

Original Article - Year 2017 - Volume 32 -
Surgical treatment of axillary hidradenitis suppurativa using a parascapular flap
Tratamento cirúrgico de hidradenite axilar supurativa com o uso do retalho paraescapular
ABSTRACT
INTRODUCTION: Hidradenitis suppurativa (HS) is a disease with a prevalence of approximately 1% in the population and is difficult to clinically treat. Through chronification, it may lead to functional limitations, especially in the axillary region.
METHODS: This study reports eight cases of axilla with chronic HS, Hurley stage III, treated with wide excision of the diseased part of the axillary region, followed by immediate reconstruction with a parascapular flap. The patients underwent surgery at the Plastic Surgery and Burns Service of the State Government Workers' Hospital of São Paulo.
RESULTS: All the treated patients had no recurrence. All the parascapular flaps remained viable, and infection of one of the flaps (12.5%) was the immediate complication. Closure of the entire donor area was performed using primary synthesis.
CONCLUSION: The treatment of chronic axillary HS, stage III, based on radical resection and reconstruction with a parascapular flap proved to be an effective alternative to locally control the disease and is a safe procedure to cover the axillary defect.
Keywords: Hidradenitis suppurativa; Axilla; Surgical flaps; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A hidradenite supurativa (HS) é uma doença com prevalência em torno de 1% na população, de difícil tratamento clínico, que em sua cronificação pode levar a limitações funcionais, principalmente na região axilar.
MÉTODOS: Este trabalho relata oito axilas com HS crônica estágio III de Hurley tratadas com exérese ampla da doença na região axilar e sua reconstrução imediata com o retalho paraescapular, operados no pelo Serviço de Cirurgia Plástica e Queimaduras do Hospital do Servidor Público Estadual de São Paulo.
RESULTADOS: Todas as axilas tratadas não tiveram recorrência da doença (100%). Todos os retalhos paraescapulares mantiveram-se viáveis (100%), sendo a infecção de um dos retalhos (12,5%) a complicação imediata. Fechamento de 100% da área doadora em síntese primária.
CONCLUSÃO: O tratamento da HS crônica axilar estágio III baseado na ressecção radical e reconstrução com retalho paraescapular mostrou-se uma opção efetiva no controle local da doença e um retalho seguro para cobertura do defeito axilar.
Palavras-chave: Hidradenite supurativa; Axila; Retalhos cirúrgicos; Procedimentos cirúrgicos reconstrutivos.
Hidradenitis suppurativa (HS), also known as acne inversa, was first described in 1839 by Alfred Velpeau, who reported an inflammation in the skin with formation of superficial abscesses in the axilla, breast, and perianal regions1. In 1854, Verneiul suggested an association between HS and sweat glands2.
HS may affect areas of the body where apocrine sweat glands exist; however, this condition is more common in the axilla skin and inguinoperineal region. It is characterized by a disorder in the terminal follicular epithelium of apocrine skin areas. This may cause follicular occlusion by comedo-like hyperkeratosis, recurrent inflammation, and mucopurulent drainage. Furthermore, chronification of the inflammation occurs, culminating in progressive scars3.
The prevalence of the disease in the general population is approximately 1%. The most common age group affected ranges from 11 to 50 years, with a ratio of 2 to 5 females to every male3. Regarding risk factors, smoking and obesity deserve highlight; when combined, they are associated with a more severe condition4. In epidemiological studies, an increase in the incidence of oral and hepatocellular cancers, as well as squamous cell carcinoma (especially in the gluteal region) in patients with chronic features has been reported5.
The chronic form of HS is clinically presented with salivary fistula, recurrent abscesses that lead to fibrosis, hypertrophic scar, and induration. In the axilla, it leads to shoulder movement limitation6.
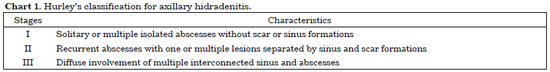
This condition may be classified into three stages according to the Hurley scale (Chart 1). Stages II and III, which are diffused diseases, are treated with radical excision and reconstruction with a flap7,8.
OBJECTIVE
To describe the surgical treatment of chronic axillary hidradenitis, stage III using a parascapular flap to reconstruct defects in the axilla.
METHODS
A retrospective study was conducted, and medical records were reviewed; thereby, four patients with chronic bilateral axillary HS were identified. They were operated in the period from January 2013 to January 2015, with failure of the previous clinical treatment, at the State Government Workers' Hospital of São Paulo (Figures 1 to 3). This study abided by the principles of the Declaration of Helsinki.
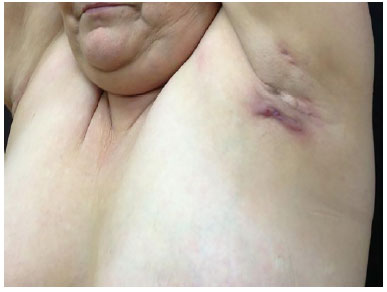
Figure 1. Preoperative profile view.
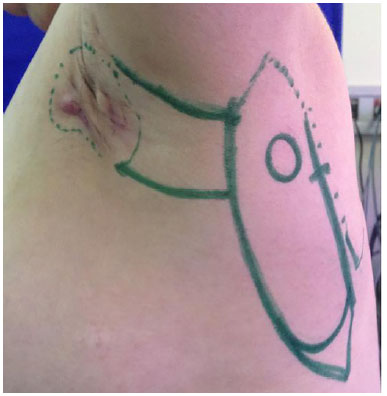
Figure 2. Planning of resection and the parascapular flap, with identification of the left triangular space.

Figure 3. Posterior view with planning of two parascapular flaps.
Surgery was performed under general anesthesia, with the patients in the lateral decubitus position, with macroscopic delimitation of the area compromised with HS, including 2 cm beyond the hairy area as the margin to be resected, limiting the deep margin to the muscle fascia. The tissues were sent for anatomopathological study and tissue culture.
Immediate reconstruction of the axilla was performed, with coverage of the skin defect with ipsilateral transposition of the parascapular flap and synthesis of the receptor axillary bed and donor area in the back with mononylon 3-0 and 4-0 in three planes. Tubular suction drains were used in the donor area and axilla of 15F, with withdrawal if flow rate was <30 ml/24 h.
After reconstruction of the axilla, the patients' position was changed to decubitus, and then the same surgical procedures were performed in the contralateral axilla.
The patients were discharged on the first postoperative day while receiving orally administered clindamycin at 1200 mg/day for 14 days, non-steroidal anti-inflammatory for 5 days, and painkillers in case of pain. In addition, the patients were followed up with weekly hospital visits in the first 2 months postoperatively, and monthly hospital visits until completion of the first postoperative year.
RESULTS
Axillary reconstruction with parascapular flap was performed in eight patients out of which four were female patients. The patients improved with local disease control, without recurrence in the follow-up period of 6 to 32 months postoperatively. One of the flaps developed infection and wound dehiscence, with a need for hospital readmissions on the 15th postoperative day, with surgical approach for cleaning and debridement of devitalized tissue, with new advances and repositioning of the flap. The culture-guided antibiotic was modified, and the patients were discharged after 3 days.
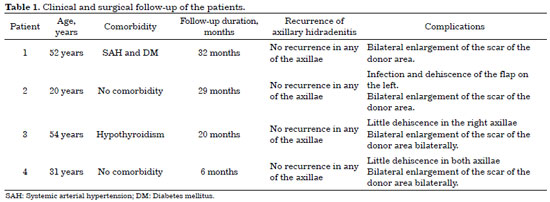
Small skin dehiscence (solution of continuity up to 5 mm of skin with exposure down to subcutaneous plane) occurred in the distal ends of three parascapular flaps, which were healed without prejudice to the result by second intention. Total loss of parascapular flap did not occur in any case. The donor areas evolved with enlargement of the scars, with a need for revision according to the patients' aesthetic complaint in all the cases (Table 1).
The patients reported an improvement in abduction of the upper limbs, with gain of amplitude and absence of axillary contracture (Figures 4 and 5).

Figure 4. Postoperative view of the coverage of the axillary defect and the donor area with the left parascapular flap.

Figure 5. Posterior view of the donor areas of the parascapular flaps, with full abduction of the upper limbs.
DISCUSSION
Mild acute HS is treated with anti-inflammatories, and topical and oral antibiotics because of secondary infection by bacteria, especially Staphylococcus aureus and coagulase-negative Staphylococcus, which may include anaerobic bacteria, Streptococcus, and gram-negative bacilli. In moderate and serious forms, beyond the measures mentioned, surgery becomes necessary to reduce morbidity and recurrence9. Weight loss and smoking cessation are important measures to decrease the severity and recurrence of the disease.
Surgical treatment is recommended in rebounding chronic HS. Hurley scale helps determine the degree of tissue resection. Regarding methods of resection for axillary disease, excisions may be locally limited to the hairy edge, or may be radical, consisting of a 2-cm margin from the hairy edge and deepening to the muscle fascia10. The axillary HS, regarding the employment of a radical resection, has a lower rate of recurrence, ranging from 0% to 3%10-12.
As for the forms of coverage of the defect in the axillary region, primary synthesis, healing by secondary intention, and skin and flap grafting are employed. The first three procedures are the most frequently used. The flaps are used for more-complex defects, with better reconstruction quality13. Grafting, despite being commonly used, is associated with high rates of infection, necrosis, and contracture14.
The flaps are classified as local, regional, and free. Among the local flaps, Limberg, propeller and transposition flaps deserve highlight. The anterolateral thigh flap is the most widely used free flap in axillary reconstruction. Nonetheless, it is associated with a trapdoor effect15. The latissimus dorsal muscle, scapular, thoracodorsal perforating artery (TDAP), and parascapular flaps are local flap alternatives.
Literature reported that the latissimus dorsi muscle flap, despite enabling primary closure of the donor area, often evolves with distal necrosis14. Moreover, it is a poor alternative for breast reconstruction. The fasciocutaneous scapular flap is thick, requiring the refinement of the thickness in the fat layer to be more adequate for the region and anterior chest region14. The TDAP flap requires a more improved dissection technique and is based on smaller-caliber vessels. Nevertheless, it is a good alternative15.
Described in 198216, the parascapular flap is a fasciocutaneous flap based on the descending branch of the circumflex scapular artery, which is a subscapular branch. It may be used as a pedicle flap or freely, as it has a safe and reliable pedicle. It is located in the lateral portion of the scapula, providing for coverage of extensive defects, and its donor area can be closed primarily. This is our choice in the reconstruction of defects with chronic axillary HS because it allows for similarities in color, texture, and skin thickness between the recipient and donor areas (Figures 6 to 8).

Figure 6. Dissected parascapular flap on the right.
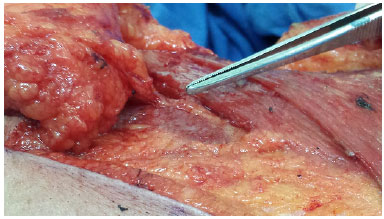
Figure 7. Identification of the pedicle in the parascapular flap (descending branch of the circumflex scapular artery) in the triangular space.

Figure 8. View of the right parascapular flap pedicle.
CONCLUSION
The treatment of chronic axillary HS, stage III, based on radical resection and reconstruction with a parascapular flap seems to be a safe and effective option. This procedure not only controls the disease locally, but also results in low morbidity of the donor area.
COLLABORATIONS
LCVTJ Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
MSLO Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
RAS Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
DNP Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
LF Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
REFERENCES
1. Balik E, Eren T, Bulut T, Büyükuncu Y, Bugra D, Yamaner S. Surgical approach to extensive hidradenitis suppurativa in the perineal/perianal and gluteal regions. World J Surg. 2009;33(3):481-7. PMID: 19067039 DOI: http://dx.doi.org/10.1007/s00268-008-9845-9
2. Ather S, Chan DS, Leaper DJ, Harding KG. Surgical treatment of hidradenitis suppurativa: case series and review of the literature. Int Wound J. 2006;3(3):159-69. DOI: http://dx.doi.org/10.1111/j.1742-481X.2006.00235.x
3. Belda Junior W, Chiacchio ND, Criado PR. Tratado de Dermatologia. São Paulo: Atheneu; 2010. p. 1144-52.
4. Sartorius K, Emtestam L, Jemec GB, Lapins J. Objective scoring of hidradenitis suppurativa reflecting the role of tobacco smoking and obesity. Br J Dermatol. 2009;161(4):831-9. PMID: 19438453 DOI: http://dx.doi.org/10.1111/j.1365-2133.2009.09198.x
5. Lapins J, Ye W, Nyrén O, Emtestam L. Incidence of cancer among patients with hidradenitis suppurativa. Arch Dermatol. 2001;137(6):730-4. PMID: 11405761
6. Parks RW, Parks TG. Pathogenesis, clinical features and management of hidradenitis suppurativa. Ann R Coll Surg Engl. 1997;79(2):83-9. PMID: 9135232
7. Menderes A, Sunay O, Vayvada H, Yilmaz M. Surgical management of hidradenitis suppurativa. Int J Med Sci. 2010;7(4):240-7. DOI: http://dx.doi.org/10.7150/ijms.7.240
8. Hurley HJ. Axillary hyperidrosis, apocrine bromhidrosis, hidradenitis suppurativa, and familial benign pemphigus: surgical approach. In: Roenigk RK, Roenigk Jr. HH, eds. Roenigk & Roenigk's Dermatologic Surgery: Principles and Practice. 2nd ed. New York: Marcel Dekker; 1996. p. 623-45.
9. Shuja F, Chan CS, Rosen T. Biologic drugs for the treatment of hidradenitis suppurativa: an evidence-based review. Dermatol Clin. 2010;28(3):511-21. DOI: http://dx.doi.org/10.1016/j.det.2010.03.012
10. Soldin MG, Tulley P, Kaplan H, Hudson DA, Grobbelaar AO. Chronic axillary hidradenitis--the efficacy of wide excision and flap coverage. Br J Plast Surg. 2000;53(5):434-6. DOI: http://dx.doi.org/10.1054/bjps.1999.3285
11. Harrison BJ, Mudge M, Hughes LE. Recurrence after surgical treatment of hidradenitis suppurativa. Br Med J (Clin Res Ed). 1987;294(6570):487-9. DOI: http://dx.doi.org/10.1136/bmj.294.6570.487
12. Nesmith RB, Merkel KL, Mast BA. Radical surgical resection combined with lymphadenectomy-directed antimicrobial therapy yielding cure of severe axillary hidradenitis. Ann Plast Surg. 2013;70(5):538-41. DOI: http://dx.doi.org/10.1097/SAP.0b013e31828ea7cb
13. Alharbi Z, Kauczok J, Pallua N. A review of wide surgical excision of hidradenitis suppurativa. BMC Dermatol. 2012;12:9. DOI: http://dx.doi.org/10.1186/1471-5945-12-9
14. Ogawa R, Hyakusoku H, Murakami M, Koike S. Reconstruction of axillary scar contractures--retrospective study of 124 cases over 25 years. Br J Plast Surg. 2003;56(2):100-5. DOI: http://dx.doi.org/10.1016/S0007-1226(03)00035-3
15. Busnardo FF, Coltro PS, Olivan MV, Busnardo AP, Ferreira MC. The thoracodorsal artery perforator flap in the treatment of axillary hidradenitis suppurativa: effect on preservation of arm abduction. Plast Reconstr Surg. 2011;128(4):949-53. PMID: 21921770 DOI: http://dx.doi.org/10.1097/PRS.0b013e3182268c38
16. Nassif TM, Vidal L, Bovet JL, Baudet J. The parascapular flap: a new cutaneous microsurgical free flap. Plast Reconstr Surg. 1982;69(4):591-600. PMID: 7071197 DOI: http://dx.doi.org/10.1097/00006534-198204000-00001
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital do Servidor Público Estadual, São Paulo, SP, Brazil
Institution: Hospital do Servidor Público Estadual, São Paulo, SP, Brazil.
Corresponding author:
Luis Carlos Vieira Tavares Júnior
Rua Pedro de Toledo, 1800 - Vila Clementino
São Paulo, SP, Brazil - Zip Code 04039-004
E-mail: lulinha_tavares@hotmail.com
Article received: April 1, 2015.
Article accepted: July 9, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter