

Case Report - Year 2017 - Volume 32 -
Bone reabsorption associated with silicone implants in mentoplasty: a clinical case report
Reabsorção óssea associada ao implante de silicone em mentoplastia: relato de caso clínico
ABSTRACT
For many years, silicone implants were used in reconstructive and esthetic surgeries, especially in cases in which the facial profile of patients presented deficiencies in the inferior third of the face. This material proved to be successful in most aspects. However, several complications were well reported in the literature, as the case of bone reabsorption in the region of the mandibular chin. In this article, the authors present two clinical cases of bone reabsorption from the anterior cortex of the chin associated with silicone implants and discuss the etiology, complications, and treatment plan.
Keywords: Mentoplasty; Bone reabsorption; Silicones.
RESUMO
Durante muitos anos, os implantes de silicone foram utilizados em cirurgias reconstrutivas e estéticas, principalmente em casos em que o perfil facial do paciente apresenta deficiência no terço inferior da face. Este material tem provado ser bem sucedido na maioria dos aspectos, contudo, algumas complicações já foram bem relatadas na literatura, como é o caso das reabsorções ósseas na região de mento mandibular. No presente artigo os autores apresentam dois casos clínicos de reabsorção óssea da cortical anterior do mento, associada ao implante de silicone e discutem a etiologia, as complicações e o plano de tratamento.
Palavras-chave: Mentoplastia; Reabsorção óssea; Silicones.
The pillar of face surgery is the quest for harmony through remodeling of tissue contours. Towards this goal, several alloplastic materials are used. The materials currently available in the market largely vary in density, remodeling, tissue reaction, reabsorption, migration, incidence of infections, extrusion rate, and the ease of removal1.
Aspects, such as low toxicity, carcinogenic potential, satisfactory bioactivity to prevent organ rejections, and sufficient stability to support the physiological environment and to avoid changes in the receptor site, would be crucial to achieve the success and longevity of the treatment2.
The advantages of silicone implants include a lower risk for sensory loss and the possibility to be removed, if the result is unsatisfactory; conversely, the disadvantages include asymmetry, malposition, hematoma, seroma, infection, mobility, extrusion, and bone reabsorption3.
When removal of the implant material is required owing to any of the aforementioned reasons, lip ptosis might occur owing to the lack of insertion of the chin muscle of the mandible; in these cases, the best option would be to perform mentoplasty via basilar osteotomy4,5.
However, care should be taken while suturing the chin muscle so that lip ptosis does not occur, regardless of the technique used.
OBJECTIVE
In this article, the authors present two clinical cases of bone reabsorption of the anterior cortex of the chin associated with silicone implants and discuss the etiology, complications, and treatment plan.
CASE REPORT
Case 1
Patient D.S., a 53-year-old woman with leukoderma, was sent for evaluation of a radiolucent lesion in the chin region. This was observed by the endodontist after requesting a computed tomography (CT) scan to evaluate the fracture of a tooth in the chin region. During the anamnesis, the patient was reported to have silicone chin implants for almost 38 years, without any complaint in the region.
During the extra-oral examination, no changes, such as lip ptosis, pain upon palpation, or any sensitivity change in the region of the inferior lip (dysesthesia), were observed. During the intra-oral examination, no changes were observed in the color of the mucous membranes or the shape of the oral vestibule. CT evaluation revealed a delimited hypodense area, which extended from the region of teeth 33 to 44 (Figures 1 and 2). On the percussion and thermal pulp vitality tests, positive responses were obtained in all teeth adjacent to the lesion. With the collected clinical data and tomographic analyses, the hypothesis of bone reabsorption related to silicone implant was clear; therefore, the removal of the silicone prosthesis associated with mentoplasty via basilar osteotomy was proposed.

Figure 1. Three-dimensional computed tomography reconstruction image demonstrating an extension of the injury.
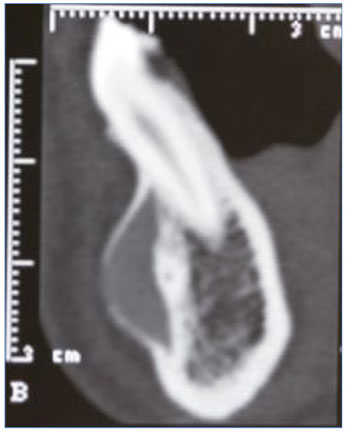
Figure 2. Sagittal tomographic section showing bone reabsorption in the proximity of the root of tooth 33.
Case 2
Patient J.J.J., a 29-year-old woman with leukoderma, was referred by the orthodontist for evaluation of a class II facial tooth deformity and temporomandibular disorders. During the anamnesis, the patient was reported to have been submitted to rhinoplasty and silicone implantation in the chin region ~10 years ago. During the intra and extra-oral clinical examinations, no change was observed on the mucous membrane or skin in the chin region; there were also no paresthesia, dysesthesia, and pain upon palpation.
After requesting for preoperative imaging examinations (CT), a hypodense lesion extending from the region of teeth 33 to 43 (Figures 3 and 4) was observed, with expansion of the vestibular cortex. The results of the percussion and thermal pulpal vitality tests were positive in all teeth close to the lesion. Based on the tomographic and clinical findings, the diagnostic hypothesis of bone reabsorption related to silicone implant was obtained.
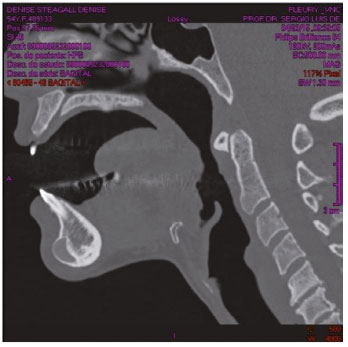
Figure 3. Sagittal section of computed tomography.

Figure 4. Axial section showing bone reabsorption and three-dimensional reconstruction of the implant extension.
The proposed treatment was removal of the silicone prosthesis associated with mentoplasty via basilar osteotomy.
DISCUSSION
The first reports of failure related to alloplastic implants were described by Robinson6 in 1972 in which 12 of 14 patients submitted to acrylic and silicone implantations presented bone reabsorptions of up to 5 mm. In this article, reabsorption was attributed to the shape of the implant or its positions. In other reports, the etiology was related to the pressure exerted by large implants, subperiosteal placement, and implant hardness1,4.
Besides producing a significant defect with potential damages to underlying structures, such as tooth roots and nerves, bone reabsorption may also be responsible for the loss of chin projection. Radiographically, reabsorption seems to occur 12 months after placing the implants; however, there are reports of bone reabsorption at 2 months follow-up5-7.
Of all regions, the chin seems to be the most affected owing to the thickness of the vestibular cortex and the great tension exerted by the chin muscle; conversely, bone reabsorption is rare in other regions, such as in the zygomatic region owing to the bone density and minimum muscle tension exerted by the facial muscles against this bone8.
Patients with class II facial tooth deformities (long lower third of the face and lip incompetence) seem to be more predisposed to bone reabsorption in implants installed in the chin owing to the fact that this hyper-function takes pressure and to the migration of the implant superiorly on the thinner bone, which predisposes the reabsorption. In addition, implants are more sensitive to be placed in these patients for esthetic purposes4,9.
In case of severe reabsorption, implant removal should be considered. Serious distortions of the soft tissues have been reported after its removal10. Owing to this, mentoplasty should be performed via basic osteotomy in the same surgical time as a prophylactic measure to avoid residual deformities10. In both the cases reported above, these were the treatments used.
Basilar chin osteotomy is a procedure that offers many advantages over other techniques for chin augmentation, e.g., better contour of the soft tissues by the maintenance of the mandibular base, predictability, versatility in three-dimensional correction, and maintenance of the joined mobile pedicle that allows better viability of the osteotomized segment10 (Figure 5).
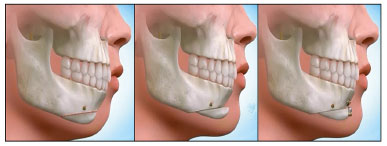
Figure 5. Scheme of a basic osteotomy of the chin using Dolphin Imaging 11.8 Premium® (Dolphin Imaging & Management Solutions, Chatsworth, CA).
Basilar mentoplasty with silicone implants has yielded concerns over the years owing to the complications that are well reported in the literature. When considering the removal of these implants, osteotomy should be planned to avoid residual deformities.
COLLABORATIONS
GCR Writing the manuscript or critical review of its contents.
SLM Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; writing the manuscript or critical review of its contents.
RM Conception and design of the study; completion of surgeries and/or experiments.
HCLS Writing the manuscript or critical review of its contents.
MVFM Writing the manuscript or critical review of its contents.
REFERENCES
1. Cuzalina LA, Hlavacek MR. Complications of facial implants. Oral Maxillofac Surg Clin North Am. 2009;21(1):91-104. DOI: http://dx.doi.org/10.1016/j.coms.2008.10.009
2. Sclafani AP, Romo T 3rd. Biology and chemistry of facial implants. Facial Plast Surg. 2000;16(1):3-6. DOI: http://dx.doi.org/10.1055/s-2000-7320
3. Scaccia FJ, Allphin AL, Stepnick DW. Complications of augmentation mentoplasty: a review of 11,095 cases. Int J Aesth Rest Surg 1993;1(1):3-8. DOI: http://dx.doi.org/10.1177/074880689301000306
4. Matarasso A, Elias AC, Elias RL. Labial incompetence: a marker for progressive bone resorption in silastic chin augmentation. Plast Reconstr Surg. 1996;98(6):1007-14. DOI: http://dx.doi.org/10.1097/00006534-199611000-00012
5. Peled IJ, Wexler MR, Ticher S, Lax EE. Mandibular resorption from silicone chin implants in children. J Oral Maxillofac Surg. 1986;44(5):346-8. DOI: http://dx.doi.org/10.1016/S0278-2391(86)80028-3
6. Robinson M. Bone resorption under plastic chin implants. Follow-up of a preliminary report. Arch Otolaryngol. 1972;95(1):30-2. DOI: http://dx.doi.org/10.1001/archotol.1972.00770080078006
7. Friedland JA, Coccaro PJ, Converse JM. Retrospective cephalometric analysis of mandibular bone absorption under silicone rubber chin implants. Plast Reconstr Surg. 1976;57(2):144-51. PMID: 1250884 DOI: http://dx.doi.org/10.1097/00006534-197602000-00002
8. Hinderer UT. Nasal base, maxillary, and infraorbital implants-alloplastic. Clin Plast Surg. 1991;18(1):87-105. PMID: 2015752
9. Ward J, Podda S, Garri JI, Wolfe SA, Thaller SR. Chin deformities. J Craniofac Surg. 2007;18(4):887-94. DOI: http://dx.doi.org/10.1097/scs.0b013e3180684401
10. Cohen SR, Mardach OL, Kawamoto HK Jr. Chin disfigurement following removal of alloplastic chin implants. Plast Reconstr Surg. 1991;88(1):62-6. DOI: http://dx.doi.org/10.1097/00006534-199107000-00010
1. Universidade de Santo Amaro, São Paulo, SP, Brazil
2. Conselho Federal de Odontologia, Brasília, DF, Brazil
3. Universidade Federal de São Paulo, São Paulo, SP, Brazil
4. Hospital Israelita Albert Einstein, São Paulo, SP, Brazil
5. Hospital São Luiz do Morumbi, São Paulo, SP, Brazil
6. Hospital Itaim, São Paulo, SP, Brazil
7. Universidade Federal de Mato Grosso do Sul, Campo Grande, MS, Brazil
Institution: Hospital Israelita Albert Einstein, São Paulo, SP, Brazil.
Corresponding author:
Henrique Celestino Lima e Silva
Rua Martiniano de Carvalho - Bloco A, Bela Vista
São Paulo, SP, Brazil Zip Code 01321-001
E-mail: henriquelimacirurgia@gmail.com
Article received: February 8, 2017.
Article accepted: April 23, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter