

Original Article - Year 2017 - Volume 32 -
Reduction mammoplasty with combined Pitanguy technique and Silveira Neto flap for nipple-areolar complex elevation
Mamoplastia redutora com realização de técnica de Pitanguy, associada ao retalho de Silveira Neto para ascensão de complexo areolopapilar
ABSTRACT
INTRODUCTION: Mammary hypertrophy is common, and has great clinical importance, affecting women both psychologically and functionally, especially when severe. To avoid vascular compromise and necrosis associated with reduction mammoplasty in cases with severe hypertrophy and ptosis, a safe option involves combined use of Pitanguy technique and a Silveira Neto areolar superomedial dermoglandular flap.
METHODS: Fourteen reduction mammoplasties were performed between April 2014 and July 2016 with the combined technique. Parenchymal resection ranged from 900 to 1,800 g, and the superior displacement distance of the nipple-areolar complex ranged from 5 to 15 cm. Vascular and scarring complications of the nipple-areolar complex were evaluated.
RESULTS: All patients reported satisfaction with the aesthetic and functional results obtained with surgery. A small area of sloughing where the inframammary crease and the vertical scar intersect was observed in 4 patients; healing occurred by second intention, without significant aesthetic sequelae. Neither sloughing nor partial or total necrosis of the nipple-areolar complex were observed, despite the significant elevation. Two cases of hypopigmentation of a small area at the areolar margin were observed.
CONCLUSION: The combined technique was successful in the treatment of prominent mammary hypertrophy, enabling safe reduction of large volumes, correction of severe ptosis, and significant elevation of the nipple-areolar complex. Good aesthetic and functional results were obtained, without vascular compromise of the nipple-areolar complex.
Keywords: Mammoplasty; Breast/abnormalities; Reconstructive surgical procedures; Surgical flaps; Areola.
RESUMO
INTRODUÇÃO: A hipertrofia mamária é uma alteração do contorno corporal bastante frequente, e de grande importância clínica, já que repercute na mulher tanto psicologicamente como funcionalmente, em especial nas grandes hipertrofias. Para evitar o sofrimento vascular e necroses nos casos de mamoplastias redutoras em grandes hipertrofias e ptoses severas, uma opção segura é a realização de mamoplastia redutora a Pitanguy, associada à confecção de retalho dermoglandular areolado superomedial de Silveira Neto.
MÉTODOS: Foram realizadas, no período de abril de 2014 a julho de 2016, 14 mamoplastias redutoras utilizando a técnica descrita. A ressecção de parênquima variou entre 900 gramas a 1.800 gramas, e a distância de deslocamento superior do complexo areolopapilar variou entre 5 e 15 centímetros. Observou-se a incidência de complicações vasculares e cicatriciais do complexo areolopapilar.
RESULTADOS: Todas as pacientes referiram satisfação com o resultado estético e funcional obtidos pela cirurgia. Em quatro pacientes, houve pequena área de epidermólise na região de encontro do sulco submamário com a cicatriz vertical, que cicatrizaram por segunda intenção, sem causar grandes sequelas estéticas. Em nenhum dos casos houve epidermólise ou necrose parcial ou total do complexo areolopapilar, apesar de grandes ascensões dos mesmos. Houve dois casos de hipocromia em pequena área da margem areolar.
CONCLUSÃO: Para o tratamento de grandes hipertrofias mamárias, a combinação das técnicas selecionadas foi bem-sucedida em possibilitar grandes reduções volumétricas, correção de ptoses severas, com elevação do complexo areolopapilar por distâncias significativas, com segurança. Desta forma, foram obtidos bons resultados estéticos e funcionais, sem sofrimentos vasculares do complexo areolopapilar.
Palavras-chave: Mamoplastia; Mama/anormalidades; Procedimentos cirúrgicos reconstrutivos; Retalhos cirúrgicos; Aréola.
Mammary hypertrophy is a common problem in Brazil. It is of great clinical importance, since it can affect women both psychologically, through its aesthetic effects, and functionally, by leading to postural disorders, physical limitations, and even respiratory discomfort1,2.
Several surgical techniques have been developed to correct this mammary deformity by reducing glandular volume and correcting ptosis, with the intent of obtaining a better aesthetic result. These techniques have achieved greater safety and a lower rate of postoperative complications. Among the complications observed in reduction mammoplasty, especially in severe cases, are unaesthetic scars and changes in the sensitivity of the nipple-areolar complex. However, the most serious complication is vascular compromise of the nipple-areolar complex, with subsequent sloughing and partial or complete necrosis, resulting in major sequelae.
In order to avoid vascular compromise and necrosis in cases of marked hypertrophy and ptosis, which require significant elevation of the nipple-areolar complex, a safe option consists of reduction mammoplasty using the Pitanguy technique, combined with the creation of a dermoglandular mono upper pedicle flap with a medial base, developed by Silveira Neto3.
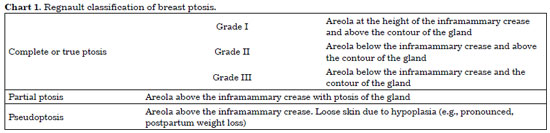
Regnault devised a grading system for mammary ptosis (Chart 1). The system classifies true ptosis in 3 grades, based on the position of the areola relative to the inframammary crease, skin, and mammary gland. Regnault further defined partial ptosis (or glandular ptosis) and pseudoptosis4.
OBJECTIVE
This study aimed to describe the pre- and postoperative characteristics of patients who underwent the combined Pitanguy reduction mammoplasty technique and the Silveira Neto superomedial dermoglandular flap for large elevations of the nipple-areolar complex, to quantify the frequency of vascular and scar complications.
METHODS
This study followed the principles of the Declaration of Helsinki. All patients signed a Free and Informed Consent Form. Fourteen reduction mammoplasties were performed from April 2014 to July 2016 in the Plastic Surgery Hospital, Rio de Janeiro, RJ, using the Pitanguy technique combined with the creation of a dermoglandular mono upper pedicle Silveira Neto flap with a medial base. Patient ages ranged from 19 to 56 years.
The surgical criteria were: the presence of breast hypertrophy and severe ptosis, Regnault grades II and III (Figure 1 and Chart 1), and aesthetic complaints or pain.
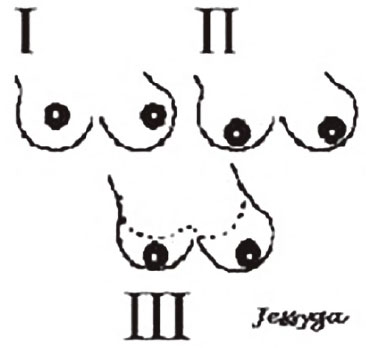
Figure 1. Regnault - Classification of breast ptosis.
Source: Regnault P. Breast ptosis: definition and treatment. Clin Plast Surg. 1976;3(2):193-2034.
Patients with pseudoptosis, partial ptosis, or grade I ptosis (Figure 1 and Chart 1), and patients with prior breast surgeries, current smoking history, and vasculopathies were excluded.
Preoperative assessment included physical examination, with photographs taken in standing, right and left frontal oblique, and right and left profile positions. Laboratory tests, surgical risk discussion, chest X-rays, and breast imaging were performed; ultrasonography was performed for patients under 35 years old and mammography for those over 35.
Patients underwent surgery with general or upper epidural anesthesia with sedation. A semi-seated position was used during the procedure, with the arms abducted to 90 degrees. Surgical marking was performed with methylene blue, using the Pitanguy technique, with point A (Figure 2) indicating the projection of the inframammary crease on the midclavicular line
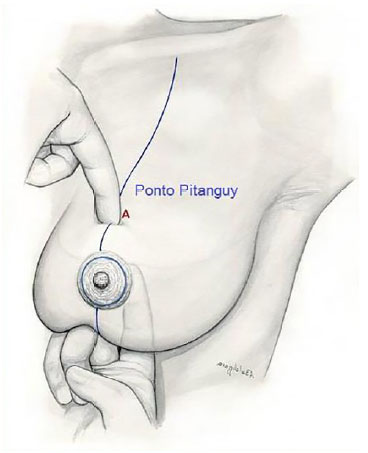
Figure 2. Marking of point A - Projection of the inframammary crease in the midclavicular line.
The amount of tissue to be resected was estimated with digital clamping (Figure 3); points B and C were marked, forming a triangle with point A; then points D and E were marked (Figure 4), corresponding to the medial and lateral limits of the horizontal incision. The first breast was marked and the marking was transferred by wire or compass to the contralateral breast1,2 (Figure 5). Tattooing was performed with a 0.7-mm needle; the breasts were infiltrated with saline solution and epinephrine at a concentration of 1:200,000.
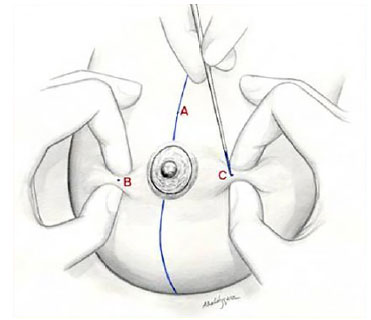
Figure 3. Marking of points B and C - Digital clamping maneuver.
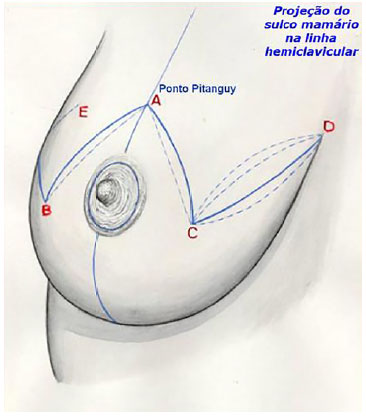
Figure 4. Pitanguy Marking-Pitanguy classic marking.

Figure 5. Pitanguy technique marking.
The incisions were initiated at the areola (Figure 6), with Schwartzman's maneuver of deepithelialization of the periareolar region, while preserving the dermal vascular bed5. Resection of the breast parenchyma was restricted to the lower pole of the breast in a flat or "inverted-keel" form1 (Figure 7).
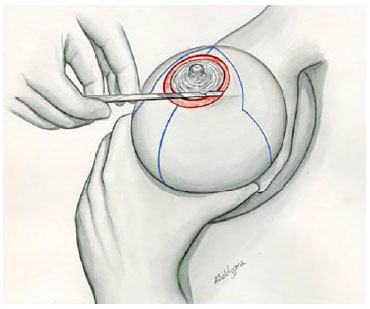
Figure 6. Schwartzman's maneuver with deepithelialization of the periareolar region.
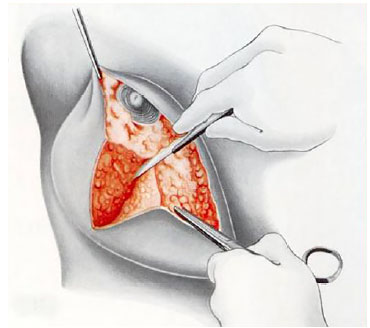
Figure 7. Flat parenchymal resection.
Preparation of the dermoglandular mono upper pedicle flap with a medial base was performed (Figure 8), maintaining a total thickness of approximately 2 to 3 cm (Figure 9), with lateral rotation and elevation of the nipple-areolar complex to point A (Figures 10 and 11),.

Figure 8. Deepithelialization of the superomedial areolar pedicle.

Figure 9. Superomedial areolar pedicle preparation.
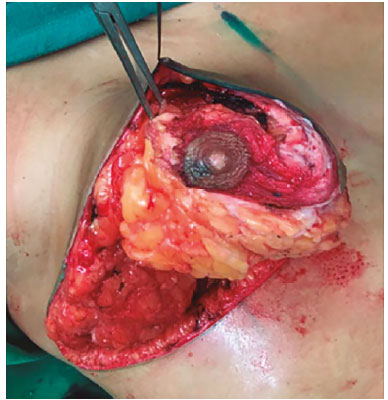
Figure 10. Lateral rotation of the pedicle with elevation of the nipple-areolar complex up to point A.

Figure 11. Final appearance demonstrating elevation of the nipple-areolar complex without tension.
Hemostasis was performed in approaching the medial and lateral pillars of the mammary parenchyma, and from points C to D along a horizontal line; breast assembly was performed using simple and separate points in the vertical and horizontal incisions (Figure 12), with posterior marking of the definitive and most appropriate location of the nipple-areolar complex using an areolotome (Figure 13). No drains were used. Closure was performed in layers using 3-0 and 4-0 nylon suture and skin edges were apposed using 4-0 Monocryl intradermal sutures. Compression dressings were applied and the patient was discharged after 24 hours of observation.
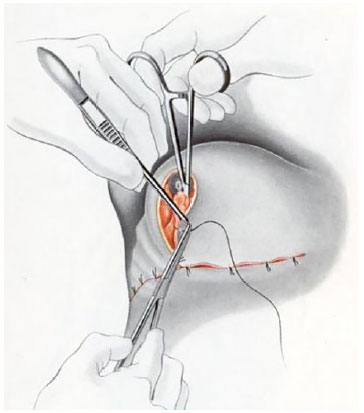
Figure 12. Assembly of the breast cone with single stitches in the vertical and horizontal incisions.
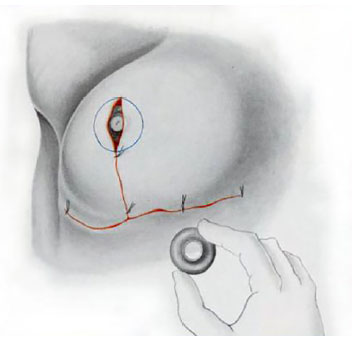
Figure 13. Positioning of the areolar marking using an areolotome.
Parenchymal resection ranged between 900 and 1,800 g, and the superior displacement distance of the nipple-areolar complex varied from 5 to 15 cm.
External stitches were removed by the 14th postoperative day. Weekly follow-up was performed up to the 30th postoperative day, and thereafter at 3, 6, and 12 postoperative months.
RESULTS
The combined surgical technique was performed in 14 patients. Parenchymal resection ranged between 900 and 1,800 g, and the superior displacement distance of the nipple-areolar complex ranged from 5 to 15 cm. All patients reported satisfaction with the aesthetic and functional results of surgery (Figures 14 and 15).
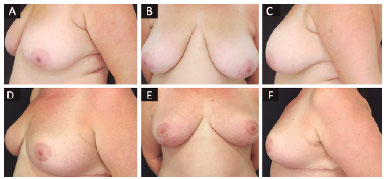
Figure 14. A, B, and C: Preoperative; D, E, and F: Postoperative at 6 months.
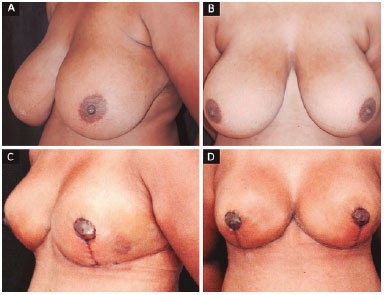
Figure 15. A and B: Preoperative; C and D: Postoperative at 1 month.
A small area of sloughing where the inframammary crease and vertical scar intersect was observed in 4 patients. This healed by second intention, without causing significant aesthetic sequelae. No sloughing or partial or total necrosis of the nipple-areolar complex was observed in any of the patients, despite significant elevation. Two cases of hypopigmentation of a small area at the areolar margin were observed (Figure 16).
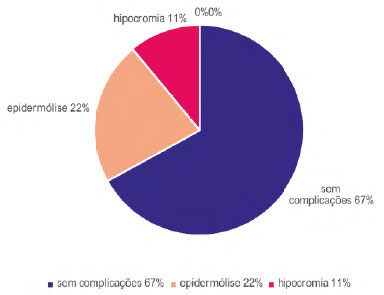
Figure 16. Postoperative complications.
DISCUSSION
Reduction mammoplasty is one of the most commonly performed procedures in plastic surgery. The choice of surgical procedure in each case should take into account the surgical indications, the safety of the method, the postoperative complications, and the long-term results. The treatment of prominent mammary hypertrophy is an even greater challenge, because ptosis is usually more severe, and significant parenchymal resection is needed, making elevation of the nipple-areolar complex and correct positioning difficult.
Thus, there is a need to perform techniques that use vascular pedicles to ensure adequate blood supply, and to avoid areolar injury and necrosis. Several techniques have been described, based mainly on the vascularization of the nipple-areolar complex. These may have two transverse pedicles, as in the technique described by Pitanguy1,2, vertical pedicles, as in the McKissoc6 technique, a single lateral pedicle, as in the Skoog7,8 technique, or a medial pedicle as in the Silveira Neto3 technique.
The technique used in this study, a dermoglandular mono upper pedicle flap with a medial base, described by Silveira Neto in 19763, is based on the vascularization of the internal mammary artery. The technique proved to be effective in cases of prominent hypertrophy, with use of a safe areolar flap, allowing for large displacements of the nipple-areolar complex, and a low risk of ischemic complications or tension-related deformities. This proved to be an excellent alternative to areola-free grafts in the most difficult cases, with the advantage of promoting greater aesthetic quality and better sensitivity of the areolar region.
CONCLUSION
The combination of the selected techniques was successful in the treatment of prominent mammary hypertrophy, enabling the safe reduction of large volumes, correction of severe ptosis, and elevation of the nipple-areolar complex by significant distances. Thus, good aesthetic and functional results were obtained, without vascular compromise of the nipple-areolar complex.
COLLABORATIONS
LARG Analysis and interpretation of data; conception and design of the study; performing surgeries; writing the manuscript.
FH Critical review e final approval of the manuscript.
REFERENCES
1. Pitanguy I. Une nouvelle technique de plastie mammaire. Étude de 245 cas consécutifs et présentation d'une technique personnelle. Ann Chir Plast (Marseille). 1962;7(3):199-208.
2. Pitanguy I, Salgado F, Radwansky HN. Reduções mamárias: técnicas pessoais sem descolamento cutâneo. In: Mélega JM, ed. Cirurgia plástica: fundamentos e arte. Cirurgia Estética. Rio de Janeiro: Médica e Científica; 2003. p. 477-84.
3. Silveira Neto E. Mastoplastia redutora setorial com pedículo areolar interno. In: Anais do XIII Congresso Brasileiro de Cirurgia Plástica e I Congresso Brasileiro de Cirurgia Estética; Abr 1976; Porto Alegre, RS, Brasil. EMMA.
4. Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976;3(2):193-203.
5. Schwarzmann E. Die technik der mammaplastik. Chirurg. 1930;2:932-43.
6. McKissock PK. Reduction mammaplasty with a vertical dermal flap. Plast Reconstr Surg. 1972;49(3):245-52. PMID: 4551235 DOI: http://dx.doi.org/10.1097/00006534-197203000-00001
7. Skoog T. A technique of breast reduction; transposition of the nipple on a cutaneous vascular pedicle. Acta Chir Scand. 1963;126:453-65. PMID: 14072329
8. Skoog TG. Breast hypertrophy. A method of reduction. In: Skoog TG, ed. Plastic surgery: New method and refinements. Philadelphia: Saunders; 1974. p. 333-80.
1. Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
2. Hospital Universitário Clementino Fraga Filho, Rio de Janeiro, RJ, Brazil
3. Hospital da Plástica, Rio de Janeiro, RJ, Brazil
Institution: Hospital da Plástica, Rio de Janeiro, RJ, Brazil.
Corresponding author:
Luciana Abdalla Rosa Gasparoni
Rua Visconde de Pirajá, 351, sala 614 - Ipanema
Rio de Janeiro, RJ, Brazil - Zip Code 22410-906
E-mail: lucianabdalla@hotmail.com
Article received: July 14, 2016.
Article accepted: September 19, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter