

Case Report - Year 2017 - Volume 32 -
Rhinophyma: a surgical treatment option
Rinofima: opção cirúrgica como tratamento
ABSTRACT
INTRODUCTION: Rhinophyma is a condition involving chronic inflammation of the nose and is characterized by progressive hypertrophy and hyperplasia of sebaceous glands and connective tissue. Rhinophyma leads to an appearance of nasal elephantiasis, which is caused by the congestion of dermis vessels. Its etiology is mostly associated with alcohol abuse. Rhinophyma is considered by some researchers to be an advanced stage of acne rosacea. Here, we report a case of rhinophyma that was surgically treated with decortication and electrocoagulation at the Plastic Surgery Service of the University Hospital of the Federal University of Santa Catarina.
METHODS: A review of medical and photographic records of a case of rhinophyma was conducted.
RESULTS: The patient was underwent surgical treatment with favorable outcomes.
CONCLUSION: There are several treatments for rhinophyma, with decortication and electrocoagulation being an excellent therapeutic option.
Keywords: Rhinophyma; Surgical reconstructive procedures; Nasal diseases; Nose.
RESUMO
INTRODUÇÃO: Rinofima é uma inflamação crônica dos tecidos do nariz, caracterizada por hipertrofia e hiperplasia progressivas das glândulas sebáceas e do tecido conjuntivo. Determina um aspecto de elefantíase nasal, secundária à congestão dos vasos da derme. Sua etiologia está associada, na maioria dos casos, ao uso abusivo de álcool. É considerada por alguns autores como sendo um estágio avançado de acne rosácea. O artigo tem como objetivo relatar um caso de rinofima, tratado cirurgicamente no Serviço de Cirurgia Plástica do Hospital Universitário da Universidade Federal de Santa Catarina com decorticação e eletrocoagulação.
MÉTODO: Foi realizado revisão de prontuário e registro fotográfico de um caso de rinofima.
RESULTADOS: Paciente foi submetido a tratamento cirúrgico com evolução favorável.
CONCLUSÃO: Existem diversos tratamentos para rinofima, sendo que a decorticação e a eletrocoagulação constituem uma excelente opção terapêutica.
Palavras-chave: Rinofima; Procedimentos cirúrgicos reconstrutivos; Doenças nasais; Nariz.
Rhinophyma is a condition involving chronic inflammation of the nose and is characterized by abnormal coloration and texture, vascularization impairment, irregular exophytic growth, and telangiectasias1. It features progressive hypertrophy and hyperplasia of sebaceous glands and nasal subjunctive tissue, which are caused by the congestion of dermis vessels2. These alterations can culminate in a complete deformation of the nose.
Although usually asymptomatic, it can lead to a mechanical compression of nasal structures, in addition to significant emotional impairment. This results in the appearance of elephantiasis. Historically, it was associated with various other names, such as hyperplastic acne, "cauliflower" nose, "potato" nose, or "drinker" nose2. In 1845, Hebrea used a terminology derived from the Greek rhino (nose) and phyma (growth), which resulted in rhinophyma becoming the universally accepted name3.
Its etiology is not fully understood. Some authors associate this disease with an advanced stage of centrofacial acne rosacea, and they consider it an uncommon subtype (3.7%)4,5. However, other authors believe that rhinophyma is a different disease, since, unlike rosacea, it prevails in men and can manifest without typical acne.
There is evidence of associated genetic factors. Cases of twins, uncles, or grandparents of patients affected have been described. Previously, several risk factors have been described, including alcohol abuse and sunlight exposure. It is also described in association with condiments, caffeine, hot foods, and other factors causing facial redness6.
The diagnosis is mostly clinical and should be differentiated from acne vulgaris, seborrheic dermatitis, lupus erythematosus, mycosis fungoides, sarcoidosis, and cutaneous tuberculosis7. Drug treatment, particularly for advanced cases, seems to provide less satisfactory results than does surgical treatment8. The literature describes some surgical options, all of which seek to remove sebaceous glands and to promote the recovery of nasal contour9.
OBJECTIVE
In this report, we describe a case of rhinophyma that was surgically treated at the Plastic Surgery Service of HU/UFSC (University Hospital, connected to the Federal University of Santa Catarina), Florianópolis, SC, with decortication and electrocoagulation.
CASE REPORT
A 63-year-old male patient sought medical attention at the Plastic Surgery Service of HU/UFSC, with complaints of progressive nasal volume associated with deformity and difficulty in breathing that had worsened over the preceding 10 years. A significant history of sun exposure was described in his medical records, along with notes that he did not consume alcohol or smoke. He also did not present with other pathologies.
Upon physical examination, a significant increase in nasal volume, telangiectasias, erythema, cutaneous thickening, nodules, and dilated pilosebaceous pores were observed. An impaired chin area and ear lobes were also detected, as shown in f'igure 1. For these reasons, we suspected rhinophyma. Clinical treatment for this suspected condition was never performed. We observed lowering of the external nasal valve, with no changes in inspiration.
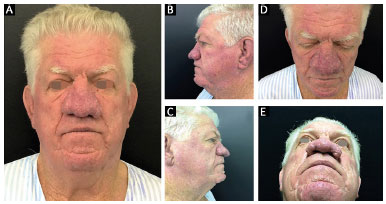
Figure 1. Preoperative evaluation. A: Patient with increased nasal volume and chin impairment; B and C: Pre-operative profile pictures of the patient; D: Top view where telangiectasias, erythema, and cutaneous thickening can be observed; E: Image shows the mechanical compression of nasal structures.
The patient was placed under general anesthesia. After local infiltration with anesthetic and vasoconstricting solution, surgical resection was conducted using a cold scalpel (blade 20). The entire compromised area was resected in the nasal region, while preserving cartilage and an approximate subcutaneous segment of 1-2 mm. This was followed by cauterization with electrocautery. Cauterization of the chin region and ear lobes was performed, as shown in figure 2.
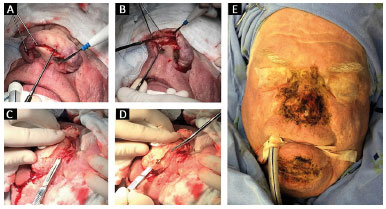
Figure 2. Surgical procedure. A and B: Images showing the rhinophyma resection plan; C and D: Surgical resection with a cold scalpel. The entire affected area in the nasal region was resected, preserving the subcutaneous tissue and cartilage; E: Cauterization with electrocautery. Cauterization of the chin region.
Healing by second intention was chosen (i.e., no grafts were used). Daily dressings with essential fatty acids oil were applied in the area from the immediate postoperative period until complete healing (i.e. for approximately 60 days). The anatomopathological report corroborated the clinical suspicion of rhinophyma (Figure 3).
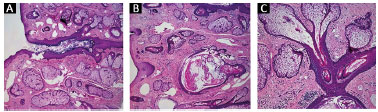
Figure 3. Anatomopathological evaluation of the resected area. The images indicate the presence of sebaceous hyperplasia with dilated follicular units and keratin "plugs" in the dermis. Fibrosis and mononuclear inflammatory infiltration surrounding the area can be observed. A: 40x magnification image; B: Image with 40x2 increase; C: 100x magnification image.
The patient presented a quite favorable evolution and was satisfied with the aesthetic and functional results, showing improved emotional and respiratory aspects. His evolution was complete 60 days after surgery (Figure 4). Nasal dyschromia of the scar was shown, without other changes. The procedure performed in this case and the reporting of its outcomes followed the principles of the Declaration of Helsinki, revised in 2000. The patient provided written informed consent, which provided for the use of information contained in his medical record as well as the publication of his images.
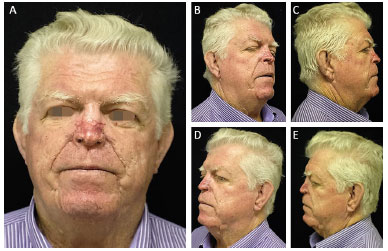
Figure 4. Postoperative day 60. Pictures of the patient, 60 days after surgery. A: Image showing complete healing of the nasal region with dyschromic scar; B and C: Right profile pictures of the patient, indicating optimal results; D and E: Left profile pictures of the patient 60 days after rhinophyma.
DISCUSSION
Rhinophyma is a pathology that requires aggressive treatment, not only due to the aesthetic and functional deformity that it causes, but also due to the risk of associated malignancy. Malignancy may occur, thereby possibly resulting in basal cell carcinoma and, more rarely, squamous cell carcinoma or angiosarcoma7. In this case, no associated neoplasia was found.
In considering the etiology of rhinophyma related to acne rosacea, we suggest classifying the subtype according to the degree of impairment10. Acne rosacea is a form of chronic inflammation without a permanent cure. In the early stages, combination therapy offers better results when compared to monotherapy10. Conversely, for advanced cases, such as rhinophyma, patients are advised to undergo surgical treatment, which results in the removal of sebaceous, hypertrophic, and hyperplasic glands; re-establishes nasal contour; and possibly resolves respiratory difficulty caused by the mechanical compression of the nose.
Several surgical techniques have been described in the literature, including graft excision or skin flap application; excision with healing by second intention; CO2 or argon laser ablation; cryosurgery, electrosurgery; and dermabrasion2.
There is no consensus regarding the best surgical treatment option. However, certain techniques are more beneficial, such as those that remove potentially associated tumors when opting for resection. Several authors do not recommend local flaps, which is an aggressive treatment for an otherwise benign pathology. However, in some severe cases, such as exceptional conduct, partial skin grafting is recommended2.
The complications resulting from treatment, regardless of the therapeutic option, include unsightly scars, asymmetry, and dyschromia. Among these complications, perforation is considered to be the most serious. In addition, the risk of relapse should be considered. In the case reported herein, we chose surgical resection followed by electrocoagulation, without intercurrences.
CONCLUSION
As a stigmatizing disease that presents with deformity and malignant potential, rhinophyma should be considered during medical evaluation. Surgical resection is one of the available therapeutic options that can have promising results. In our clinic, the patient presented herein experienced a satisfactory evolution regarding aesthetic and functional aspects following resection and electrocoagulation. We consider this technique to be a simple, efficient, and safe procedure.
COLLABORATIONS
ICL Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
DOB Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
DFVA Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
GPW Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
AKDA Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
REFERENCES
1. Stark R. Plastic Surgery of the Head and Neck. vol. 1. New York: Churchill Livingstone; 1987. p. 595-600.
2. Costa TC, Firme WAA, Brito LMR, Vieira MBG, Leite LAS. Rinofima: opções cirúrgicas utilizadas no Serviço de Cirurgia Plástica do Hospital Agamenon Magalhães - PE. Rev Bras Cir Plást. 2010;25(4):633-6. DOI: http://dx.doi.org/10.1590/S1983-51752010000400012
3. Mathes S, Weinberger S, Hentz V. Plastic surgery: tumors of head, neck and skin. 2nd ed. Philadelphia: W. B. Saunders; 2006. p. 254.
4. Espinosa Reyes JA, Parra Valencia DP. Rinofima: una revisión de la literatura. Acta Otorrinolaringol Cir Cabeza Cuello. 2012;40(3):220-7.
5. Khaled A, Hammami H, Zeglaoui F, Tounsi J, Zermani R, Kamoun MR, et al. Rosacea: 244 Tunisian cases. Tunis Med. 2010;88(8):597-601. PMID: 20711968
6. Zanini SA, Carreirão S, Lessa S. Cirurgia do Nariz. Rinologia e Rinoplastia: Funcional, Reparadora e Estética. Rio de Janeiro: Revinter; 1994. p. 89-94.
7. Sperli AE, Freitas JOG, Fischler R. Rinofima: tratamento com equipamento de alta frequência (radiofrequência). Rev Bras Cir Plástica. 2009;24(4):504-8.
8. Gupta AK, Chaudhry MM. Rosacea and its management: an overview. J Eur Acad Dermatol Venereol. 2005;19(3):273-85. DOI: http://dx.doi.org/10.1111/j.1468-3083.2005.01216.x
9. Sadick H, Goepel B, Bersch C, Goessler U, Hoermann K, Riedel F. Rhinophyma: diagnosis and treatment options for a disfiguring tumor of the nose. Ann Plast Surg. 2008;61(1):114-20. PMID: 18580161 DOI: http://dx.doi.org/10.1097/SAP.0b013e31815f12d2
10. Weinkle AP, Doktor V, Emer J. Update on the management of rosacea. Clin Cosmet Investig Dermatol. 2015;8:159-77. DOI: http://dx.doi.org/10.1097/PSN.0000000000000111
1. Hospital Universitário Polydoro Ernani de São Thiago, Universidade Federal de Santa Catarina, Florianópolis, SC, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Hospital Universitário Polydoro Ernani de São Thiago, Universidade Federal de Santa Catarina, Florianópolis, SC, Brazil.
Corresponding author:
Daniel Ongaratto Barazzetti
Rua Tereza Pezzi, 1200 - São Leopoldo
Caxias do Sul, RS, Brazil Zip Code 95080-570
E-mail: danielbarazzetti@hotmail.com
Article received: October 1, 2016.
Article accepted: February 21, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter