

Ideas and Innovation - Year 2017 - Volume 32 -
The peninsula in rhytidoplasty
A península na ritidoplastia
ABSTRACT
INTRODUCTION: High implantation of the hairline by the ear is a frequent, unpleasant stigma in rhytidoplasties. To overcome this problem, we created the Peninsula technique in the mid-1999. Initially used in secondary face liftings, its indication has since been broadened, becoming indispensable in primary cases of high hair implantation and in patients requiring major skin resection.
METHODS: The total number of rhytidoplasties performed was 7,356, with 2,512 patients operated using the Peninsula technique from 1999 to 2016. Mean age was 48, 98% were females and 2% males. The technique presents three variants.
RESULTS: Patients were monitored on a monthly basis until discharge at the end of six months. Among the results, there were some complications, which are usual in any type of facial surgery. In the great majority of cases, with the use of the Peninsula, it was possible to obtain good skin traction, with the greater correction of the mid third, maintaining the capillary implantation line.
CONCLUSION: We can conclude that the Peninsula technique is a unique resource, easily reproducible, capable of reducing the learning curve in rhytidoplasty, as it allows generous skin resection without changing capillary implantation, avoiding post-surgical stigma and optimizing the quality of the results and patient satisfaction, with a little scar burden.
Keywords: Rhytidoplasty; Lifting; Face; Hair.
RESUMO
INTRODUÇÃO: A ascensão do pé do cabelo é um estigma frequente e desagradável nas ritidoplastias. Para contornar esse problema, criamos a técnica da Península em meados de 1999. Inicialmente utilizada nas faces secundárias, sua indicação foi ampliada, tornando-se imprescindível nos casos primários de implantação alta do cabelo e naqueles pacientes que necessitariam de grande ressecção de pele.
MÉTODOS: O total de ritidoplastias realizadas foi de 7356, tendo sido operados 2512 pacientes utilizando a técnica da Península, no período que cursa entre 1999 e 2016, com idade média de 48 anos, sendo 98% dos pacientes do sexo feminino e 2% do sexo masculino. A técnica apresenta três variantes.
RESULTADOS: Os pacientes continuaram, posteriormente, em acompanhamento mensal até a alta ao final de 6 meses. Dentre os resultados, surgiram algumas complicações, comuns a qualquer tipo de cirurgia da face. Na grande maioria dos casos, com a utilização da Península, foi possível a realização de uma boa tração cutânea, com maior correção do terço médio, mantendo a linha de implantação capilar.
CONCLUSÃO: Podemos concluir que a técnica da Península é um recurso único, de fácil reprodução, capaz de reduzir a curva de aprendizado em ritidoplastias, uma vez que permite generosa ressecção de pele sem alteração da implantação capilar, atuando de modo a evitar estigmas pós-cirúrgicos e otimizando a qualidade dos resultados e satisfação por parte dos pacientes, com pequeno ônus cicatricial.
Palavras-chave: Ritidoplastia; Remoção; Face; Cabelo.
High implantation of the hairline by the ear is a frequent, unpleasant stigma in rhyitidoplasties. To overcome this problem, we developed the Peninsula technique in 1999, and it was initially used in secondary face liftings. Since then, its indication has been broadened, becoming indispensable in primary cases of high hair implantation and in patients with excessive flaccidity of the mid third of the face, requiring large skin resections. As a transitional element between the cranial and mid thirds, it is a unique resource allowing generous skin resection without changing the hairline1.
Eventual remaining scars from previous surgeries do not prevent the use of the Peninsula technique. Measurements have change as we acquired more experience with the technique, which presents three variants.
The principles and measurements are similar in any of the variants and will be discussed below.
OBJECTIVE
To demonstrate an alternative technique for use in secondary or primary rhytidoplasties in patients with high hairline implantation thus avoiding stigmatization.
METHODS
A total 7,356 rhytidoplasties were performed, with 2,512 patients operated in the period between 1999 and 2016 using the Peninsula technique, mean age was 48 years, 98% were females and 2% males.
During the rhytidoplasties, we started with a pre-capillary incision in the cervical mastoid region, followed by retroauricular and pre-auricular (pre-tragal) incisions, and then we performed the Peninsula.
The principles and measurements are similar in all variants (Figure 1). The base for the demarcation of this technique starts at Point A, from which the implantation of the hairline is contoured to point B and this AB distance varies between 2.5 and 3cm. The BC inclination, 5 to 8 cm from one point to the other, will follow the direction of the desired traction, defined at the moment of resection according to the exceeding tissue. This measurement is repeated between Points A and C. Beyond Point C, there are modifications depending on the type of variant to be executed1.

Figure 1. The peninsula is part of a set of incisions. It represents an important element linking the frontal region and the mid face. Its measurements are not rigit, but must be maintained without the described parameters.
In cases aiming to correct only the lateral portion of the upper third of the face and tail end of the eyebrows, the Temporal variant is indicated, and from Point C the marking continues to Point D.
In cases aiming to correct the cranial third of the face as a whole, approaching not only the tail end, but also the head of the eyebrows, in addition to treatment of the frontal region musculature, the Frontal variant is indicated, and, from one side of Point C, we move on to Point C on the contralateral side.
In the cases of patients with high hairline implantation, which might become exacerbated in the case of intracapillary traction, the Frontal Pre-capillary variant is indicated. From Point C, the marking goes to Point D and continues in a zigzag shape along the hairline the contralateral Point D.
After the incisions, we proceed with skin detachment, lipectomy with scissors, followed by closed liposuction with a cannula 3 from the submental region, liposuction with an open RP5 cannula of SMAS/Platysma, plication in the form of an anteriorized sickle and hemostasis. Soon after, traction is applied with exeresis of skin excess, placement of a portovac drain number 14 and suture. Finally, we put on dressings with face cushioning and crepon.
While hospitalized, patients were monitored by nursing technicians trained for this type of function.
During the two-day hospitalization, the eyelid stitches (made with Seda 6.0 thread) were removed, and the head was washed. The other stitches were removed between 5 to 12 days. The last to be removed were those from the earlobes, which were protected with micropore tape for 15 more days. Lymphatic drainage was allowed after postoperative day four.
RESULTS
Patients were subsequently submitted to a monthly examination until discharge at six months.
Among the results, complications such as a hematoma (more frequent in males), skin suffering/necrosis, nerve lesion, technical failure, anaesthesia, poor scarring, infection, residual bruising, foreign body, alopecia were observed. All of them are common in any type of facial surgery, although nothing can be compared to the dissatisfaction. In the great majority of cases, with the use of the Peninsula technique, it was possible to perform good skin traction, with greater correction of the mid third, without raising the hairline implantation by the ear.
DISCUSSION
Peninsula Variants
Temporal Peninsula
Indicated in primary and secondary surgeries. The figure illustrates the initial measurements: AB 2.5 to 3 cm; AC/CB 5 to 8 cm; CD varies in size and curvature, depending on whether it is a primary or secondary case (Figure 2). The intention to raise the tail end of the eyebrows will also influence its orientation and dimension1,2 (Figure 3).
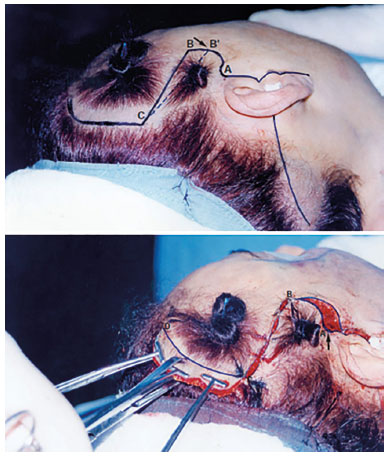
Figure 2. Insertion of point B.

Figure 3. Holding the scissors are shown above makes dissection easier and safer.
Demonstrating the evolution of the Peninsula, the BA distance decreased to B`A, whose scar ended up becoming barely perceptible, thereby expanding its indication in primary cases. On the other hand, CB migrated to CB`, whose new inclination became more aligned with the traction vector of that area (Figure 2): Point B returns to its original position; strong traction of the CB flap; the assistant pushes the scalp forward; Point C is the start of the anchorage; traction and marking of the temporal flap to be resected; marking of Point A; broad resection of the flap that this approach allows, without raising the hairline implantation by the ear1.
Frontal Peninsula
Imagine the coronal incision going to Point A. The peninsula interferes with this pathway. As a routine, for complete facial surgery, one begins with the neck, then the face, and, finally, with any variant of the frontal region. Point B is marked boldly and repeated to emphasize its importance in the dynamics of the technique (Figure 4). The dissection is subgalic above Point B and superficial below. Between the two dissection planes, the Y pedicle is preserved where the frontal branch of the facial nerve passes by1,3-5.

Figure 4. Demarcation of pre-capillary frontal peninsula.
For traction of the Peninsula, it is fundamental to return Point B to the original position to avoid any type of elevation. This point is the initial marking for the creation of the Peninsula. In the following stage, the assistant vigorously pushes the scalp forward, while the surgeon simultaneously tractions the cranial flap backwards. This set of maneuvers provides reasonable tension, essential to achieve the objective of the technique. The procedure continues with action in the frontal region, finishing with the temporal remnant1.
Depending on the case, the traction components of the Peninsula may or may not be preceded by cervical traction. Point A is pushed a forward with a d'Assunção mini forceps, followed by the creation of a small flap that will fill this point1.
The resection follows a harmonious line, avoiding rectification of the scar, which could be detrimental to the principles of the technique (Figure 5).
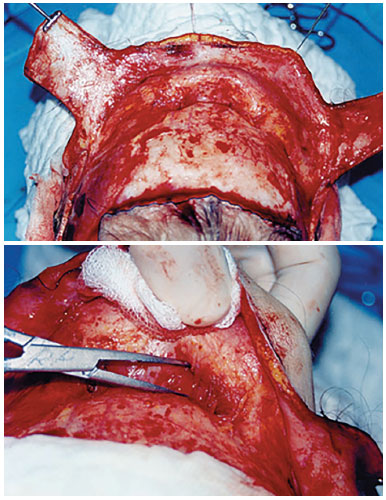
Figure 5. Extensive release of the flap with treatment of the frontal musculature.
The fixation point at A is followed by the resection of the Peninsula flap. There should not be any tension in the AB segment so that it results in an almost imperceptible scar. The earlobes and pre-auricular points are likewise demarcated without tension (Figure 4).
Pre-Capillary Frontal Peninsula
The Pre-Capillary Frontal Peninsula blends in with the Temporal. The jagged incision, along with the frontal hairline implantation, penetrates around half a centimetre into the hairline implantation (Figure 6). The technical indication for this surgery is secondary face lifting with a scant, almost non-existing hairline, aging of the face with predominance in the frontal region, which is wide, whether the result or not of previous surgery.

Figure 6. Pre and postoperative of a frontal peninsula.
Surgical sequence: neck; face; Peninsula; temporal flap, finishing with the frontal incision; extensive freeing of the flap treating all the musculature responsible for skin cracking1,6,7 (Figure 7); resection of the skin segment; continuous suture. It is fundamental that Point B be returned to its original position, as already emphasized, to avoid a step, marking of Point A in the Peninsula; SMAS plication in the form of an anteriorized sickle.

Figure 7. Pre and postoperative of pre-capillary frontal peninsula. Focus on the lateral raising of the eyebrow and on the frontal and peninsula scar.
The suture consists of approximately 7 stitches made with colorless 4.0 nylon for anchorage, and with 5.0 nylon for continuous suture.
Hair fringes is the ideal hairstyle to cope with the scarring burden, although it is fully compensated by the satisfactory outcome of the technique (Figure 8).

Figure 8. Pre and postoperative temporal peninsula.
Demarcation of the Peninsula and the frontal pre-capillary incision (Figures 6 and 7): notice how important the irregularity of the zigzag incision is (Figure 6).
CONCLUSION
Therefore, as described above, one may conclude that the Peninsula technique is a unique resource, easily reproducible, capable of reducing the learning curve in rhytidoplasty, as it enables ample skin resection without interfering with hairline implantation. It does not require the creation of flaps for compensation. In addition, it avoids post-surgical stigma and optimizes the quality of the results leading to patient satisfaction, despite the slight scarring mentioned above.
It should be once again reinforced that the eventual presence of a previous scar does not mean a preclusion of the Peninsula procedure, and that this technique works well for primary and secondary cases.
COLLABORATIONS
RP Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents.
GHP Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents.
AKRT Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents.
CLS Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents.
REFERENCES
1. Pontes R. O Universo da Ritidoplastia. Rio de Janeiro: Revinter; 2011. p. 119-46.
2. Zide BM. Surgical anatomy around the orbit. Philadelphia: Lippincott Williams & Wilkins; 2006. p. 19-23.
3. Seckel BR. Zonas faciais de perigo: evitando a lesão de nervos em cirurgia plástica facial. 1a ed. Rio de Janeiro: Di Livros; 1998.
4. Rohrich RJ, Pessa JE. Facial topography: clinical anatomy of the face. St. Louis: Quality Medical Publishing; 2012. 216 p.
5. Larrabee Jr. WF, Makielski KH. Surgical anatomy of the face. New York: Raven Press; 1993.
6. Thiel W. Atlas fotográfico de anatomía práctica. Tomo II: Cabeza. Cuello. Tórax. Extremidad superior. Barcelona: Springer-Verlag Ibérica. 1999.
7. Netter FH. Atlas de anatomia humana. 2a ed. Porto Alegre: Artmed; 2000.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Niterói D'or, Niterói, RJ, Brazil
3. Universidade Federal Fluminense, Niterói, RJ, Brazil
4. Sociedade Internacional de Cirurgia Plástica Estética
5. American Society for Aesthetic Plastic Surgery
6. D'honneur de La Société Française de Chirurgie Esthétique
7. Federación Iberolatinoamericana de Cirugía Plástica
Institution: Hospital Niterói D'or, Niterói, RJ, Brazil.
Corresponding author:
Ronaldo Pontes
Av. Epitácio Pessoa, 846 - Ipanema
Rio de Janeiro, RJ, Brazil Zip Code 22410-090
E-mail: ronaldopontes@terra.com.br
Article received: March 13, 2016.
Article accepted: April 23, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter