

Original Article - Year 2017 - Volume 32 -
Marking of neo-omphaloplasty flaps using a standardized mold in anchor-line abdominoplasty
Marcação dos retalhos da neo-onfaloplastia com emprego de molde padronizado na abdominoplastia em âncora
ABSTRACT
INTRODUCTION: Abdominal dermolipectomies have shown to be highly valuable in promoting a better life quality for post-bariatric patients, with the navel being an essential scar for the aesthetics of the abdomen. Several neo-omphaloplasty techniques are described in the literature in patients who undergo anchor-line abdominoplasty, but the systematic use of a mold for preoperative marking has not been reported yet. The objective of this study was to standardize the marking of the flaps for the preparation of the neo-omphaloplasty using a mold and to demonstrate the results of its clinical application.
METHODS: A prospective, descriptive, and analytical study was conducted. Between April 2015 and December 2016, 50 patients underwent anchor-line abdominal dermolipectomy with neo-omphaloplasty using a mold to mark the two flaps for the neo-navel. A questionnaire was used to evaluate the satisfaction index regarding the new navel.
RESULTS: Forty-eight patients were female. The mean age and body mass index of the patients before abdominoplasty was 40.5 years and 27.9 kg/m2, respectively. The new navels resulted in a smaller, more oval scar, with no scars around and with adequate depth. The rate of complications was low, and none of the patients expressed dissatisfaction.
CONCLUSION: The use of the mold in the standardization of the preoperative marking in neo-omphaloplasty was effective, easy and safe to learn, low-cost, fast, and reproducible, with a low index of complications, good surgical results, and excellent patient satisfaction.
Keywords: Navel; Reconstructive surgical procedures; Bariatric surgery; Abdominoplasty.
RESUMO
INTRODUÇÃO: As dermolipectomias abdominais têm se mostrado altamente valiosas na promoção de melhor qualidade de vida para pacientes pós-bariátricos, sendo o umbigo uma cicatriz essencial para beleza de um abdome. Várias técnicas de neo-onfaloplastia são descritas na literatura para os pacientes submetidos à abdominoplastia em âncora, porém não há registro do uso sistemático de um molde para marcação pré-operatória. O objetivo é padronizar a marcação dos retalhos para confecção da neo-onfaloplastia com emprego de um molde e demonstrar os resultados da sua aplicação clínica.
MÉTODOS: Estudo prospectivo, descritivo e analítico. Entre abril de 2015 e dezembro de 2016, 50 pacientes foram submetidos à dermolipectomia abdominal em âncora com neo-onfaloplastia utilizando molde para marcação dos dois retalhos para confecção do neoumbigo. Foi utilizado um questionário para avaliar o índice de satisfação em relação ao novo umbigo.
RESULTADOS: Quarenta e oito pacientes eram do gênero feminino, a idade média foi de 40,5 anos e índice de massa corporal médio de 27,9 kg/m2 antes da abdominoplastia. Os novos umbigos resultaram em uma cicatriz pequena, com formato mais ovalado, sem cicatrizes ao redor e com profundidade adequada. Ocorreu baixo índice de complicações e não houve insatisfação nos pacientes estudados.
CONCLUSÃO: O uso do molde na padronização da marcação pré-operatória da neo-onfaloplastia mostra-se eficaz, com aprendizado fácil e seguro, apresenta baixo custo, é rápido, reprodutível, com baixo índice de complicações e bons resultados cirúrgicos, com excelente satisfação dos pacientes.
Palavras-chave: Umbigo; Procedimentos cirúrgicos reconstrutivos; Cirurgia bariátrica; Abdominoplastia.
Obesity is considered a global pandemic related to genetic, endocrine, behavioral, and environmental factors that brings significant health risks to the population and needs to be considered as a disease that requires specialized treatment1,2.
In the last decades, the number of patients who undergo bariatric surgery has significantly increased owing to the technical progress and safety of the procedures, providing excellent results in weight loss, improved quality of life, and reduction of risk factors for the health of individuals. Currently, the United States is the champion country in the number of bariatric surgeries performed, followed by Brazil with 93,500 surgeries in 2015, with a gradual increase each year2,3.
In Brazil, in 2004, the chapter on post-bariatric surgery was founded by the Brazilian Society of Plastic Surgery, an important step for scientific expansion. National surgeons such as Humberto Cardoso Resende, Roberto Kaluf, Wilson Cintra, Alfredo Donnabella, Carlos Del Pino Roxo, and Edimar Maciel are important for expanding their experience and knowledge in this new group of patients referred to as formerly obese4.
With weight loss, these patients present themselves to plastic surgeons with various body deformities and need for repair to improve their self-esteem and restore their normal physical activities. Abdominal dermolipectomies have been shown to be highly valuable in promoting the quality of life of post-bariatric patients. Literatures show that umbilicoplasty is often a weak point in the results of abdominoplasty, as it causes dissatisfaction among patients and surgeons5-7.
The navel is an essential scar for the aesthetics of the abdomen. However, this concept was not used in the first techniques of abdominoplasty performed by Kelly and Peters, among others, in the late nineteenth century in France because they did not give importance to the navel and performed the removal of the umbilical scar near the flap. The attention to the navel later began with greater intensity in the mid-twentieth century, with publications by Thorek, Vernon, and Galtier, among others, who underwent abdominoplasty with preservation of the umbilical scar8,9.
Several neo-omphaloplasty techniques are described in the literature in patients undergoing anchor-line abdominoplasty10,11, but the systematic use of a mold for preoperative marking has not been reported yet.
OBJECTIVE
This study was aimed at standardizing the marking of the flaps for neo-omphaloplasty with the use of a mold in anchor-line abdominoplasty and to demonstrate the results of its clinical application.
METHODS
A prospective, descriptive, and analytical study was conducted, following the ethical principles of the Declaration of Helsinki, between April 2015 and December 2016 at the Hospital and Maternity Therezinha de Jesus, Monte Sinai Hospital (Juiz de Fora, MG, Brazil) and Hospital Felício Rocho (Belo Horizonte, MG, Brazil). Fifty patients with abdominal dermatolipodystrophy after gastroplasty were treated. The first author performed anchor-line abdominal dermolipectomy with neo-onfaloplasty using a preoperative mold in all the patients. The mold was used to mark the two flaps for the neo-navel construction.
The inclusion criteria in the study were patients of both sexes, aged between 18 and 70 years, who had undergone laparotomic or videolaparoscopic gastroplasty, abdominal dermatolipodystrophy with horizontal and vertical cutaneous excess, or bariatric surgery at least 1 year before; had stable weight for at least 3 months; and had normal clinical and laboratory examination results. The exclusion criteria were patients who did not perform adequate postoperative follow-up. The criteria for non-inclusion were smokers and patients with psychiatric disorders.
The variables studied were sex, age, body mass index (BMI) before abdominoplasty, time interval between bariatric surgery and abdominoplasty, gastroplasty method (laparoscopic or laparotomic), time of hospital discharge, complications, and follow-up. The data were entered for statistical analysis in Microsoft Office Excel software spreadsheets. The related literatures were reviewed, and the databases consulted were PubMed and LILACS.
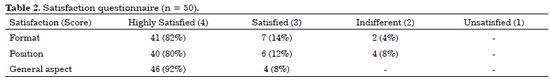
A questionnaire that was previously used in two publications specific to umbilicoplasty was used in this study for a simple and objective assessment of satisfaction with the new navel12.13. The patients were asked to evaluate three items, namely shape, position, and overall appearance. The scores ranged from 1 to 4, where 1 corresponds to poor/unsatisfied; 2, indifferent; 3, satisfied; and 4, excellent/highly satisfied.
The authors declare no conflicts of interest and funding sources.
Mold
The mold for marking the flaps of the new navel was produced with a radiographic film. The mold presents measurements of 15.5 cm in height and 2.5 cm in width. In accordance with the topography of the marking of the flaps of the new navel, the mold has an extension with a 1.5-cm width and 2-cm height in its most distal portion, with a curvilinear transition to its base 3.5 cm high. At the bottom of this extension, the mold has a 10-cm complement that allows for better adjustment of the position of the height of the neo-navel (Figure 1).
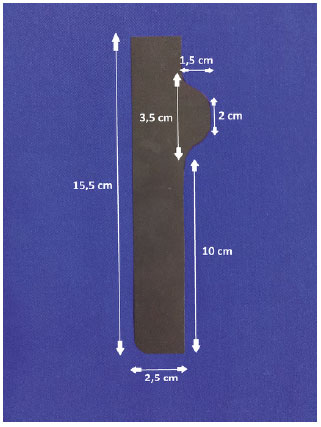
Figure 1. Measurements of the mold.
Preoperative marking
A rationalized marking of the cutaneous surplus is performed with the patient in orthostatic position (Figure 2). Point A is marked on the most cranial projection of the cutaneous excess. Point C is marked approximately 5 to 6 cm from the vaginal wishbone or penile base with the help of the patient, raising the excess skin of the pubic region, which allows planning a lifting of the pubic region.
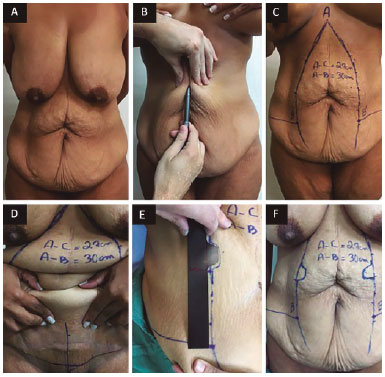
Figure 2. A: Patient standing; B: Clamping and imbrication to evaluate the excess skin to be resected vertically; C: Front view of the cutaneous demarcations of the vertical cutaneous excess; D: Point C marked approximately 5 cm from the vaginal wishbone with the patient's help in raising the excess skin of the pubic area, which allows planning for lifting of the pubic area. At this point, distance AC is measured and transferred to lines AB and AB', adding 3 cm; E: With the skin taut, the mold is positioned over points B and B for demarcation of the two flaps; F: Front view of the marking.
The AC distance is measured after elevation of point C in its proper position. This distance is transferred to lines AB and AB', adding 3 to 4 cm as safety. Then, with the skin stretched, the mold is positioned above points B and B', with the portion referring to the new navel facing upward, to make the demarcation of the two flaps (Figure 3). These flaps should be approximately 10 cm from points B and B'. Small changes can be made up or down depending on the patient's biotype, that is, down in short patients and up in slender ones.
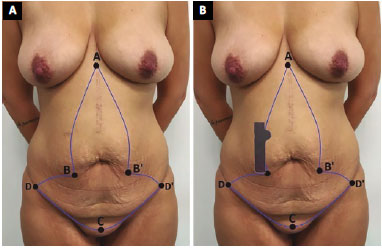
Figure 3. Marking scheme. A: Point A, upper vertex of the skin surplus; points B and B', base of the vertical cutaneous excess; point C, 5 cm from the vaginal wishbone or penis base; points D and D', lateral ends; B: The mold is positioned above points B and B' for demarcation of the two flaps of the neo-omphaloplasty.
Surgical technique
Abdominal dermolipectomy begins after general or epidural anesthesia, antibiotic prophylaxis, asepsis, and antisepsis with detergent and alcoholic chlorhexidine. Incision is performed with a scalpel on the previous marking. Monobloc exeresis of all demarcated areas with electrocautery in the supra-aponeurotic plane detachment, including the navel and its pedicle, is performed in the cranial to caudal direction.
These are followed by repositioning of the rectus abdominis muscles by plication of the anterior aponeurosis with polypropylene yarn No. 0 (Prolene®), after synthesis of the umbilical scar with the same yarn. The skin and fat flaps are approximated in the median and crossline, and suture begins, including the fascia of Scarpa of both flaps attached to the aponeurosis to avoid dead space (adhesion points).
Neo-omphaloplasty follows, in which the flaps are fixed to each other in the midline by using a 2-0 nylon yarn, with two subdermal points parallel to the aponeurosis of the rectus abdominis muscle (Figure 4). Next, the fatty tissue is approximated around the new umbilical scar with points with polyglactin 1-0 (Vicryl®). With poliglecaprone 4-0 (Monocryl®), subdermal and, lastly, intradermal points are held with the same yarn.
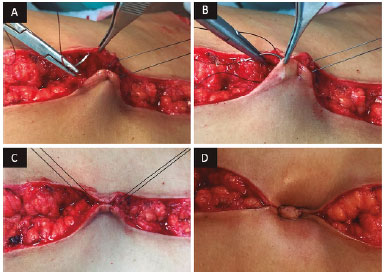
Figure 4. Neo-omphaloplasty. The flaps are fixed to each other in the midline by using nylon thread 2-0, with two parallel subdermal points to the aponeurosis of the rectus abdominis muscle.
RESULTS
Between April 2015 and December 2016, 50 patients underwent anchor-line abdominoplasty with neo-omphaloplasty using a mold in the preoperative marking. Forty-eight patients (96%) were female and two (4%) were male. The patients' ages ranged from 25 to 67 years, with a mean of 40.5 years, with a higher prevalence in the fourth and fifth decades of life.
In the 50 patients, gastroplasty was performed via laparotomy in 41 patients (82%) and via videolaparoscopy in 9 (18%). Gastric bypass (FobiCapella surgery14) was performed in all the patients. The time interval between gastroplasty and abdominal dermolipectomy ranged from 1 year 3 months to 5 years 4 months, with a mean interval of 2 years 3 months.
The BMI of the patients before abdominoplasty ranged from 21.9 to 36.7 kg/m2, with a mean of 27.9 kg/m2. The weight loss ranged from 29 to 85 kg, with a mean of 48.14 kg.
Forty-eight patients (96%) were discharged from the hospital on the first postoperative day, and two patients (4%) were discharged on the second postoperative day. The time of follow-up ranged from 2 to 14 months, with a mean of 5 months.
The new navels produced from the flaps demarcated by the mold resulted in a small umbilical scar, with a more oval shape, without surrounding scars, and with adequate depth, as can be seen in Figures 5 to 8.
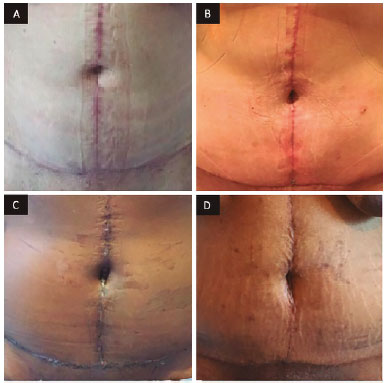
Figure 5. Front view after surgery for neo-omphaloplasty. A: Six months after surgery; B: Three months after surgery; C: Thirty days after surgery; D: Twenty-one days after surgery.

Figure 6. A: Front view before surgery; B: Front view 3 months after anchor-line abdominoplasty with neo-omphaloplasty.
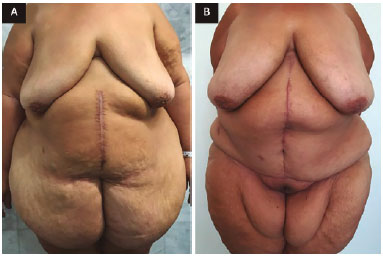
Figure 7. A: Front view before surgery; B: Front view 8 months after anchor-line abdominoplasty with neo-omphaloplasty.
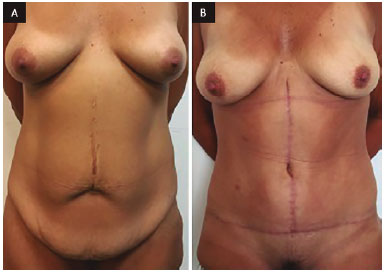
Figure 8. A: Frontal view before surgery; B: Front view 9 months after anchor-line abdominoplasty with neo-omphaloplasty.
No major complications occurred, such as pulmonary thromboembolism, deep venous thrombosis, hematoma, or necrosis. The minor complications were one case (2%) of seroma, four cases (8%) of cellulitis, six cases (12%) of hypertrophic scar, one case (2%) of keloid, five cases (10%) of small operative wound dehiscences, one case (2%) of neo-navel partial dehiscence, nine cases (18%) of neo-navel epidermolysis, and one case (2%) of granuloma (Table 1).
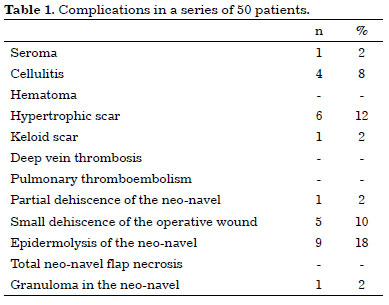
Questionnaire responses were obtained from 50 patients (Table 2). As to the new navel format, 41 patients (82%) were highly satisfied, seven (14%) were satisfied, and two (4%) were indifferent. Regarding the position, 40 patients (80%) were highly satisfied, six (12%) were satisfied, and four (8%) were indifferent. Regarding the general aspect, 41 patients (82%) were highly satisfied and nine (18%) were satisfied. None of the patients had an unfavorable evaluation regarding the criteria addressed.
DISCUSSION
Treatment of the umbilical scar is extremely important in abdominoplasty, with the navel being the main aesthetic element of the abdominal wall15. Consequently, patents desire that the umbilical scar is aesthetically pleasing after the surgical procedure.
Any kind of umbilical reconstruction aimed at attaining a good aesthetic result should consider important characteristics such as size, shape, location, and appropriate depth16. Some studies suggest several surgical techniques for umbilical reconstruction, such as the use of local flaps in different ways, sutures, and even cartilage grafts17,18.
The emergence of new ideas or technical details related to neo-omphaloplasty intends to seek better results and should be stimulated.
The parameters measured in the flaps used in the mold were based on the descriptions in literatures on the anatomy of the umbilical scar, which include depressed, surrounded by a natural skin fold that measures 1.5 to 2.0 cm in diameter19.
With the standardized measures of the flaps for neo-omphaloplasty, the mold was produced on radiography film because it is malleable, simple to reproduce, and inexpensive. A sterilizable metal mold for surgeons who prefer intraoperative demarcation was also made but not used in this study because of the author's preference for preoperative marking for the benefit of decreasing anesthesia time and surgery.
Marking the skin with small deviations may result in asymmetrical, distorted, or poorly positioned scarring. Standardization with the aid of a mold provides good symmetry and shape of the flaps with better aesthetic results, besides the reduction of surgical time. The mold can be applied to all cases of anchor-line abdominoplasty with neo-omphaloplasty. It is an effective teaching tool, as it is easy to learn and fast, has reproducible and predictable results, and involves the handling of well-vascularized flaps.
As it does not leave a circular scar, the structures are reconstructed in accordance with their natural appearance, and the result is a small and harmonious umbilical scar.
Contrary to the finding of Franco et al.20, who used a right angle in the flap base, a curvilinear transition stands out in the mold, a principle presented by Donnabella21, and leaves a less elongated and more rounded umbilical scar.
In patients with a scarce adipose panicle, adequate depth in the neo-navel is usually difficult to achieve, evolving in most cases to a shallow navel. With the approach suturing of the fatty tissue around the new umbilical scar, the aspect showed improvement with a solution to this problem21.
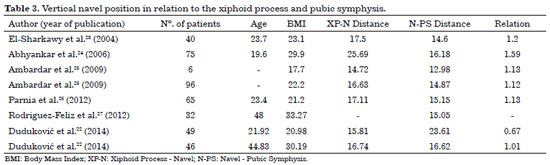
One of the drawbacks of performing neo-omphaloplasty is the difficulty in defining its position and the height of the new navel in relation to the pubis and xiphoid process. In the review of literatures, some articles measured the vertical position of the navel in the abdomen, having as reference points the xiphoid process and pubic symphysis because they are static structures.
These studies show that the position of the navel is lower than the midpoint between these structures; that is, the distance from the navel to the xiphoid process is greater than the distance between the navel and the pubic symphysis, with a ratio ranging from 1.01 to 1.59, except in the study of Duduković et al.22, who identified otherwise in groups of young women in a Croatian population, with a ratio of 0.67 (Table 3)22-27.
No consensus has been reached as to the optimal position of the umbilical scar, and such a definition should be resolved with the aesthetic sense of the surgeon. Owing to the lack of similar work in the Brazilian population and to such divergence of results found in literatures, this study used a rationalized marking of 10 cm from points B and B (measure incorporated to the mold) in medium-shape biotypes as a fast and reliable method to define the anatomical position in neo-omphaloplasty, which can be adjusted in accordance with biotype (increased for slender biotypes and decreased for shorter biotypes), generating a distance of approximately 14 to 16 cm from the symphysis pubic to the new navel.
The incidence rates of complications in abdominoplasties and specific complications in the neo-navel were low in the patients in this study. Only one case of seroma was identified, requiring puncture for drainage; no suction drain was used in this case. The cellulites were treated with amoxicillin and clavulanate acid for 7 days, with good clinical response.
In the patient who had a keloid scar, triamcinolone was applied, with six sessions in a 3-week interval, with an unsatisfactory response until the completion of the study. The incidence of epidermolysis in the neo-navel was 18%, with a higher incidence at the beginning of the study. After suturing the flaps near the aponeurosis so that the stitches were not too tight, complications were reduced. In the review of literatures, few studies were found describing the specific complications in the neo-navel; we believe that these complications are underreported28-30.
CONCLUSION
The use of the mold in the standardization of the preoperative marking in neo-omphaloplasty is effective, easy and safe to learn, low-cost, fast, and reproducible, and had low complication rates and good surgical results, with excellent patient satisfaction.
COLLABORATIONS
ACMA Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
JCRRA Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents.
AFSF Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents.
JLD Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents.
VPA Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript.
RCF Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript.
TFD Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript.
AD Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript.
REFERENCES
1. Donnabella A, Neffa L, Barros BB, Santos FP. Abdominoplastia pós-cirúrgica bariátrica: experiência de 315 casos. Rev Bras Cir Plást. 2016;31(4):510-5.
2. Ramos AC. O Brasil procurando preencher o seu espaço na cirurgia bariátrica. Arq Bras Cir Dig. 2014;27(Supl.1):1-1.
3. Sociedade Brasileira de Cirurgia Bariátrica e Metabólica. Volume de cirurgias bariátricas por ano no Brasil [acesso 2017 Jan 27]. Disponível em: http://www.sbcbm.org.br/ wordpress/imprensa-2/releases/evolucao-das-cirurgias-bariatricas-no-brasil/
4. Sociedade Brasileira de Cirurgia Plástica. Capítulo de cirurgia plástica pós-bariátrica [acesso 2017 Jan 27]. Disponível em: http://www2.cirurgiaplastica.org.br/sbcp/capitulose-comissoes/
5. Visscher TL, Seidell JC. The public health impact of obesity. Annu Rev Public Health. 2001;22:355-75. DOI: http://dx.doi.org/10.1146/annurev.publhealth.22.1.355
6. Furtado IR, Nogueira CH, Lima Júnior EM. Cirurgia plástica após a gastroplastia redutora: planejamento das cirurgias e técnicas. Rev Soc Bras Cir Plást. 2004;19(2):35-40.
7. Reno BA, Mizukami A, Calaes IL, Staut JG, Claro BM, Baroudi R, et al. Neo-onfaloplastia no decurso das abdominoplastias em ancora em pacientes pós-cirurgia bariátrica. Rev Bras Cir Plást. 2013;28(1):114-8. DOI: http://dx.doi.org/10.1590/S1983-51752013000100019
8. Regnautl P. The history of abdominal dermolipectomy. Aesthetic Plast Surg. 1978;2(1):113-23. DOI: http://dx.doi.org/10.1007/BF01577945
9. Bozola AR, Bozola AC. Abdominoplastia. In: Mélega JM, Baroud R, eds. Cirurgia Plástica Fundamentos e Arte: Cirurgia Estética. Rio de Janeiro: Medsi; 2003. p. 609-23.
10. Pfulg M, Van de Sijpe K, Blondeel P. A simple new technique for neo-umbilicoplasty. Br J Plast Surg. 2005;58(5):688-91. DOI: http://dx.doi.org/10.1016/j.bjps.2005.01.013
11. Franco T, Franco D. Neoomphaloplasty: An old and new technique. Aesthetic Plast Surg. 1999;23(2):151-4. DOI: http://dx.doi.org/10.1007/s002669900260
12. Dogan T. Umbilicoplasty in abdominoplasty: a new approach. Ann Plast Surg. 2010;64(6):718-21. PMID: 20407366 DOI: http://dx.doi.org/10.1097/SAP.0b013e3181b02210
13. Lee MJ, Mustoe TA. Simplified technique for creating a youthful umbilicus in abdominoplasty. Plast Reconstr Surg. 2002;109(6):2136-40. DOI: http://dx.doi.org/10.1097/00006534-200205000-00054
14. Capella RF, Capella JF, Mandec H, Nath P. Vertical Banded Gastroplasty-Gastric Bypass: preliminary report. Obes Surg. 1991;1(4):389-95. DOI: http://dx.doi.org/10.1381/096089291765560782
15. Lee SJ, Garg S, Lee HP. Computer-Aided Analysis of the "Beautiful" Umbilicus. Aesthet Surg J. 2014;34(5):748-56. DOI: http://dx.doi.org/10.1177/1090820X14533565
16. Joseph WJ, Sinno S, Brownstone ND, Mirrer J, Thanik VD. Creating the Perfect Umbilicus: A Systematic Review of Recent Literature. Aesthetic Plast Surg. 2016;40(3):372-9. DOI: http://dx.doi.org/10.1007/s00266-016-0633-x
17. Matsuo K, Kondoh S, Hirose T. A simple technique for reconstruction of the umbilicus, using a conchal cartilage composite graft. Plast Reconstr Surg. 1990;86(1):149-51. DOI: http://dx.doi.org/10.1097/00006534-199007000-00026
18. Marconi F. Reconstruction of the umbilicus: a simple technique. Plast Reconstr Surg. 1995;95(6):1115-7. DOI: http://dx.doi.org/10.1097/00006534-199505000-00028
19. Craig SB, Faller MS, Puckett CL. In search of the ideal female umbilicus. Plast Reconstr Surg. 2000;105(1):389-92. PMID: 10627008 DOI: http://dx.doi.org/10.1097/00006534-200001000-00062
20. Franco D, Medeiros J, Farias C, Franco T. Umbilical reconstruction for patients with a midline scar. Aesthetic Plast Surg. 2006;30(5):595-8. DOI: http://dx.doi.org/10.1007/s00266-006-0114-8
21. Donnabella A. Reconstrução anatômica da cicatriz umbilical. Rev Bras Cir Plást. 2013;28(1):119-23. DOI: http://dx.doi.org/10.1590/S1983-51752013000100020
22. Dudukovic M, Kisic H, Baez ML, Bulic K, Veir Z, Cvjetičanin B, et al. Anatomical Prediction for Surgical Positioning of the Umbilicus in a Croatian Population. Ann Plast Surg. 2015;75(2):135-9. DOI: http://dx.doi.org/10.1097/SAP.0000000000000012
23. El-Sharkawy AG, Said TA, Shafik IA, Khalifa HA. A study of the aesthetic patterns of the umbilicus among Egyptians with a new technique for umbilical reconstruction de novo. Kasr El-Aini J Surg. 2004;5(3):87-99.
24. Abhyankar SV, Rajguru AG, Patil PA. Anatomical localization of the umbilicus: an Indian study. Plast Reconstr Surg. 2006;117(4):1153-7. PMID: 16582780 DOI: http://dx.doi.org/10.1097/01.prs.0000204793.70787.42
25. Ambardar S, Cabot J, Cekic V, Baxter K, Arnell TD, Forde KA, et al. Abdominal wall dimensions and umbilical position vary widely with BMI and should be taken into account when choosing port locations. Surg Endosc. 2009;23(9):1995-2000. DOI: http://dx.doi.org/10.1007/s00464-008-9965-1
26. Parnia R, Ghorbani L, Sepehrvand N, Hatami S, Bazargan-Hejazi S. Determining anatomical position of the umbilicus in Iranian girls, and providing quantitative indices and formula to determine neo-umbilicus during abdominoplasty. Indian J Plast Surg. 2012;45(1):94-6. DOI: http://dx.doi.org/10.4103/0970-0358.96594
27. Rodriguez-Feliz JR, Makhijani S, Przybyla A, Hill D, Chao J. Intraoperative assessment of the umbilicopubic distance: a reliable anatomic landmark for transposition of the umbilicus. Aesthetic Plast Surg. 2012;36(1):8-17. DOI: http://dx.doi.org/10.1007/s00266-011-9748-2
28. Lievain L, Aktouf A, Auquit-Auckbur I, Coquerel-Beghin D, Scotte M, Milliez PY. Abdominoplasty complications: particularities of the post-bariatric patients within a 238 patients series. Ann Chir Plast Esthet. 2015;60(1):26-34. PMID: 25245542 DOI: http://dx.doi.org/10.1016/j.anplas.2014.08.013
29. Fischer JP, Wes AM, Serletti JM, Kovach SJ. Complications in body contouring procedures: an analysis of 1797 patients from the 2005 to 2010 American College of Surgeons National Surgical Quality Improvement Program databases. Plast Reconstr Surg. 2013;132(6):1411-20. PMID: 24005367 DOI: http://dx.doi.org/10.1097/PRS.0b013e3182a806b3
30. Cavalcanti ELF. Neoumbilicoplastia como opção de reconstrução umbilical nas dermolipectomias abdominais em âncora pós-gastroplastia. Rev Bras Cir Plást. 2010;25(3):509-18. DOI: http://dx.doi.org/10.1590/S1983-51752010000300019
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Felício Rocho, Belo Horizonte, MG, Brazil
3. Instituto de Cirurgia Plástica Avançada, Belo Horizonte, MG, Brazil
4. Hospital e Maternidade Therezinha de Jesus, Juiz de Fora, MG, Brazil
5. Hospital Monte Sinai, Juiz de Fora, MG, Brazil
6. Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brazil
7. Faculdade de Medicina da Universidade de Itaúna, Itaúna, MG, Brazil
8. Hospital da Plástica, Rio de Janeiro, RJ, Brazil
Institution: Hospital Felício Rocho, Belo Horizonte, MG, Brasil; Hospital e Maternidade Therezinha de Jesus e Hospital Monte Sinai, Juiz de Fora, MG, Brazil.
Corresponding author:
Augusto César de Melo Almeida
Rua Erê, 23 - 1205 - Prado
Belo Horizonte, MG, Brazil - Zip Code 30411-052
E-mail: contato@draugustoalmeida.com.br
Article received: April 5, 2017.
Article accepted: July 9, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter