

Original Article - Year 2017 - Volume 32 -
Revisiting Postbariatric Monsplasty
Revisitando a puboplastia pós-bariátrica
ABSTRACT
INTRODUCTION: The treatment of the pubic region is an integral part of lower body readjustment in post-bariatric patients, considering the pathophysiology and generalized characteristics of contour deformities after a considerable weight loss. The objective is to present our experience in the treatment of post-bariatric patients, exclusively by low marking of abdominoplasty with appropriate tissue mobilization vectors, without the necessity to leave vertical or oblique scars in the pubic region.
METHODS: The medical and photographic records of patients subjected to different abdominal approaches were retrospectively evaluated, applying the principles described above in the combined treatment of the pubic region. A low anterior skin incision was created, and angled cranial detachment towards the aponeurotic plane (with the bevel preserving the deep upper fat) and maintenance of excess fat on the upper edges to facilitate the fixation of the flaps through the superficial fascial system were performed. The outcomes' quality was subjectively evaluated by a single observer.
RESULTS: In the case series of 126 consecutive patients, the strategy used restored the best position, tone, and shape of the pubis in 100% of the cases; the results were subjectively classified as good (40%) or very good (60%). The complications more frequently found in the post-operative period were small suture dehiscence (23.8%) and seroma formation (19%), with good evolution provided by dressings and serial punctures.
CONCLUSION: The surgical strategy presented involving low positioning of the anterior incision and flap alignment in the superficial fascial system and skin by fixation allows the proper treatment of the pubic region during post-bariatric abdominoplasty procedures, without the need for additional resections and scars.
Keywords: Surgical reconstructive procedures; Bariatric surgery; Morbid obesity; Changes in body weight; Pubic symphysis.
RESUMO
INTRODUÇÃO: O tratamento da região pubiana é parte integrante do reajuste corporal inferior nos pacientes pós-bariátricos, tendo em vista a fisiopatologia e o caráter generalizado das deformidades de contorno após grandes emagrecimentos. O objetivo é apresentar nossa experiência no tratamento de pacientes pós-bariátricos, exclusivamente pela marcação baixa da abdominoplastia com vetores adequados de mobilização tecidual, sem a necessidade de cicatrizes verticais ou oblíquas na região do púbis.
MÉTODOS: Foram avaliados retrospectivamente prontuários médicos e registros fotográficos de pacientes submetidos a diferentes abordagens abdominais, com aplicação dos princípios descritos acima no tratamento associado da região pubiana. Incisão cutânea anterior baixa, descolamento cranial angulado em direção ao plano aponeurótico (bisel preservando gordura profunda superior), e manutenção um excedente gorduroso nos bordos superiores para a facilitar a fixação dos retalhos através do Sistema Fascial Superficial. Uma avaliação subjetiva da qualidade dos resultados foi caracterizada por observador único.
RESULTADOS: Numa casuística de 126 pacientes consecutivos, a tática empregada possibilitou restabelecer a melhor posição, tônus e formato do púbis em 100% dos casos, cujos resultados foram subjetivamente classificados como bom (40%) ou ótimo (60%). As intercorrências mais frequentemente encontradas na evolução pós-operatória foram pequenas deiscências da sutura (23,8%) e seromas (19%), com boa evolução pelos curativos e punções seriadas.
CONCLUSÃO: A tática cirúrgica apresentada, com posicionamento baixo da incisão anterior e aproximação dos retalhos por fixação no sistema fascial superficial e pele, possibilita o tratamento adequado da região pubiana durante as abdominoplastias pós-bariátricas, sem a necessidade de ressecções e cicatrizes adicionais.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Cirurgia bariátrica; Obesidade mórbida; Alterações do peso corporal; Sínfise pubiana.
The new understanding of the body contour physiopathology in considerable weight losses requires specialists to consider specifically tissue anatomical changes and biodynamics to improve the diagnosis and surgical planning in post-bariatric patients. Therefore, it is necessary to change some of the paradigms acquired in the treatment of classic diseases that usually result from pregnancies, aging, and mild to moderate weight changes.
As a fundamental concept, obesity followed by a considerable weight loss causes extensive deformities in all body parts that require a broader approach owing to the proximity of all tissues involved. Therefore, it is important to treat not only single structures, but also all affected body segments, including those of the pubic area. Very different from those of most conventional patients, the morphological changes are not anatomically restricted to the anterior abdominal wall, but are closely related to the lateral and posterior aspects of the lower body, including the pubis, flanks, proximal thigh roots, and buttocks.
It is precisely in the subcutaneous tissues that these changes are more intense and spread with a generalized pattern. Thus, it is the responsibility of the surgeon to guide and discuss with patients all aspects that need to be corrected in detail, while explaining the variables of the different approaches, as well as the possible outcomes and limitations.
In the early 1990s, Lockwood1 published new concepts that provided a better and more complete understanding of the entire three-dimensional structure of the connective tissue between the dermis and the muscle. These aim at establishing and popularizing the so-called superficial fascial system (SFS) with the specific supportive function of the skin and body fat (Figure 1A). The large fat accumulation in the adipocytes of patients with obesity produces a mechanical effect relying on the generalized stretching of the SFS fibers owing to the volumetric expansion of the entire subcutaneous space (Figure 1B).
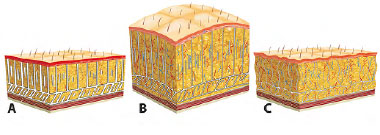
Figure 1. A: Normal tissue: SFS showing subcutaneous collagenous fibers in balance with the skin and fat; B: Obesity: Increased adipocytes promoting skin and SFS distension; C: Weight loss: Subcutaneous emptying with structural imbalance of the SFS and subsequent tissue laxity. SFS: Superficial Fascial System.
Conversely, subsequent weight loss leads to a massive emptying of these adipocytes, reducing the volume of the subcutaneous tissues without causing the retraction of collagen fibers that remain elongated and thin. This characterizes the SFS failure, which causes a great tissue laxity, a hallmark characteristic of these patients (Figure 1C). Figure 1 shows the schematic representation of the pathophysiological mechanism involved in the tissue trophism of patients with major weight loss2.
In summary, the trophism of the subcutaneous tissues in post-bariatric patients is the key for a better understanding of deformities following considerable weight loss as well as their treatment. Paradoxically, while the skin is hypotrophic and not elastic, the entire body coverage shows a dramatic laxity due to the SFS failure in cases of aggravated tissue distension.
The effect of gravity on the weight of these tissues and the limiting of the areas of adherence to deeper plans will determine the general pattern of body contour deformities. The experience of the surgeons should guide them in understanding these deformities, not only by the appearance of certain structures observed when the patients are placed in the orthostatic position, but also mainly by the actual causes of this biodynamic behavior, which should be addressed through an efficient planning.
The pubic region should be evaluated along with the entire lower body. Its treatment would be more efficient if the surgical plan takes into account the need for a combined approach with the anterior abdomen, precisely owing to the proximity of the tissues that form an inseparable anatomic unit.
Attempts to approach the abdomen without including the pubis in the planning usually cause disharmonious results owing to the inadequacy of the tissues, which would result in tissue segments that are closely interconnected. Similarly, approaches for the correction or isolated adequacy of the pubis generally require more invasive maneuvers that cause more scars and reduce the naturalness of the results.
Figure 2 shows some patterns of contour deviation from the pubic region in a post-bariatric patient and points out the need to evaluate the entire body segment for a planning that would promote harmony with the adjacent tissues, including the abdomen and the thigh root.

Figure 2. Examples of the pubic region in patients who lost weight, with different levels of sagging and tissue redundancy.
OBJECTIVE
The objective of this study is to present our experience in the treatment of the pubic region of post-bariatric patients, exclusively by proper planning of resections and respective tissue mobilization vectors during lower body readjustment.
METHODS
We retrospectively analyzed the medical and photographic records of post-bariatric patients presenting surgical evolution after being submitted to lower body readjustment between January 2013 and August 2016. The patients were attended to in the outpatient clinic of the Hospital das Clínicas of the Botucatu Medical School and the private clinic of the first author.
The selection criteria included as follows: history of bariatric surgery; great tissue laxity and different levels of pubic region involvement; stabilization of weight loss (weight variation of less than 3% in a period of 3 months); maximum body mass index of 30 kg/m2; and at least 18 months of post-operative date (gastric bypass surgery).
The patients received all information relating to the procedures that were submitted, including possible outcomes and limitations, which were duly reported and documented in the Informed Consent Form. In both phases of medical intervention and data collection, the principles established by the Declaration of Helsinki and their updates were observed.
Pre-operative marking
As a fundamental rule in the interventions performed, regardless of the approach indicated for lower body readjustment (anterior transverse - conventional; anterior composite - anchor; circumferential or circumferential composite), the correction of the pubic region was performed exclusively by low marking and suspension of the lower flap, without any additional cutaneous resection, either in the vertical or oblique direction of the pubic triangle. The pre-operative manual traction of the region simulated the result to be obtained, including the position of the final low scar (Figure 3).

Figure 3. Palpation of the pubic region in a post-bariatric patient showing the correction vector with the reduction and suspension of the ptosed tissue.
Regardless of the intensity of pubic sagging and ptosis, the patients were initially placed in the horizontal dorsal decubitus position so that in the presence of vigorous cranial traction of all pubis, a first horizontal line of approximately 14 cm was then marked, with its central point 5 cm away from the vulvar rhyme (hairy) after marking the anterior midline. The new upper skin edge of the pubic region was subsequently determined. This maneuver is fundamental because it determines the so-called cutaneous anchor line, that is, the final position of the anterior horizontal scar after aligning the flaps (Figure 4).

Figure 4. Patient in the horizontal dorsal decubitus position and upper pubic traction maneuvers for low horizontal marking 5 cm away from the vulvar rhyme.
From this initial delimitation, the patients were placed in the standing position, and the marking followed the needs and individual indications, with the planning of tissue resections in the anterior or circumferential plane, with or without a vertical component (anchor). The specific manual clamping maneuvers with tissue mobilization defined the pattern of surgical marking by always determining the anchor line, that is, the desired final position of the scars by moving the more fixed flaps' edges as opposed to the more mobile flaps (Figure 5).
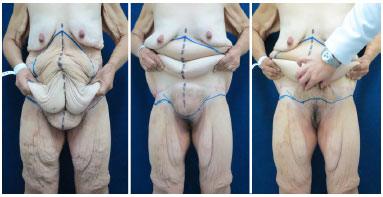
Figure 5. Similar patient in the standing position showing the marking performed for the circumferential lower body composite approach, with special emphasis on the low positioning of the horizontal incision, below the level of the pubis 5 cm away from the vulvar rhyme.
Surgical technique
The strategies related to the pubic area regardless of the specific maneuvers performed in the implementation of various techniques for lower body adjustment were covered. Since the edges to be approximated usually undergo a great mobilization to reach their new position, especially in the anchor approaches, where there is little or no detachment, there is a risk that the "inverted T-shape" region will have little subcutaneous tissue, thus causing excessive tension and local depression. To prevent this occurrence, we included two specific actions in the production of these flaps.
In the lower flap, the upper fatty detachment toward the aponeurotic plane should be conducted by making a large bevel in the cranial direction, that is, with an angle that would allow conservation of a good amount of deep fat in the upper pubic region after the cutaneous incision. Thus, in addition to preserving the lymphatic circulation at this level when the skin at the base of the pubic triangle migrates toward the abdominal flap, it slides over a fatty cushion that protects against a possible localized depression. Moreover, in the production of the upper flaps, an extra fatty component was also preserved in the corresponding central region for the same purpose (Figure 6A).
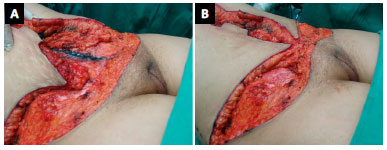
Figure 6. A: Strategic detail of the cranially angled lower detachment and fatty component at the edge of the upper flaps; B: Flap approximation in the anterior composite approach (anchor).
The central approximation of the flaps was performed initially by deeper sutures at the level of the SFS using simple mononylon 3.0 sutures, followed by subdermal sutures using colorless mononylon 4.0 and intradermal finishing sutures using monochryl 3.0 threads. It should be noted that because of the bevel made in the upper region of the inverted triangle, we did not perform the aponeurotic fixation of the flaps, but only the union of the subcutaneous tissue with deep sutures, since interesting the SFS (Figure 6B).
Such sutures followed laterally, distributing the tissues and reducing the tension for the closure of the skin. The final anchorage of the approximate flaps was determined by the migration and blocking of the cutaneous plane, according to the planning explained during previous appointments (Figure 7).
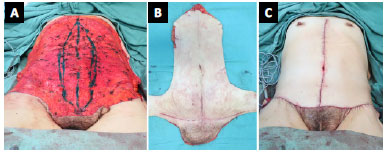
Figure 7. Intraoperative circumferential composite approach of the lower body. A: Resected anterior tissue, with a low incision at the level of the pubis; B: Surgical piece showing the pubic tissue resected in continuity with the abdomen; C: Final aspect after the sutures with the redefinition of the pubic region.
At the end of flap approximation, if there were excess fatty tissues in the pubic cone already reduced by the low horizontal incision, we moved the hand that performed the lipectomy to the scissors in a more superficial plane without liposuction or additional skin resection. We did not recommend resections of the deep fat at this level, since they tend to predispose to lymphatic complications, especially with the formation of prolonged edema and seromas in the post-operative period.
Post-operative evaluation
With the information supported by the clinical follow-up, collection of the medical records, and comparison of the pre- and post-operative photographs, a subjective classification was performed by the first author, attempting to classify the results obtained specifically in the pubic region as "Poor," "Fair," "Good," or "Very good." As criteria to be identified in this evaluation, we highlight the position (suspension), shape, and tissue tone of the pubic cone, besides possible unesthetic scars or distortions.
RESULTS
We evaluated 126 post-bariatric patients submitted to lower body readjustment in their different modalities; of these, three underwent such via the anterior transverse approach (conventional - 2.4%), 12 via the simple circumferential approach (9.6%), 42 via the circumferential composite approach (circumferential anchor - 33.3%), and 69 via the anterior composite approach (anchor - 54.7%). All cases were marked and operated with the participation of the first author, following this method when approaching the pubic area.
Females prevail in these cohorts, with 113 patients (89.7%) and 13 (10.3%) males. Intravenous general anesthesia was used in 55 patients (43.7%), spinal block in 45 (35.7%), and a combination of the two techniques in 26 (20.6%). Suction drains were placed in all cases and maintained for 5 to 10 days, until the daily flow rate was below 40 mL.
The adverse event that was more frequently found in the post-operative period was small suture dehiscence (30 cases - 23.8%), which was exclusively treated with fibrinolytic ointment dressings. The occurrence of seromas was identified in 24 cases (19%), and the treatment included serial punctures or spontaneous drainage with absorbent dressings.
Two patients developed large abdominal hematomas (1.5%) caused by the previous composite approach (anchor), which were treated with surgical re-intervention to proceed with surgical emptying while still in the immediate post-operative period. In the present study, no cases of tissue necrosis and cardiovascular or thromboembolic phenomena were observed.
The method allowed planning of the treatment of the pubis in 100% of the cases, correcting ptosis, laxity, and tissue excess only by the low anterior incision, with readjustment of the dimensions and texture of the pubic cone, without vertical or oblique resections at this level.

Figure 8. Lower body readjustment: Pre- and post-operative images of the composite circumferential approach (12 months) plus internal reduction of the thighs (6 months).

Figure 9. Lower body adjustment: Final aspect showing the harmonious redefinition of the pubis in detail.
The quality evaluation of the post-operative results, specifically with regards to the evolution of the pubic region, was performed by a single observer and the subjective classification of operated cases. With the surgical evolution time varying between 4 and 44 months, the results of 50 and 76 patients were classified as "Good" (40%) and "Very good" (60%), respectively. No result was recorded as "Poor" or "Fair." Although with the subjective criteria, these evaluations recorded the unequivocal improvement of the pubic area in all patients, in relation to the position, natural tissue tone, and format without the stigma of unesthetic and deforming scars.
Figures 8 and 9 show the results of the treatment for body contour in the patient that was previously presented in the planning as illustrated in Figures 6 and 7. This was a severe case with an extreme degree of tissue laxity after considerable weight loss. The patient was subjected to lower body readjustment via the composite circumferential approach plus inner thigh reduction in a second operative time.
It is worth noting that despite the severity of the installed deformities, it was possible to achieve a harmonious aspect of the pubis in the middle of the abdomen, flanks, and thighs, without the need to create unesthetic scars in the body contour. It was not necessary to perform lateral resections surrounding the pubis; however, continuing with the abdominal and thigh resections, which avoided "framing" the pubis and causing an unsightly appearance with undesirable stigma, was needed.
DISCUSSION
The pubic region is a part of the lower body and deserves a special attention in surgical planning, since it constitutes a fundamental element for the esthetic balance of that segment. As with the navel, no result can be considered ideal if the pubic region is not balanced with the new abdominal contour. In general, obesity followed by a considerable weight loss significantly affects the mons pubis. This is usually redundant and ptosed in post-bariatric patients.
Among the approaches for the treatment of excess dermo-fat at this level, the literature presents some forms of tissue resection both horizontally and vertically, through medial scars, side scars, or both3-14. We consider the scars surrounding the pubis with the treatment of the thighs in continuity with the horizontal scar of the abdomen as extremely stigmatizing and unesthetic.
Medial vertical incisions can be hidden by the hair; however, we still prefer to avoid using them, since it is possible to dry large amounts of skin and fat from this region only by the low positioning of the anterior abdominal horizontal incision, which allows repositioning of the ptosed tissue, as well as restoring of the triangular shape of the mons pubis, as shown in this study.
Our treatment philosophy was derived from the work presented by Aly3 and Kaluf4, who already advocated a low incision in abdominoplasty procedures in combination with the pubic lift. The normal pubic area is shaped like an inverted triangle, and after a major weight loss, excess tissues are located on the highest portion corresponding to the base of this triangle, which is stretched during obesity in continuity with the abdominal tissue.
Thus, if we keep the low horizontal skin incision 5 cm away from the vulvar commissure, the entire contingent of the excess tissues should be removed along with the surgical piece. This would leave a new inverted triangle, which would be quite reduced and whose base can be distributed and adjusted to the superior flap without the need for vertical resections. Regardless of the approach used, i.e., abdominal, anterior transverse (conventional), anterior composite (anchor), circumferential, or circumferential composite, it will be possible to include the pubic region in the surgical planning of the lower body.
As initially suggested by Aly3, we consider it essential to perform this inferior marking at the level of the pubis, with the patients in the horizontal dorsal position, since gravity facilitates the accomplishment of the upper traction maneuver, aiding in better distribution of tissues, with greater efficiency and uniformity. From this lower initial delimitation, we continued marking the patients in the orthostatic position, according to the previous planning of the resection (anchor, circumferential, etc.).
Based on the pre-operative observations, it is noted that most of the excess pubic tissues are above this marking and will be eliminated along with the abdominal tissue that is a part of the surgical piece. This can be observed clearly in Figure 7B. The intense structural disorder of the SFS allows for large dermo-adipose resections, with the possibility of primary closure only by approaching the flaps, without any detachment beyond the incised edges. With great viability and circulatory safety, this tissue redistribution corrects excesses and repositions structures with a greater contour harmony (Figures 7A-C).
Abdominal approaches that do not include the correction of the pubis usually result in a flaccid and ptosed aspect, in disharmony with the new contour obtained in the abdomen. Similarly, possible attempts of isolated treatment of the pubic region will require more scars, with an unnatural aspect of the segment. Even in cases with an apparently less severe deformity, the pathophysiology of tissue laxity after a considerable weight loss requires the recommendation of the treatment of and planning for the pubic region along with the lower body to obtain more harmonious contour results. Figures 10-13 present two more examples illustrating the final outcome of this approach in different types of post-bariatric patients.
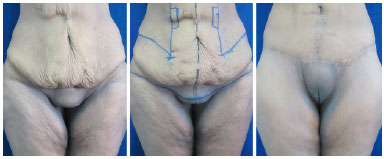
Figure 10. Lower body readjustment - frontal view. Pre-operative image, marking, and post-operative image of the composite circumferential approach (15 months) with emphasis on the harmonious redefinition of the pubic region.

Figure 11. Lower body readjustment - left lateral view. Pre-operative image, marking, and post-operative image of the composite circumferential approach (15 months) with emphasis on the harmonious redefinition of the pubic region.

Figure 12. Lower body readjustment - left lateral view. Pre-operative image, marking, and post-operative image of the composite circumferential approach (18 months) with emphasis on the harmonious redefinition of the pubic region.
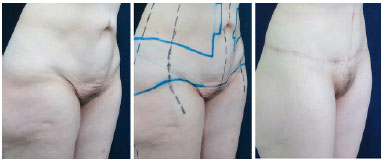
Figure 13. Lower body readjustment - right lateral view. Pre-operative image, marking, and post-operative image of the composite circumferential approach (18 months) with emphasis on the harmonious redefinition of the pubic region.
Although poorly observed in our series, small suture dehiscence and formation of localized seromas are the main complications found in performing this approach, with the treatment being generally conservative for dressings and punctures, respectively. Other possible complications described in the specialized literature divided into minor and major adverse events can be related to post-bariatric patients in general15; however, there is no evidence of a direct causal relationship with the specific approach of the pubic region.
The production and approximation of fatty flaps in the lower central region, which corresponds to the upper limit of the new pubis, seem to be an important strategy to ensure the optimal closure of the sutures without localized sinking due to the great concentric migration of these flaps and their fixation to the aponeurotic plane, which is recommended by some authors. The quality evaluation of the results could and should be improved in future studies with the use of more objective and prospective criteria, with the participation of both patients and independent observers.
CONCLUSION
The presented surgical strategy involving a low positioning of the anterior incision and alignment of the flaps by sutures in the SFS and skin allows the proper treatment of the pubic area in post-bariatric abdominoplasty procedures, without the need for additional resections and scars.
COLLABORATIONS
FHM Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
FV Conception and design of the study; writing the manuscript or critical review of its contents.
JMG Completion of surgeries and/or experiments.
RJC Conception and design of the study; completion of surgeries and/or experiments.
REFERENCES
1. Lockwood TE. Superficial fascial system (SFS) of the trunk and extremities: a new concept. Plast Reconstr Surg. 1991;87(6):1009-18. PMID: 2034721 DOI: http://dx.doi.org/10.1097/00006534-199106000-00001
2. Mendes FH, Viterbo F. Reajuste do corpo inferior: conceitos e filosofia de tratamento. In: Mendes FH, Viterbo F. Cirurgia Plástica Pós-Bariátrica. Rio de Janeiro: DiLivros; 2016. p. 201-65.
3. Aly AS. Belt lipectomy. In: Aly AS, ed. Body Contouring after massive weight loss. 1st ed. St Louis: Quality Medical Publishing; 2006. p. 71-145.
4. Kaluf R, Araújo GAZ, Martins DL, Campos LCB, Magalhães RC, Santos Júnior AJ. Tratamento da região pubiana na abdominoplastia de pacientes após grande perda ponderal. Rev Bras Cir Plást. 2008;23(4):302-4.
5. Loeb R. Narrowing of the mons pubis during thigh lifts. Ann Plast Surg. 1979;2(4):290-7. DOI: http://dx.doi.org/10.1097/00000637-197904000-00004
6. Matarasso A, Wallach SG. Abdominal contour surgery: treating all aesthetic units, including the mons pubis. Aesthet Surg J. 2001;21(2):111-9. DOI: http://dx.doi.org/10.1067/maj.2001.114789
7. Hurwitz DJ. Single-staged total body lift after massive weight loss. Ann Plast Surg. 2004;52(5):435-41. DOI: http://dx.doi.org/10.1097/01.sap.0000123361.14654.a5
8. Filho JM, Belerique M, Franco D, Franco T. Dermolipectomy of the pubic area associated with abdominoplasty. Aesthetic Plast Surg. 2007;31(1):12-5. DOI: http://dx.doi.org/10.1007/s00266-006-0102-z
9. Alter GJ. Management of the mons pubis and labia majora in the massive weight loss patient. Aesthet Surg J. 2009;29(5):432-42. DOI: http://dx.doi.org/10.1016/j.asj.2009.08.015
10. El-Khatib HA. Mons pubis ptosis: classification and strategy for treatment. Aesthetic Plast Surg. 2011;35(1):24-30. DOI: http://dx.doi.org/10.1007/s00266-010-9552-4
11. André FS. Abdominoplasty and pubic lifting. Rev Bras Cir Plást. 2009;24(3):345-50.
12. Marques M, Modolin M, Cintra W, Gemperli R, Ferreira MC. Monsplasty for women after massive weight loss. Aesthetic Plast Surg. 2012;36(3):511-6. DOI: http://dx.doi.org/10.1007/s00266-011-9859-9
13. Andre FS, Jacobowski B, André RSS. Lifting of the mons pubis after massive weigth loss. Rev Bras Cir Plást. 2013;28(4):627-32.
14. Tavares-Filho JM, Franco D, Franco T. Refinamentos na abordagem da região pubiana. In: Mendes FH, Viterbo F. Cirurgia Plástica Pós-Bariátrica. Rio de Janeiro: DiLivros; 2016. p. 354-65.
15. Cavalcante HA, Lima Jr, EM, Mendes FH. Eventos adversos em cirurgia plástica pós-bariátrica. In: Mendes FH, Viterbo F. Cirurgia Plástica Pós-Bariátrica. Rio de Janeiro: DiLivros; 2016. p. 719-45.
1. Clínica FHMendes, Lins, SP, Brazil
2. Faculdade de Medicina de Botucatu, Universidade Estadual Paulista, Botucatu, SP, Brazil
Institution: Faculdade de Medicina de Botucatu, Universidade Estadual Paulista, Botucatu, SP, Brazil.
Corresponding author:
Flavio Henrique Mendes
Rua Claudio Manoel da Costa, 65 - Jardim Ariano
Lins, SP, Brazil - Zip Code 16400-464
E-mail: mendesmd@fhmendes.com.br
Article received: December 4, 2016.
Article accepted: February 21, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter