

Original Article - Year 2017 - Volume 32 -
Gluteoplasty using the Intramuscular (XYZ) Method
Gluteoplastia Técnica Intramuscular (XYZ)
ABSTRACT
INTRODUCTION: The shape and size of the buttocks are essential to the notion of bodily beauty. This has resulted in a growing interest in gluteoplasty among both women and men. The aim of the present study was to present the author's experience with gluteoplasty using the intramuscular XYZ method.
METHOD: Between 2010 and 2015, 29 patients aged 22 to 64 years (average, 43 years) underwent gluteoplasty; of these 26 were women (89.66%) and 3 were men (10.34%). Round or oval implants were used, with volumes of 240 to 420 ml (average, 330 ml), depending on the individual case.
RESULTS: Good results were obtained in terms of volume increase and harmony of the gluteal region, with a high degree of patient satisfaction.
CONCLUSIONS: The intramuscular XYZ method was safe, both for primary and secondary surgery, to treat cases of asymmetry and/or visible implants. Predetermining the XYZ reference points makes this procedure safe and reproducible.
Keywords: Reconstructive surgical procedures; Buttocks; Silicone elastomers; Prosthesis and implants.
RESUMO
INTRODUÇÃO: No conceito de beleza corporal, a forma e o tamanho das nádegas são fundamentais, provocando uma crescente busca não só de mulheres, como também de homens, pela cirurgia de gluteoplastia. O objetivo deste trabalho é apresentar a experiência do autor em gluteoplastia com a técnica intramuscular (XYZ).
MÉTODO: No período de 2010 a 2015 foram operados 29 pacientes com idades entre 22 e 64 anos (média 43 anos), sendo 26 mulheres (89,66%) e três homens (10,34%). Foram usados implantes redondos ou ovais, com volumes entre 240 e 420 ml (média de 330 ml), dependendo da melhor indicação para cada caso.
RESULTADOS: Foram obtidos bons resultados sob o aspecto de aumento de volume e harmonia da região glútea, com alto índice de satisfação dos pacientes.
CONCLUSÕES: Na casuística do estudo a técnica intramuscular (XYZ) se mostrou segura, tanto nas cirurgias primárias como nas cirurgias secundárias, para tratar casos de assimetria e/ou implantes visíveis. Com a pré- determinação dos pontos fixos XYZ, o procedimento torna-se seguro e reprodutível.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Nádegas; Elastômeros de silicone; Próteses e implantes.
Body shape enhancement is increasingly desired, especially in tropical countries like Brazil, where the body is highly exposed. Buttocks are made up of muscles, which are responsible for moving the lower limbs and keeping the torso erect1. Gluteoplasty aims to enhance body shape, and the number of patients undergoing gluteoplasty has been growing worldwide. In the USA, there was an 86% increase in gluteoplasties between 2013 and 2014.
Silicone implants are used in aesthetic procedures for the gluteal region. This method was introduced by Bartels in 1969, placing subcutaneous mammary implants through an incision in the gluteal cleft. In 1984, Robles introduced the submuscular implant method, with an incision in the intergluteal cleft. In 1996, Vergara and Marcos described an intramuscular implant method2, and in 2004, De La Peña described a subfascial method. In 2004, Gonzalez3 established the parameters for intramuscular detachment with marking of fixed anatomical points to guide dissection, avoiding extramuscular implantation, which may be visible and/or palpable.
OBJECTIVE
The aim of this report is to present the author's experience in gluteoplasty using the intramuscular XYZ method.
METHODS
Between 2010 and 2015, 29 gluteoplasties were performed using the intramuscular XYZ method at the Tabancura Clinic in Santiago, Chile; of these, 26 were performed on women and 3 on men, aged between 22 and 64 years (average, 43 years). All gluteoplasty patients operated on by the author during this period were included in the present study. Buttock-specific implants with volumes between 240 and 420 ml (average, 330 ml) were used in all cases, of which 12 were round and 17 oval (in men, all were round). Twenty-six cases were performed for aesthetic correction of gluteal hypoplasia, and 3 were reoperations due to asymmetry and/or implant visibility, following surgery by others. The study was conducted in accordance with the Helsinki principles.
Method
All patients underwent surgery under general anesthesia. An upper point, A, was marked in the intergluteal cleft with the patient in standing position. This point is extremely important to guarantee that the scar is hidden in the intergluteal cleft. Following anesthesia, antisepsis was performed with the patient prone, using disinfecting povidone, topical povidone, and a gauze plug with topical povidone in the anus, which is covered with a compress sutured to the skin.
The XYZ points, described by Gonzalez3, were then marked (Figure 1). Point X, lateral to the sacrum, was defined to initiate undermining where the gluteus maximus (GM) is thickest (4-7 cm). Point X is located at the midpoint of GM thickness, at an average of 3 cm deep. Even in very thin patients, it should never be less than 2.5 cm deep to achieve good muscle cover. Point Y is 4-5 cm lateral the posterior superior iliac spine, and marks the lateral limit of the GM4.
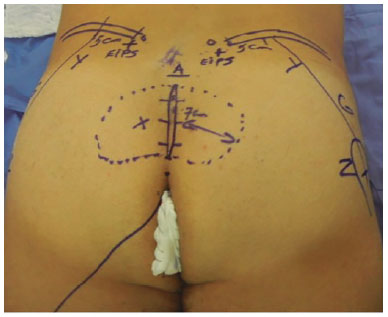
Figure 1. Preoperative marking.
At point Y, the iliac crest is moved caudally by pressing the lateral border of the GM. Point Y is also located at the midpoint of GM thickness, but at its lateral part. Point Z is determined as the closest point to the trochanter over line G. Line G delimits the lateral limit of the GM, and is marked on the skin as a line beginning at point Y and ending at point Z. After points XYZ are determined, the intergluteal cleft, the area to be undermined corresponding to the size of the implant, and both GMs are infiltrated with saline-adrenaline solution (1:500,000).
A needle is used in the areas of incision and undermining, and 20-cm × 1.8-mm cannulas are used for muscle infiltration (Figure 2). Each GM is infiltrated with 100 ml of solution. Starting at point A, an elliptical area 5-7-cm long and 0.5-cm wide is marked in the caudal direction. The skin incision is perpendicular until the subcutaneous tissue is reached, then angles at 45º in the subcutaneous tissue in the direction of the muscle fascia, leaving the base of the island flap (sacrocutaneous ligament)3 as large as possible (Figure 3, A and B).
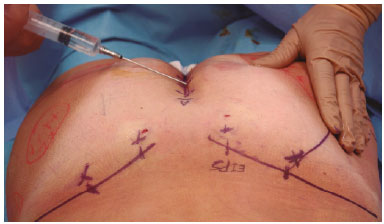
Figure 2. Gluteal infiltration.
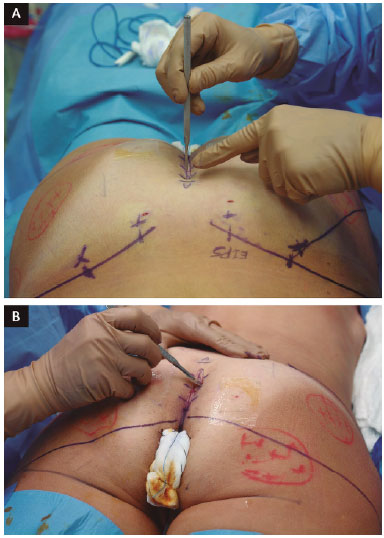
Figure 3. A: Skin island incision; B: Preservation of the sacrocutaneous ligament.
Initially, undermining is performed in the suprafascial plane, preserving the fascia over a distance of approximately 5-7 cm, sufficient to introduce the implant. At point X (Figure 4), a fissure is created parallel to the muscle fibers, and a straight underminer is introduced to a depth of 3 cm by blunt dissection (Figure 5). Once the underminer is introduced, it is tilted to 45º and pushed in the direction of point Y until it reaches the iliac crest. The underminer is then rotated cephalocaudally, with line G as the lateral limit, and pushed in the direction of point Z, i.e., close to the trochanter.

Figure 4. Point X.
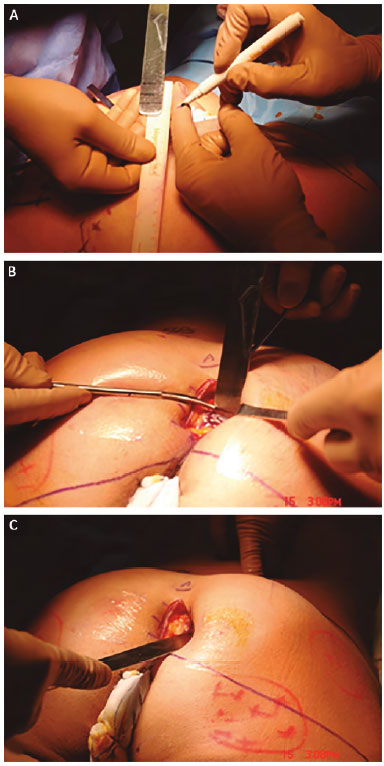
Figure 5. Detachment of the gluteus maximus.
At this time, the XYZ area is detached, and the dissection is completed using a "duckbill" muscle separator3 (Figure 6). Hemostasis is verified, 2 compresses soaked in epinephrine solution (1:500,000) are placed, and the procedure is repeated on the contralateral side. The compresses are removed, and hemostasis is verified using fiber optics, ensuring a good muscle cover (Figure 7).

Figure 6. Sheath creation using a duckbill separator.
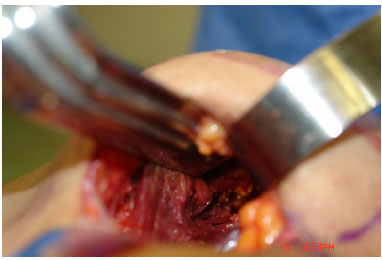
Figure 7. Review of the muscle cover.
Test inserts are placed, and the one providing best shape and volume is selected. The testers are removed, vacuum aspiration drains are placed inside the muscle sheath, and are removed through a counter-opening in the suprasacral area. Three 1-0 polyglactin sutures are passed in the margins of the GM. The implants are then placed, so that the muscles can be sutured without tension, using the previously prepared sutures (Figure 8).

Figure 8. Placement of the implant without muscular tension.
Adhesion points in the detached subcutaneous tissue5, and points between the gluteus dermis-fat flap and the island of deepithelialized skin (sacrocutaneous ligament)3, were apposed with 3-0 polyglactin sutures. Skin closure was performed using simple 5-0 monofilament nylon sutures. This area is kept uncovered for daily hygiene and treatment with topical povidone twice a day. In the immediate postoperative period, patients are placed in a sitting position on pillows, with no pressure in the gluteal area. Ambulation is permitted on the first postoperative day.
Complications and Solutions
Pain was the most frequent immediate complication, but we observed less pain intensity when the patients were placed in a sitting position in the immediate postoperative period. Postoperative edema is believed to affect the sciatic nerve less intensely than when the patient is prone. The sensory component of the sciatic nerve is very sensitive to edema/bloody exudate6, and may cause pain radiating to the back of the leg, causing sciatica7.
A late complication is muscle atrophy, which may be related to a thin muscle cover in surgery. Both late seroma, mainly associated with textured implants, and implant rotation, resulting from the widening of the sheath, can result in visible implants8.
Of the 29 patients, 26 were primary surgeries and 3 were reoperations. Suture dehiscence was the most frequent complication, occurring in 4 cases (13%) (Figure 9); asymmetry occurred in 1 case (3.44%). Dehiscence was treated with local dressings and spontaneous closure; 2 cases were closed with stitches, and the case of asymmetry was re-operated with good results (Figure 10).

Figure 9. Skin dehiscence.
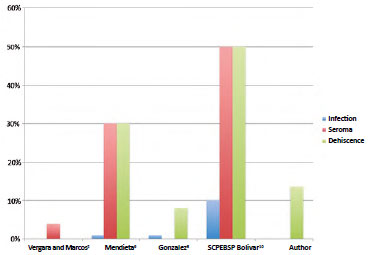
Figure 10. Distribution of complications.
In cases of asymmetry and/or visibility of implants resulting from surgeries by others, we removed the implants and treated the capsule with radial incisions and suture of the deep and superficial leaflets, using continuous stitches to lift the gluteal dermocutaneous flap. The patients were followed with ultrasonography, and when the GM presented a minimum thickness of 3 cm, which occurred at 4 to 6 months, reoperation was performed to place the intramuscular implants (Figure 11 A and B). There were no cases of hematoma or infection. One case of dehiscence evolved into a fistula from the capsule to the subcutaneous tissue, and was treated with fistulectomy, using local anesthesia following magnetic resonance imaging of the fistula (Figure 12).
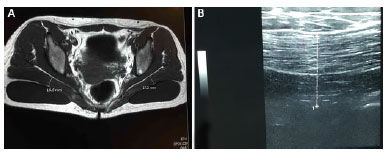
Figure 11. Magnetic resonance imaging for preoperative planning.
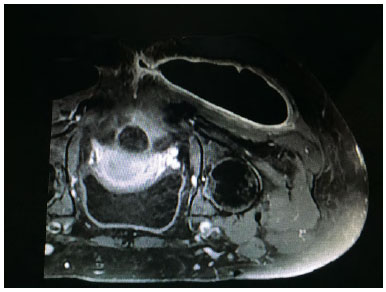
Figure 12. Magnetic resonance imaging of fistula.
RESULTS
Good results and patient and author satisfaction with natural and harmonious contours in both shape and volume were achieved in the 29 patients. Liposuction of the waist and/or filling of previously marked areas5, especially areas of trochanteric depression, were also performed in several patients (Figure 13 and 14).
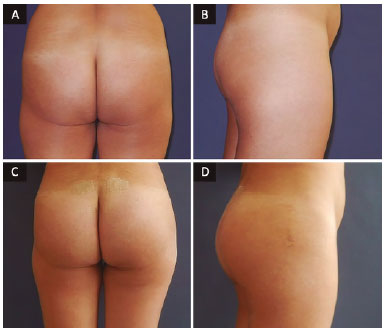
Figure 13. Patient, 33 years old, round implant 270 ml. A and B: Preoperative; C and D: Postoperative.
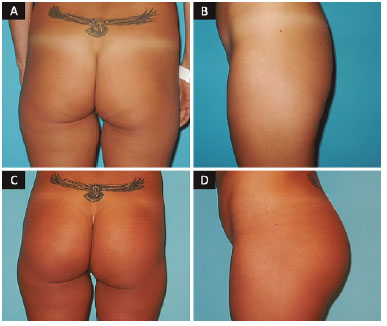
Figure 14. Patient, 38 years old, oval implant 365 ml. A and B: Preoperative; C and D: Postoperative.
DISCUSSION
Buttock shape and size are essential to the notion of female beauty and sensuousness. Several authors have developed methods to improve buttock shape and volume. Initially, the methods of implant placement in the subcutaneous and subfascial planes presented a high percentage of complications, such as asymmetry and visible implants.
The Robles submuscular method limits the size and position of the implants, but carries great risk of injury to the sciatic nerve. Vergara and Marcos2 introduced an intramuscular method in which a wider sheath and better position of the implant are obtained, with more harmonious results. Gonzalez3 established anatomical parameters, using fixed points for safe and uniform undermining. He described an intramuscular implant method in which points XYZ are fixed, determine the area of undermining, and line G indicates the external limit of the sheath relative to the lateral limit of the GM.
With these parameters, the sheath can be established safely and uniformly, avoiding asymmetry and/or visible implants. The 2 implant models are round or oval, and several subtypes have a flat or concave base, high/low projection, and textured or smooth surface. We prefer smooth implants, in order to avoid the frequent late seromas associated with textured implants.
In male patients, the layer of fatty tissue is thinner than in women, and the probability of visible implants is therefore higher. Round implants have higher projection and allow for larger volume, being indicated for "short" buttocks. In very thin women and/or those with flaccid skin, round implants should be avoided because of the high probability of being visible. In these cases, it is better to use oval implants. These are more versatile, and can be placed vertically, at 45º, or horizontally6.
There was one case of asymmetry among the primary patients,. All other cases were considered by the authors and patients as good from an aesthetic point of view, including the reoperation cases. Whenever necessary, liposuction and/or fat grafting were also performed, in order to achieve better aesthetic results11.
Our aim of achieving an aesthetic result that meets patient expectations is limited to the size of the GM. The patients should therefore be informed clearly of this anatomical limitation to the implant size, in order to avoid subsequent dissatisfaction.
CONCLUSION
Gluteoplasty has the highest annual growth, worldwide. It is currently increasing by 42% per year in Brazil, and increased by 86% in the USA between 2013 and 2014. The intramuscular method was observed to be safe and reproducible, as long as there is good knowledge of the regional anatomy. We believe that this accounts for this increase in the number of gluteoplasties. The fixed points XYZ described by Gonzalez greatly improved the safety and reproducibility of this method, and adjusted the placement of larger implants with better aesthetic positioning. Augmentation gluteoplasty using the XYZ method is safe and reproducible, providing satisfactory results in the opinion of the author and his patients.
COLLABORATIONS
ADC Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
JVF Critical review of its contents.
DG Completion of surgeries and/or experiments.
REFERENCES
1. Drake RL, Vogl AW, Mitchell AWM. Gray's - Anatomia Clínica Para Estudantes - 3ª Ed. Rio de Janeiro: Elsevier; 2015.
2. Vergara R, Marcos M. Intramuscular gluteal implants. Aesthetic Plast Surg. 1996;20(3):259-62. DOI: http://dx.doi.org/10.1007/s002669900030
3. Gonzalez R. Augmentation gluteoplasty: the XYZ method. Aesthetic Plast Surg. 2004;28(6):417-25. DOI: http://dx.doi.org/10.1007/s00266-004-3130-6
4. Serra F, Aboudib JH, Cedrola JP, de Castro CC. Gluteoplasty: anatomic basis and technique. Aesthet Surg J. 2010;30(4):579-92. DOI: http://dx.doi.org/10.1177/1090820X10380389
5. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41. PMID: 19328174 DOI: http://dx.doi.org/10.1016/S1090-820X(98)70073-1
6. Gonzalez R. Gluteoplastia: Passo a passo da cirurgia do contorno posterior. Rio de Janeiro: Indexa; 2008.
7. Gonzalez R. A simple way to avoid sciatic pain after intramuscular gluteal implant. Aesthetic Plast Surg. 2007;31(5):602-3. DOI: http://dx.doi.org/10.1007/s00266-007-0058-7
8. Gonzalez R. Gluteal implants: the "XYZ" intramuscular method. Aesthet Surg J. 2010;30(2):256-64. DOI: http://dx.doi.org/10.1177/1090820X10369213
9. Mendieta CG. Intramuscular gluteal augmentation technique. Clin Plast Surg. 2006;33(3):423-34.
10. Azevedo DM, Gonçalves Junior P, Pereira J, Amoedo TB, Kuroyanagi FM, Cotes EFM, et al. Gluteoplastia de aumento: experiência do Serviço de Cirurgia Plástica Dr. Ewaldo Bolivar de Souza Pinto. Rev Bras Cir Plást. 2012;27(1):87-92.
11. Rodrigues Neto JN, Guimarães GS, Benedik Neto A, Cammarota MC, Daher JC. Prótese glútea: o uso da lipoaspiração na melhora dos resultados. Rev Bras Cir Plast. 2010;25(2):344-8.
1. Clínica Tabancura, Santiago, Chile
2. Faculdade de Medicina de Pouso Alegre, Pouso Alegre, MG, Brazil
3. Sociedade Chilena de Cirurgia Plástica, Reconstrutiva e Estética, Santiago, Chile
Institution: Clínica Tabancura, Santiago, Chile.
Corresponding author:
Antonio Donizeti Castilho
Av. Kennedy, 7100
Of. 906 Vitacura - Santiago, Chile
E-mail: castplast@gmail.com
Article received: May 12, 2016.
Article accepted: September 19, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter