

Review Article - Year 2017 - Volume 32 -
Prevalence of body dysmorphic disorder in patients who are candidates and/or are submitted to aesthetic procedures in the specialty of plastic surgery: a systematic review with meta-analysis
Prevalência do transtorno dismórfico corporal em pacientes candidatos e/ou submetidos a procedimentos estéticos na especialidade da cirurgia plástica: uma revisão sistemática com meta-análise
ABSTRACT
This study aimed at showing the prevalence of body dysmorphic disorder (BDD) in patients who are candidates and/or are submitted to aesthetic procedures in the specialty of plastic surgery via a systematic review of the literature and a meta-analysis. To comply with the proposed objective, we analyzed the most relevant studies originally published in any language that were available in the National Library of Medicine (MEDLINE), Cochrane, and SciELO databases. Searches were performed using keywords associated with the theme and inclusion and exclusion criteria. Thus, the final sample of this study was composed of 15 publications, which were submitted to a meta-analysis. It can be confirmed that 12.5% of the patients who were candidates/submitted to aesthetic procedures in the specialty of plastic surgery had BDD. Of these, the majority were women (75.7%) with a mean age of 30 (± 10.5) years. Given the high number of patients with BDD attended to in the specialty, it is important that plastic surgeons focus on providing patients with adequate care to identify individuals who potentially have BDD and consequently conduct an interdisciplinary follow-up with the participation of psychologists and psychiatrists.
Keywords: Plastic surgery; Body dysmorphic disorder; Aesthetics; Prevalence.
RESUMO
Este estudo objetivou verificar, por meio de uma revisão sistemática da literatura e da realização de uma meta-análise, a prevalência do transtorno dismórfico corporal em pacientes candidatos e/ou submetidos a procedimentos estéticos na especialidade da Cirurgia Plástica. Para cumprir com o objetivo proposto, foram analisados os mais relevantes estudos publicados originalmente em qualquer idioma, porém, que estivessem indexados às bases de dados National Library of Medicine (MEDLINE), Cochrane e Scielo, nas quais as buscas foram realizadas, por meio do uso de descritores associados ao tema e de critérios de inclusão e exclusão. Sendo assim, a amostra final deste estudo foi composta por 15 publicações, as quais foram submetidas a uma meta-análise, podendo-se verificar que 12,5% dos pacientes que são candidatos/submetidos a procedimentos estéticos na especialidade da Cirurgia Plástica possuem transtorno dismórfico corporal. Destes, a maioria é do gênero feminino (75,7%) e possui média de idade de 30 (± 10,5) anos. Devido ao alto índice de pacientes com transtorno dismórfico corporal atendidos na especialidade, ressalta-se a importância de os cirurgiões plásticos atentarem-se para o adequado atendimento dos pacientes, com vistas à identificação dos indivíduos potencialmente portadores desse transtorno e, consequentemente, à solicitação de um acompanhamento interdisciplinar com a participação de psicólogos e psiquiatras.
Palavras-chave: Cirurgia plástica; Transtornos dismórficos corporais; Estética; Prevalência.
Aesthetic procedures have become considerably popular over the last two decades1. In 2000, more than 1.3 million aesthetic surgeries were performed in the United States alone, showing an increase of 198% in relation to that in 19922. In 2013, 1,452,356 aesthetic surgeries were performed in the United States, placing Brazil, where 1,491,721 surgeries were performed, in first place in the ranking of this type of procedure3.
Owing to the increased demand for aesthetic plastic surgery procedures, there is an increased interest in aspects related to this specialty and its patients. As an example, we can cite studies that seek to characterize the psychiatric disorders that these patients experience4-8, i.e., body dysmorphic disorder (BDD).
In general, individuals who feel that their physical characteristics do not conform to ideal standards of beauty have an increased risk of body dissatisfaction9; however, this dissatisfaction is extremely high in patients with BDD10.
In the current list of psychiatric disorders (fifth edition of the Diagnostic and Statistical Manual of Mental Disorders [DSM-5]11), the only category of diagnosis that directly addresses concerns regarding body image is BDD. Therefore, knowledge regarding this psychiatric disorder is particularly relevant to specialists in plastic surgery, considering the approach to body dissatisfaction often identified in individuals seeking exclusively aesthetic procedures.
According to the DSM-5, BDD is described as a concern with one or more defects or flaws in physical appearance that are not observable or are perceived subtly by others. In addition, BDD is characterized by repetitive behaviors and results in a clinically significant distress. These behaviors cannot be explained on the basis of normal concerns regarding physical appearance, such as body weight or shape, whether or not they are associated with muscular dysmorphia, and occur at different levels of perception11. In patients with BDD, the perception of mild physical deformities tends to be exaggerated due to underlying psychiatric or psychological problems12.
Different studies show that in the general population, the prevalence of BDD ranges from 0.7% to 2.4%, affecting mostly women, with no defined mean age13-16. However, there is a gap in the literature regarding this value in the population that is a candidate/is submitted to aesthetic procedures in the specialty of plastic surgery.
OBJECTIVE
Considering that the relationship between BDD and the specialty of plastic surgery is still poorly understood and researched, this study aimed at verifying the prevalence of BDD in patients who are candidates and/or are submitted to aesthetic procedures in plastic surgery via a systematic review of the literature and a meta-analysis.
METHODS
Search Strategy
To comply with the proposed objective, we analyzed the most relevant studies published originally in any language until January 2016 (when the search was performed), which were indexed to the United States National Library of Medicine (PubMed), Cochrane Central Register of Controlled Trials (CENTRAL), and SciELO databases, where the searches were performed.
Aiming at selecting quality scientific evidence studies, we sought publications related to meta-analyses and randomized controlled clinical trials (RCTs). The period of public publication was not initially established owing to the lack of knowledge on the number of publications on the subject available in the scientific literature.
The following combinations of keywords in Portuguese were used for the search procedure: "transtorno dismórfico corporal," "dismorfofobia," "dismorfismo corporal," "cirurgia plástica," "cirurgia estética," "cirurgia cosmética," "candidatos à cirurgia estética," and "prevalência." It is worth mentioning that the same terms were used in English in the international databases: "body dysmorphic disorder," "dysmorphophobia," "body dysmorphism," "plastic surgery," "aesthetic surgery," "cosmetic surgery," "aesthetic candidates," and "prevalence."
To identify the study designs, the terms "randomized controlled trial," "humans," and "meta-analysis" were used. Filters were not used in relation to publication dates.
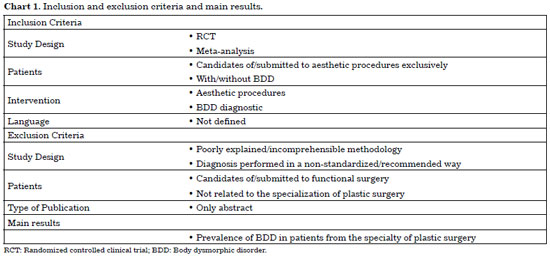
Inclusion and exclusion criteria are applied as shown in Chart 1.
RESULTS
Although we initially searched for RCTs or meta-analyses, no meta-analyses on the subject were found in the databases during the search. Therefore, only RCTs were analyzed in this study.
In addition, it is important to state that no study published in Brazil was found on the topic during the searches. However, although published in an international journal, it was possible to verify the performance of a national survey10, which is a part of the sample used in this meta-analysis.
In total, 17 publications were found that would initially be used as the basis for the data collection of this study; however, two had to be eliminated after further analysis of their methodologies owing to non-compliance with the adopted inclusion criteria. The first study that was eliminated was that of Javo and Sorlie17; despite investigating the prevalence of BDD in patients who were candidates for aesthetic procedures, they did so by sending questionnaires by e-mail to the patients, which invalidated the diagnostic method used by the authors for this study. The second excluded study was that of Metcalfe et al.18, which analyzed 188 patients (32 of whom had BDD [17.02%]), but only analyzed women who underwent breast reconstruction after mastectomy due to breast cancer; the objective of this research was related to purely aesthetic procedures.
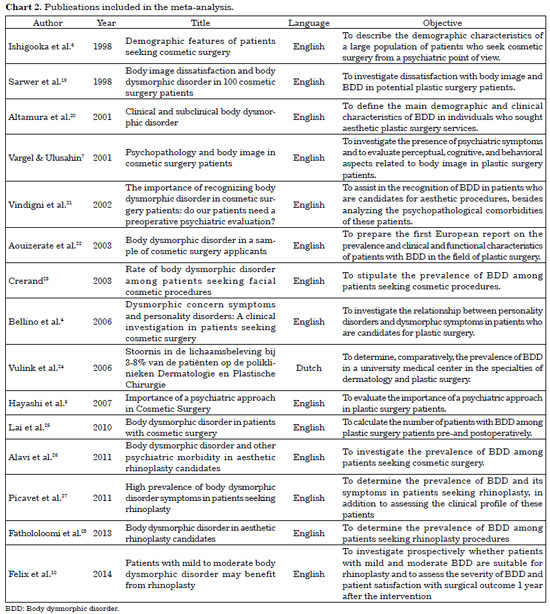
Thus, the final sample of this study was composed of 15 publications (Chart 2).
It should be noted that of those studies that made comparisons between the prevalence of BDD in patients of plastic surgery and dermatology or other specialties, only the data related to the patients who were candidates and/or were submitted to procedures of plastic surgery were collected to comply with the objective proposed in this research.
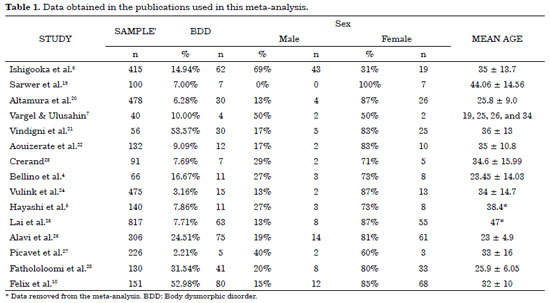
To identify the prevalence of BDD, the data regarding the number of patients included in the samples and the number of patients diagnosed with BDD were collected. In addition, we sought data regarding sex and age group, as well as the number of aesthetic procedures that the patients affected by BDD in the field of plastic surgery underwent to draw their profiles accordingly.
However, it can be reported that the data collected from the study by Felix et al.10 refer to those presented in the methodology used by the authors, considering that at a certain point, they excluded patients with severe BDD, who were included in the analysis performed in this study.
Table 1 shows the data obtained in the publications included in this meta-analysis.
As previously mentioned, this study aimed at verifying the prevalence and establishing a profile of patients with BDD in the field of plastic surgery; however, it was not possible to estimate the number of aesthetic procedures to which the patients were submitted owing to the fact that the publications did not provide these data. In addition, two studies5,25 did not present the standard deviation despite presenting the mean age of the patients with BDD, which led to the elimination of their data in the quantification of the patients' age group (as shown in Table 1).
Based on the meta-analysis performed in the 15 publications that met the inclusion and exclusion criteria established in this study, it was verified that 12.5% of the patients who were candidates and/or submitted to aesthetic procedures in the specialty of plastic surgery had BDD. Of these, the majority were women (75.7%) with a mean age of 30 (± 10.5) years.
DISCUSSION
After conducting a systematic review of the literature, it was possible to observe the lack of research conducted worldwide on the involvement of BDD in patients who were candidates for/submitted to aesthetic procedures in the specialty of plastic surgery. More specifically, it should be noted that there is no national publication on the subject, and there is only one study in Brazil that measured the prevalence of BDD in these patients10.
In the literature, a study verified the prevalence of BDD in patients who were candidates and/or were submitted to aesthetic procedures, comparing those associated with the specialty of plastic surgery with those who sought the specialty of dermatology; such a study reported that the prevalence of BDD is higher in dermatology patients (8.5%) than in plastic surgery patients (3.16%)24. However, the percentage of 3.16% found by the authors is considerably lower than the 12.5% found in this study when the meta-analysis was composed of 15 studies.
It is possible to state that the prevalence of 12.5% of the patients affected by BDD who were submitted to aesthetic procedures in plastic surgery can be considered quite high when compared with the findings of studies that analyzed the prevalence in the general population (between 0.7% and 2.4%)13-16. Even when analyzing the data of the 15 publications that were used in this meta-analysis separately, none presented a percentage within the margin found for the general population. The study that found the lowest percentage of BDD in the plastic surgery patients was that of Vulink et al.24, with a value of 3.16%, while the highest percentage was reported in the study by Vindigni et al.21 (53.57%).
It is very important for professionals to be aware of the possibility that plastic surgery patients may have BDD, not only owing to the high prevalence found in this study and the comparison of this rate with that of the general population, but also because of the findings of Biraben-Gotzamanis et al.8, which showed that six of the seven patients with BDD who underwent aesthetic plastic surgery continued to present the disorder, even 5 years after the procedure. Although the patients reported satisfaction with the results of the surgeries, their performance was not effective in reducing the symptoms of BDD, thus requiring psychological and psychiatric treatment.
Therefore, it is believed that the correct diagnosis and treatment of BDD can improve patients' self-esteem and quality of life more effectively than aesthetic procedures of plastic surgery that were not efficient based on the survey findings by Biraben-Gotzamanis et al.8. A multidisciplinary follow-up of patients who are candidates for aesthetic procedures of plastic surgery is necessary to assist them better and obtain excellent results both for the patients and professionals involved.
In addition, we emphasize that further research studies with different methodologies are required to explain better the prevalence of BDD in plastic surgery patients, mainly in Brazil, where the subject is still poorly studied.
CONCLUSION
Based on the meta-analysis, it was concluded that 12.5% of the patients who were candidates and/or submitted to exclusively aesthetic procedures of plastic surgery had BDD, with a dominance of women with a mean age of 30 years.
Considering the high number of patients with BDD attended to in the specialty, it is important that plastic surgeons focus on providing patients with adequate care to identify individuals who potentially have BDD and consequently conduct an interdisciplinary follow-up with the participation of psychologists and psychiatrists.
COLLABORATIONS
RVER Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
GBS Final approval of the manuscript; writing the manuscript or critical review of its contents.
FVA Final approval of the manuscript.
REFERENCES
1. Sarwer DB, Crerand CE. Body image and cosmetic medical treatments. Body Image. 2004;1(1):99-111. DOI: http://dx.doi.org/10.1016/S1740-1445(03)00003-2
2. Ching S, Thoma A, McCabe RE, Antony MM. Measuring outcomes in aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg. 2003;111(1):469-80; discussion 481-2. DOI: http://dx.doi.org/10.1097/00006534-200301000-00085
3. ISAPS. International Survey on Aesthetic/Cosmetic. Procedures Performed in 2013. [base de dados online]. 2014 [citado 2014 Out 10]. Disponível em: http://www.isaps.org/Media/Default/global-statistics/2014 ISAPS Global Stat Results.pdf
4. Bellino S, Zizza M, Paradiso E, Rivarossa A, Fulcheri M, Bogetto F. Dysmorphic concern symptoms and personality disorders: a clinical investigation in patients seeking cosmetic surgery. Psychiatry Res. 2006;144(1):73-8. PMID: 16914206 DOI: http://dx.doi.org/10.1016/j.psychres.2005.06.010
5. Hayashi K, Miyachi H, Nakakita N, Akimoto M, Aoyagi K, Miyaoka H, et al. Importance of a psychiatric approach in cosmetic surgery. Aesthet Surg J. 2007;27(4):396-401. DOI: http://dx.doi.org/10.1016/j.asj.2007.05.010
6. Ishigooka J, Iwao M, Suzuki M, Fukuyama Y, Murasaki M, Miura S. Demographic features of patients seeking cosmetic surgery. Psychiatry Clin Neurosci. 1998;52(3):283-7. PMID: 9681579 DOI: http://dx.doi.org/10.1046/j.1440-1819.1998.00388.x
7. Vargel S, Uluşahin A. Psychopathology and body image in cosmetic surgery patients. Aesthetic Plast Surg. 2001;25(6):474-8. DOI: http://dx.doi.org/10.1007/s00266-001-0009-7
8. Biraben-Gotzamanis L, Aouizerate B, Martin-Guehl C, Grabot D, Tignol J. Body dysmorphic disorder et chirurgie esthétique: réévaluation de 24 sujets ayant un défaut minime de l'apparence 5 ans après leur demande de chirurgie esthétique. Presse Med. 2009;38(7-8):1062-7. DOI: http://dx.doi.org/10.1016/j.lpm.2008.07.025
9. Veale D. Body dysmorphic disorder. Postgrad Med J. 2004;80(940):67-71. PMID: 14970291 DOI: http://dx.doi.org/10.1136/pmj.2003.015289
10. Felix GA, Brito MJ, Nahas FX, Tavares H, Cordas TA, Dini GM, et al. Patients with mild to moderate body dysmorphic disorder may benefit from rhinoplasty. J Plast Reconstr Aesthet Surg. 2014;67(5):646-54. PMID: 24508222 DOI: http://dx.doi.org/10.1016/j.bjps.2014.01.002
11. American Psychiatric Association (APA). Obsessive-compulsive and related disorders. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: APA; 2013.
12. Bjornsson AS, Didie ER, Phillips KA. Body dysmorphic disorder. Dialogues Clin Neurosci. 2010;12(2):221-32.
13. Buhlmann U, Glaesmer H, Mewes R, Fama JM, Wilhelm S, Brähler E, et al. Updates on the prevalence of body dysmorphic disorder: a population-based survey. Psychiatry Res. 2010;178(1):171-5. DOI: http://dx.doi.org/10.1016/j.psychres.2009.05.002
14. Koran LM, Abujaoude E, Large MD, Serpe RT. The prevalence of body dysmorphic disorder in the United States adult population. CNS Spectr. 2008;13(4):316-22. DOI: http://dx.doi.org/10.1017/S1092852900016436
15. Otto MW, Wilhelm S, Cohen LS, Harlow BL. Prevalence of body dysmorphic disorder in a community sample of women. Am J Psychiatry. 2001;158(12):2061-3. DOI: http://dx.doi.org/10.1176/appi.ajp.158.12.2061
16. Rief W, Buhlmann U, Wilhelm S, Borkenhagen A, Brähler E. The prevalence of body dysmorphic disorder: a population-based survey. Psychol Med. 2006;36(6):877-85. DOI: http://dx.doi.org/10.1017/S0033291706007264
17. Javo IM, Sørlie T. Psychosocial predictors of an interest in cosmetic surgery among young Norwegian women: a population-based study. Plast Surg Nurs. 2010;30(3):180-6. DOI: http://dx.doi.org/10.1097/PRS.0b013e3181bcf290
18. Metcalfe DB, Duggal CS, Gabriel A, Nahabedian MY, Carlson GW, Losken A. Prevalence of Body Dysmorphic Disorder Among Patients Seeking Breast Reconstruction. Aesthet Surg J. 2014;34(5):733-7. DOI: http://dx.doi.org/10.1177/1090820X14531775
19. Sarwer DB, Wadden TA, Pertschuk MJ, Whitaker LA. Body image dissatisfaction and body dysmorphic disorder in 100 cosmetic surgery patients. Plast Reconstr Surg. 1998;101(6):1644-9. PMID: 9583501 DOI: http://dx.doi.org/10.1097/00006534-199805000-00035
20. Altamura C, Paluello MM, Mundo E, Medda S, Mannu P. Clinical and subclinical body dysmorphic disorder. Eur Arch Psychiatry Clin Neurosci. 2001;251(3):105-8. PMID: 11697569 DOI: http://dx.doi.org/10.1007/s004060170042
21. Vindigni V, Pavan C, Semenzin M, Granà S, Gambaro FM, Marini M, et al. The importance of recognizing body dysmorphic disorder in cosmetic surgery patients: do our patients need a preoperative psychiatric evaluation? Eur J Plast Surg. 2002;25(6):305-8.
22. Aouizerate B, Pujol H, Grabot D, Faytout M, Suire K, Braud C, et al. Body dysmorphic disorder in a sample of cosmetic surgery applicants. Eur Psychiatry. 2003;18(7):365-8. DOI: http://dx.doi.org/10.1016/j.eurpsy.2003.02.001
23. Crerand CE. Rate of body dysmorphic disorder among patients seeking facial cosmetic procedures [Thesis]. Philadelphia: Drexel University; 2003.
24. Vulink NC, Sigurdsson V, Kon M, Bruijnzeel-Koomen CA, Westenberg HG, Denys D. Stoornis in de lichaamsbeleving bij 3-8% van de patiënten op de poliklinieken Dermatologie en Plastische Chirurgie. Ned Tijdschr Geneeskd. 2006;150(2):97-100.
25. Lai CS, Lee SS, Yeh YC, Chen CS. Body dysmorphic disorder in patients with cosmetic surgery. Kaohsiung J Med Sci. 2010;26(9):478-82. DOI: http://dx.doi.org/10.1016/S1607-551X(10)70075-9
26. Alavi M, Kalafi Y, Dehbozorgi GR, Javadpour A. Body dysmorphic disorder and other psychiatric morbidity in aesthetic rhinoplasty candidates. J Plast Reconstr Aesthet Surg. 2011;64(6):738-41. PMID: 21269896 DOI: http://dx.doi.org/10.1016/j.bjps.2010.09.019
27. Picavet VA, Prokopakis EP, Gabriëls L, Jorissen M, Hellings PW. High prevalence of body dysmorphic disorder symptoms in patients seeking rhinoplasty. Plast Reconstr Surg. 2011;128(2):509-17. PMID: 21788842 DOI: http://dx.doi.org/10.1097/PRS.0b013e31821b631f
28. Fathololoomi MR, Tabrizi AG, Bafghi AF, Noohi SA, Makhdoom A. Body dysmorphic disorder in aesthetic rhinoplasty candidates. Pak J Med Sci. 2013;29(1):197-200.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Municipal Barata Ribeiro, Rio de Janeiro, RJ, Brazil
3. Hospital e Maternidade Therezinha de Jesus, Juiz de Fora, MG, Brazil
4. Hospital Universitário Pedro Ernesto, Rio de Janeiro, RJ, Brazil
5. Hospital Santa Isabel, Ubá, MG, Brazil
Institution: Hospital e Maternidade Therezinha de Jesus, Juiz de Fora, MG, Brazil.
Corresponding author:
Rafael Vilela Eiras Ribeiro
Avenida Itamar Franco, 4001 - Dom Bosco
Juiz de Fora, SP, Brazil - Zip Code 36033-318
E-mail: vilelaeiras@hotmail.com
Article received: November 28, 2016.
Article accepted: February 21, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter