digitorum superficialis at the forearm;
• Extensor indicis hood suturing on the middle finger lateral bands;
• Stabilization of the extensor indicis proprius and 1st extensor digitorum, and tenorrhaphy of the common extensor tendon toward the middle finger;
• First radial digital artery anastomosis to the 3rd radial digital artery, along with vein grafting;
• Neurorrhaphy of the 3rd radial and ulnar digital nerves;
• Residual defect coverage with partial skin grafting, one week after the joint transfer.
The patient received hand therapy for 6 months, and has 20 to 60-degree ROM at the MCP, and 10 to 20-degree flexion at the "new PIP" (Figures 6 and 7).

Figure 6. X-ray 6 months after surgery.

Figure 7. Final appearance.
The hand has 6 basic functions, according to Moran and Berger1: precision pinch, key pinch, lateral and directional pinch, hook grip, grip, and spaced grip.
Three basic functions were impaired in this patient: directional pinch, hook grip, and spaced grip. This loss was due to the absence of the PIP of normal fingers, in addition to the loss of sensibility and mobility in the 4th finger.
It was necessary to construct an "acceptable hand"2, a concept suggested by Del Piñal, in which 3 fingers are aesthetic and functional, with nearly normal length, adequate PIP ROM, and good sensitivity, in addition to a functional thumb. Therefore, in this case, it was necessary to reconstruct at least one finger that was previously amputated, and a PIP with suitable ROM and length.
Despite the results reported in the case series by Wei et al.3, the transfer of toes to the hand is still resisted by patients because of concern about the final aesthetic aspects of the donor and receiving areas. Thus, the patient refused this alternative.
PIP arthroplasty using the 4th finger had a low chance of success, since movement was painful and there was loss of radial sensitivity.
The transfer of the MCP to the middle finger could provide adequate length and stability to another finger and a better aesthetic result, and limited the donor area to the traumatized hand itself.
Obviously, this option had limitations. Foucher et al.4 compared ROM in prosthetic joint reconstructions, including vascularized and non-vascularized joint transfers of the MCP and PIP, and concluded that the ROM and PIP were smaller when compared to the MCP.
Murray et al.5 demonstrated that there was a loss of grip strength, key pinch, and supination in 20% of patients after removal of the index finger. Moreover, the force of directional grasp was reduced by 50%, due to a decrease in the lever arm in the palmar region. In the intact hand, the grasp width extends from the hypothenar eminence to the index region. The radial palm represents the external fulcrum of movement and the loss of the radial index finger decreases the fulcrum by approximately 25%.
As worrisome as the biomechanical consequences, dysesthesia is the most debilitating post-resection complication involving the radial nerve, and is caused by the formation of a neuroma. Hyperesthesia or painful sensitivity to light touch at the commissure formed between the thumb and middle finger was present in 59% of patients and interfered with hand function in 37% of the cases.
The small number of patients who did not develop a neuroma felt that removal of the radial nerve at the index finger improved grip between the thumb and middle finger. This suggests that gripping is more important than preserving grip strength for certain patients. There is also the possibility that amputation of the index finger improves carpometacarpal joint function in the remaining fingers6.
The microsurgical transfer of the MCP to achieve PIP function is a bold solution, and few reports can be found on this subject in the current literature. Further studies need to be carried out to validate this approach. If verified in the future, this may be an alternative to the surgeon's arsenal in the reconstruction of a mutilated hand.
COLLABORATIONS
RLT Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents.
HAN Final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
FCI Completion of surgeries and/or experiments.
JCN Completion of surgeries and/or experiments.
BAV Completion of surgeries and/or experiments.
THW Final approval of the manuscript.
REFERENCES
1. Moran SL, Berger RA. Biomechanics and hand trauma: what you need. Hand Clin. 2003;19(1):17-31. DOI: http://dx.doi.org/10.1016/S0749-0712(02)00130-0
2. del Piñal F. The indications for toe transfer after "minor" finger injuries. J Hand Surg Br. 2004;29(2):120-9.
3. Wei FC, Epstein MD, Chen HC, Chuang CC, Chen HT. Microsurgical reconstruction of distal digits following mutilating hand injuries: results in 121 patients. Br J Plast Surg. 1993;46(3):181-6. PMID: 8490695 DOI: http://dx.doi.org/10.1016/0007-1226(93)90165-8
4. Foucher G, Hoang P, Citron N, Merle M, Dury M. Joint reconstruction following trauma: comparison of microsurgical transfer and conventional METHODS: a report of 61 cases. J Hand Surg Br. 1986;11(3):388-93. DOI: http://dx.doi.org/10.1016/0266-7681(86)90164-6
5. Murray JF, Carman W, MacKenzie JK. Transmetacarpal amputation of the index finger: a clinical assessment of hand strength and complications. J Hand Surg Am. 1977;2(6):471-81. DOI: http://dx.doi.org/10.1016/S0363-5023(77)80029-4
6. White WL. Why I hate the index finger. Hand (N Y). 2010;5(4):461-5. DOI: http://dx.doi.org/10.1007/s11552-010-9285-5
1. Instituto de Ortopedia e Traumatologia, Faculdade de Medicina, Universidade de São Paulo, São Paulo, SP, Brasil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brasil
3. Associação Brasileira de Cirurgia da Mão, São Paulo, SP, Brasil
4. Sociedade Brasileira de Microcirurgia Reconstrutiva, São Paulo, SP, Brasil
5. Sociedade Brasileira de Ortopedia e Traumatologia, São Paulo, SP, Brasil
6. Sociedade Brasileira de Cirurgia da Mão, São Paulo, SP, Brasil
7. Universidade Estadual de Campinas, Campinas, SP, Brasil
8. Hospital A. C. Camargo, São Paulo, SP, Brasil
Institution: Instituto de Ortopedia e Traumatologia, Faculdade de Medicina, Universidade de São Paulo, São Paulo, SP, Brazil.
Corresponding author:
Renan Lyuji Takemura
Rua Carneiro da C'unha, 1266
São Paulo, SP, Brazil - Zip Code 04144-001
E-mail: lyujitakemura@yahoo.com
Article received: February 15, 2017.
Article accepted: June 7, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter