

Original Article - Year 2017 - Volume 32 -
Vertical approach to the pectoralis major in breast implant insertion
Abordagem vertical do peitoral maior nas inclusões mamárias
ABSTRACT
INTRODUCTION: This study demonstrates an alternative method to access the retromuscular space and avoid undesirable effects caused by breast implant insertion in this space.
METHODS: We evaluated 328 female patients, aged 17 to 62 years, with complaints of micromastia and bilateral ptosis. All patients underwent insertion of bilateral implants using a vertical incision in the pectoralis major. Follow-up was performed for at least 6 months.
RESULTS: The technique of vertical incision in the pectoralis major increases the options for access to the retromuscular space in breast implant insertion. This method successfully achieves appropriate positioning of the implant and avoids additional scars.
CONCLUSIONS: The technique proved to be effective, avoiding scars and the double-bubble effect, and increases the options for access to the retromuscular space.
Keywords: Mammary implants; Prostheses and implants; Mammoplasty; Breast; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: O trabalho demonstra uma abordagem alternativa para ampliarmos a escolha do espaço retromuscular e evitarmos os efeitos indesejáveis nas inclusões de próteses mamárias neste plano.
MÉTODOS: Foram avaliados 328 pacientes do sexo feminino, com idade entre 17 e 62 anos, com queixa de hipomastia e certo grau de ptose mamária bilateral. Todas as pacientes foram submetidas à inclusão de próteses bilaterais e incisão vertical no músculo peitoral maior. A avaliação foi realizada com um período mínimo de 6 meses.
RESULTADOS: A tática cirúrgica de incisão vertical no músculo peitoral maior nos permitiu ampliar a indicação do espaço retromuscular nas cirurgias de inclusão de próteses de mamas, conseguindo alcançar com êxito o posicionamento adequado da prótese e do tecido mamário, evitando cicatrizes adicionais.
CONCLUSÕES: A técnica mostrou-se eficaz na sua propositura, evitando cicatrizes e o efeito de dupla-bolha e ampliando a indicação do espaço retromuscular.
Palavras-chave: Implantes de mama; Próteses e implantes; Mamoplastia; Mama; Procedimentos cirúrgicos reconstrutivos.
Plastic surgeons frequently encounter the need to find techniques, strategies, materials, and innovative medical therapies to achieve more satisfactory results. Although the concept of female beauty has changed over time, the shape and size of breasts remain important symbols of femininity.
Many plastic surgeons have sought innovations to achieve safer and more satisfactory results. Following the introduction of the silicone implant in 1961 by Cronin and Gerow1, augmentation mammoplasty using silicone implants has become one of the most common procedures performed by plastic surgeons in Brazil and worldwide.
Plastic surgeons have several options for breast implant insertion with regard to location and surgical procedure. Use of the retromuscular space was first described in 1967 by Griffiths2. Other authors, including Dempsey and Latham3 in 1968, Regnault4 in 1977, and Mahler et al.5 and Mahler & Hauben6 in 1982, were also pioneers in this surgery. The works of Mahler et al.5 and Mahler & Hauben6 were important in developing the technique of myotomy of the pectoralis major, a key procedure for successful retromuscular implant insertion.
Like every new plastic surgeon, 22 years ago, I began by placing retroglandular implants via an inframammary incision. Then, over time, the placement, access incision, format, and texture of the implant evolved. Like most other plastic surgeons, I followed my instincts until I decided 15 years ago that I would always place implants via inframammary and retromuscular incisions. After a succession of poor outcomes, I optimized a vertical incision in the pectoralis major and sometimes in the breast parenchyma, to ensure that the implant shape remained as close as possible to that of the breast. This was characterized as a "Modified Double Space."
Using this principle, the breast also remains as close as possible to the shape of the implant, which usually has an exaggerated high shape.
OBJECTIVE
To evaluate the effectiveness of the vertical approach through the pectoralis major in breast implant insertion over a 15-year period.
METHODS
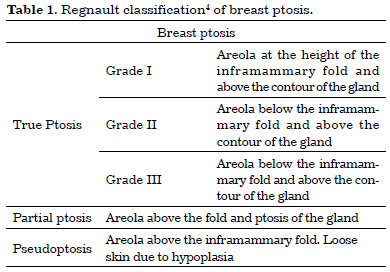
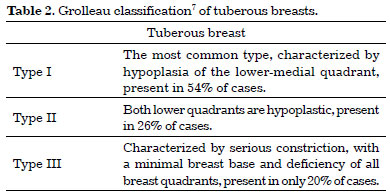
From January 2001 to January 2016, 328 patients aged 17 to 62 years underwent surgery using this approach. The retromuscular space and vertical incision in the pectoralis major were employed. Implant insertion was the only indication in 246 patients (75%), and 82 (25%) had mastopexy and implant insertion as the indication. Of the 246, 47 (19%) were performed for implant revision. The criteria for inclusion were a diagnosis of micromastia and breast ptosis (grade I, grade II, partial ptosis, or pseudoptosis) (Table 1)4. Cases of micromastia associated with grade I or grade II tuberous breasts, as described by Grolleau (Table 2)7, also were evaluated in this study.
Thus, the following characteristics were considered in determining the indication:
1 - The size and consistency of the breasts.
2 - Skin elasticity.
3 - The relationship between the breast tissue and the skin.
4 - The degree of ptosis of the nipple and inferior pole of the breast in relation to the inframammary fold.
5 - The distance between the suprasternal notch and the nipple.
Patients who met the criteria following routine preoperative examination underwent surgery under general anesthesia, without fluid supplementation. The patients in this study who complained of small breasts still had significant breast tissue, even when ptotic as described above or associated with grade I or II breast tuberosity.
The principles of Helsinki were strictly followed. Patients signed an informed consent form to permit use of their data, as well as publication of their photographs.
Surgical technique
Marking
In cases of implant insertion without mastopexy, marking was performed with the patient in standing position. A 4-cm incision was marked about 2 cm below the inframammary fold; the limits of detachment were set from the sternum to the lateral limits of muscle detachment (Figure 1). The midpoint from the nipple to the center of the inframammary incision was marked to guide the vertical incision in the pectoralis major.

Figure 1. Marking.
Surgery
Following inframammary incision and detachment of subcutaneous tissue, the lower edge of the pectoralis major was identified at the level of the sixth costal arch8, and detachment of approximately 2 cm of the rectus abdominis aponeurosis was performed inferiorly, without completely releasing the muscle (Figure 2 and 3). The pectoralis major muscle was completely detached in the medial, cranial, and lateral directions, according to the preoperative marking. We identified and preserved the lower pectoral muscle. The edge of the pectoralis major was held with two Kocher forceps, and a vertical incision of varied length was made, without exceeding the upper limit of the nipple (Figure 4 and 5). Hemostasis was confirmed and the implant was inserted (Figure 6).
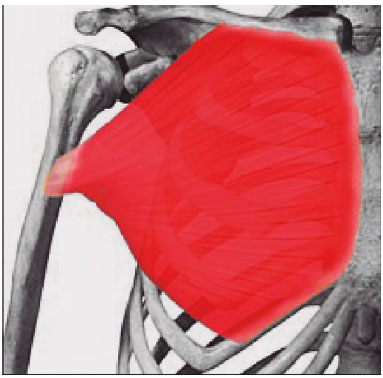
Figure 2. Route of access (Source: Reference 8).

Figure 3. Access routes.
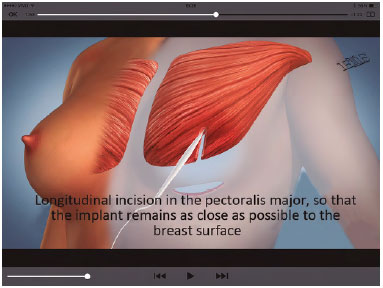
Figure 4. Vertical incision in the pectoralis major.
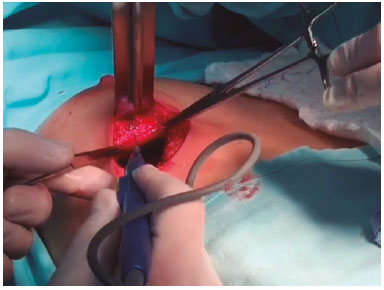
Figure 5. Vertical incision in the pectoralis major.

Figure 6. Drains were used in specific cases, and closure was performed in three planes, using continuous sutures.
Immediate postoperative management
1 - Hospital discharge on the same day in most cases. When a drain is placed, the patient is discharged after 24 hours.
2 - Dressings and a compression vest are placed for 30 days at the upper pole of the breasts (Figure 7).

Figure 7. Postoperative care.
3 -Weekly monitoring for 8 weeks, followed by monthly monitoring.
4 - Upper limb sports practice allowed after 60 days.
5 - Evaluation for possible relapse after at least 90 days.
6 - Assessment of patient satisfaction within 3 to 6 months.
RESULTS
Surgery using this approach was performed in 328 patients, with avoidance of a double-bubble effect or implant migration, and imperceptible muscle contraction in 91.9% of cases during a 2-year follow-up period (Figures 8 to 13).
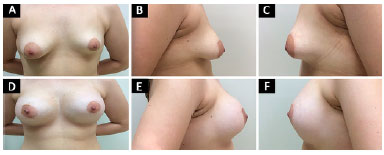
Figure 8. Case 1. A, B and C: Preoperative appearance; D, E and F: Postoperative appearance after 12 months.
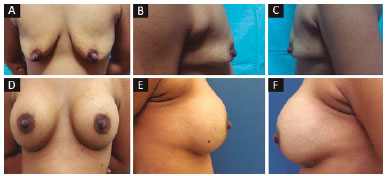
Figure 9. Case 2. A, B and C: Preoperative appearance; D, E and F: Postoperative appearance after 12 months.
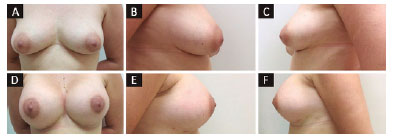
Figure 10. Case 3. A, B and C: Preoperative appearance; D, E and F: Postoperative appearance after 6 months.
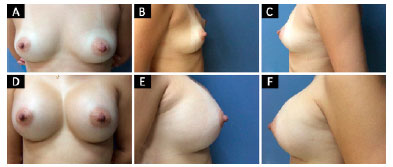
Figure 11. Case 4. A, B and C: Preoperative appearance; D, E and F: Postoperative appearance after 24 months.
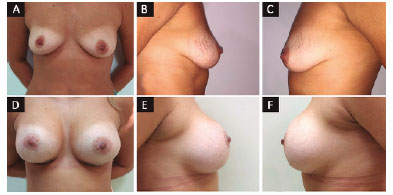
Figure 12 Case 5. A, B and C: Preoperative appearance; D, E and F: Postoperative appearance after 9 months.
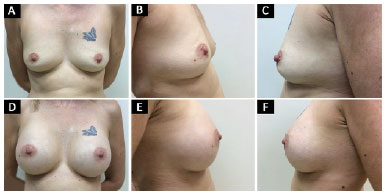
Figure 13. Case 6. A, B and C: Preoperative appearance; D, E and F: Postoperative appearance after 12 months.
Complications were inherent to the technique or specific to breast augmentation.
Complications inherent to the technique that lead to the double-bubble effect (Table 3) include:
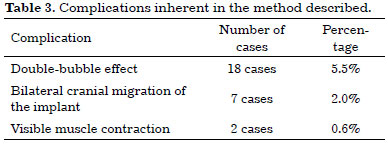
1 - Ptosis of the inferior pole of the breast.
2 - Cranial migration of the implant.
3 - Visible muscle contraction.
Reoperation was performed in 27 patients (8.3%) about 6 months postoperatively.
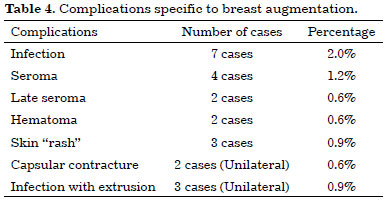
Table 4 shows the rate of complications specific to breast augmentation.
Late postoperative issues
After the first postoperative year:
§ 2 patients requested reduction of breast volume.
§ 1 requested an increase in breast volume or removal of excess skin.
After the third postoperative year:
§ 3 requested an increase in breast volume or removal of excess skin.
After the fifth postoperative year:
§ 6 requested an increase in breast volume or removal of excess skin.
§ 3 requested mastopexy.
Breast implant revision
Placement of implants in the retromuscular space sometimes results in the double-bubble effect. This is a common complication, and is a consequence of using the retromuscular space in breasts with some breast tissue, whether or not ptosis is present. These breasts were corrected with relocation of the implant in the same space, using a vertical incision in the pectoralis major, as recommended here (Figure 14).

Figure 14. Breast implant revision.
Figure 15 shows the case of a 22-year-old nulliparous patient, illustrating why most plastic surgeons remain concerned about the outcome when a retromuscular implant is placed. This patient complained of a double-bubble appearance and a "strange breast." The physical examination and imaging showed a retromuscular implant. The following treatment was proposed:
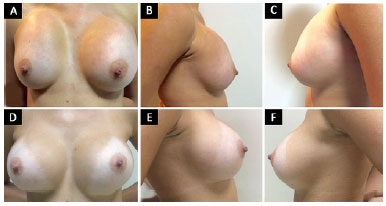
Figure 15. Breast implant revision. A, B and C: Preoperative appearance; D, E and F: Postoperative appearance after 18 months.
1 - Inferior repositioning of the implant.
2 - Retention of the implant in the retromuscular space.
3 - Vertical incision through the pectoralis major.
4 - Preservation of implant volume.
Surgery was performed with an incision in the inframammary fold and implant removal. A median vertical incision was made in the pectoralis major, and the implant was correctly placed in the retromuscular space at the inferior pole of the breast.
DISCUSSION
After extensive training, plastic surgeons naturally select techniques and materials they believe to be more effective. This choice should be based on breast anatomy and the response of the pectoral region to the presence of an implant. By studying the anatomy and vascularization of the breast, we can see that an implant in the retromuscular space provokes a less aggressive response to surrounding tissue. This harms fewer structures and avoids progression to breast atrophy that may occur with placement in the retroglandular space9.
Many surgeons and authors feel that use of the retromuscular space leads to good results, providing the implant with extra protection and ensuring surgical success. Myotomy procedures in the pectoralis major have been performed since 1982, according to Mahler & Hauben6; however, the vertical incision recommended here has not been described in the literature. The idea of using a vertical incision in the muscle stemmed from the need to create a "surgical girdle" (Figure 16 and 17) that was able to separate the upper from the lower bubble and prevent unsatisfactory results following conventional placement of a retromuscular implant.

Figure 16. Preoperative appearance and postoperative appearance at 6 months, with a double-bubble effect.
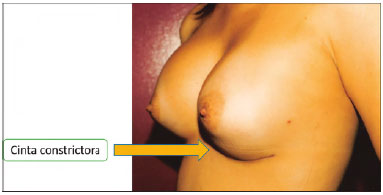
Figure 17. Presence of a surgical girdle, highlighting the double-bubble effect.
The method described was applied in 328 cases using a textured implant in a private clinic. The method proved to be highly efficient in comparison with other options (Figure 18 and 19).
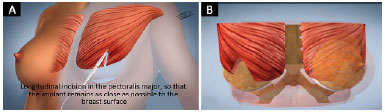
Figure 18. A: Drawing showing a vertical incision in the pectoralis major, with the aim of eliminating the surgical girdle; B: Drawing showing the incision with the implant in place.
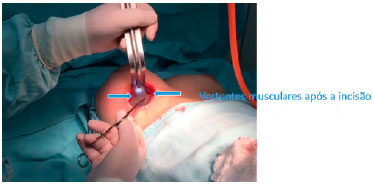
Figure 19. Implant placement after vertical incision in the pectoralis major, eliminating the surgical girdle.
Some advantages of the vertical incision are as follows:
1 - A vertical incision provides additional flexibility for positioning and symmetry in retromuscular breast implant insertion.
2 - The protection that the muscle provides for the implant minimizes the possibility of tissue weakness, as well as the risk of exposure of the implant in the inferior pole of the breast. In the upper pole, the protection provided by the intact pectoralis major avoids an effect known as rippling, in addition to providing for a more natural feel.
3 - A vertical incision decreases the amount of tissue between the implant and the breast surface, even when placed in the retromuscular space, and avoids unaesthetic effects.
4 - A vertical incision minimizes the risk of asymmetry. This incision can vary in size as needed.
5 - The retromuscular space can be used in dense breasts by making the incision in the muscle and enlarging the partition in the breast parenchyma, thus avoiding the double-bubble effect.
6 - The positioning of the implant using a vertical myotomy avoids a weighted effect in the inferior pole, avoiding early ptosis.
Comments
A case described in the literature (Figure 20)10 was treated conventionally by performing mastopexy. This case could benefit from the procedure recommended in this study, i.e., with a vertical incision in the pectoralis major, and the insertion of an implant in the retromuscular space.
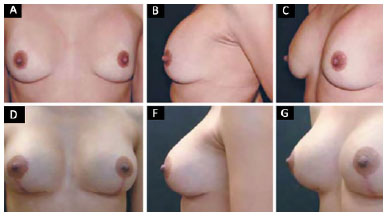
Figure 20. Literature case (Source: Reference 10).
An extensive literature search found several studies in which the pectoralis major muscle is manipulated. The authors noted the need to perform myotomy before placing a retromuscular implant9,11, but used a method unlike that recommended here; the current method achieves a better result when the retromuscular space is used. Tebbetts11 described a "Dual Plane" approach to these cases, which involved a small detachment of the lower part of the breast on the muscle, causing it to retract a little more superiorly and leaving the implant more covered by the breast to fill the inferior pole; this method was better for treatment of ptosis. Multiple other techniques were tried before we chose this approach in the pectoralis major to avoid adverse outcomes, but these were unsatisfactory.
Accordingly, we developed this technique by observing the silhouette of breasts that presented with a double-bubble effect. Daniel12 recommended a transverse incision in the pectoralis major to create a double space, with a retromuscular implant in the inferior space and a retroglandular implant in the superior space to maintain medium and long-term results.
A vertical incision in the pectoralis major enables double-space positioning of the implant in a different way, by using the advantages of the two planes and eliminating their disadvantages. Thus, we achieved a significant improvement in the results and minimized unfavorable outcomes with use of the retromuscular space.
The subfascial plane described by Graf et al.13 may present certain advantages in contrast to those of the retroglandular plane; however, this method does not completely provide the benefits offered by the retromuscular plane. In cases of a hypertrophied muscle, we can avoid a double-breast contour result14 by using the vertical approach in the pectoralis major.
Another positive feature of the retromuscular plane is the lower incidence of capsular contracture15, which is an important complication following augmentation mammoplasty. This complication is difficult to correct. Revision mammoplasty with a change in the plane associated with capsulotomy is a frequently used alternative16.
The appropriate use of the retromuscular plane could prevent many cases of capsular contracture15. Plastic surgeons should be guided by established techniques when choosing the location of an implant, while adjusting the approach as needed for each case. It is essential to have absolute mastery of the implant insertion technique in all possible planes, and internal procedures in the pectoral region should be considered as alternatives to facilitate the ongoing search for better results.
CONCLUSION
Insertion of a retromuscular implant through a vertical incision in the pectoralis major significantly decreased the risk of a double-bubble effect or cranial migration of the implant, and showed a low complication rate. Consequently, this broadened the indications for use of the retromuscular space used.
COLLABORATIONS
ELF Analysis and/or interpretation of data; statistical analyses; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
REFERENCES
1. Cronin TD, Gerow RM. Augmentation mammoplasty: a new "natural feel" prosthesis. In: Transactions of the Third International Congress of Plastic and Reconstructive Surgery. Amsterdam: Excerpta Medica; 1964.
2. Griffiths CO. The submuscular implant in augmentation mamaplasty. In: Transactions of the Fourth International Congress of Plastic Surgery. Amsterdam: Excerpta Medica; 1967. p. 1009.
3. Dempsey WC, Latham WD. Subpectoral implants in augmentation mammaplasty. Preliminary report. Plast Reconstr Surg. 1968;42(6):515-21. PMID: 5722153 DOI: http://dx.doi.org/10.1097/00006534-196812000-00001
4. Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976;3(2):193-203.
5. Mahler D, Ben-Yakar J, Hauben DJ. The retropectoral route for breast augmentation. Aesthetic Plast Surg. 1982;6(4):237-42. DOI: http://dx.doi.org/10.1007/BF01570654
6. Mahler D, Hauben DJ. Retromammary versus retropectoral breast augmentation-a comparative study. Ann Plast Surg. 1982;8(5):370-4. DOI: http://dx.doi.org/10.1097/00000637-198205000-00003
7. Grolleau JL, Lanfrey E, Lavigne B, Chavoin JP, Costagliola M. Breast base anomalies: treatment strategy for tuberous breasts, minor deformities, and asymmetry. Plast Reconstr Surg. 1999;104(7):2040-8. PMID: 11149766 DOI: http://dx.doi.org/10.1097/00006534-199912000-00014
8. Gardner E, Gray FJ, O'Rahilly R. Anatomia: estudo regional do corpo humano. 4ª ed. Rio de Janeiro: Guanabara Koogan; 1982.
9. Zeitone GC. Subpeitoral ou subglandular: qual é a melhor localização do implante para pacientes com hipomastia? Rev Bras Cir Plást. 2012;27(3):428-34.
10. Miró AL. Próteses mamárias revestidas com poliuretano: avaliação de 14 anos de experiência. Rev Bras Cir Plást. 2009;24(3):296-303.
11. Tebbetts JB. Dual plane breast augmentation: optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg. 2006;118(7 Suppl):81S-98S.
12. Daniel MJB. Inclusão de Prótese de Mama em Duplo Espaço - Prêmio Georges Arié 2004. Rev Bras Cir Plást. 2005;20(2):82-7.
13. Graf RM, Bernardes A, Rippel R, Araujo LR, Damasio RC, Auersvald A. Subfascial breast implant: a new procedure. Plast Reconstr Surg. 2003;111(2):904-8. PMID: 12560720 DOI: http://dx.doi.org/10.1097/01.PRS.0000041601.59651.15
14. Médard de Chardon V, Balaguer T, Chignon-Sicard B, Lebreton E. Double breast contour in primary aesthetic breast augmentation: incidence, prevention and treatment. Ann Plast Surg. 2010;64(4):390-6. PMID: 20224340 DOI: http://dx.doi.org/10.1097/SAP.0b013e3181b14284
15. Spear SL, Bulan EJ, Venturi ML. Breast augmentation. Plast Reconstr Surg. 2004;114(5):73E-81E. PMID: 15457008
16. Handel N. Secondary mastopexy in the augmented patient: a recipe for disaster. Plast Reconstr Surg. 2006;118(7 Suppl):152S-63S DOI: http://dx.doi.org/10.1097/01.prs.0000246106.85435.74
Clínica de Cirurgia Plástica Dr. Estefano Luiz Favaretto, Sertãozinho, SP, Brazil
Institution: Clínica de Cirurgia Plástica Dr. Estefano Luiz Favaretto, Sertãozinho, SP, Brazil.
Corresponding author:
Estéfano Luiz Favaretto
Avenida Braz Olaia Acosta, 727, térreo - Jardim Califórnia
Ribeirão Preto, SP, Brazil - Zip Code 14026-040
E-mail: estefano@elfavarettocirplastica.com.br
Article received: June 30, 2016.
Article accepted: September 26, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter