

Original Article - Year 2017 - Volume 32 -
The medial plantar flap: a case series
Retalho plantar medial: uma série de casos
ABSTRACT
INTRODUCTION: Reconstructive coverage of foot defects, especially those of the calcaneus region, is a unique technical challenge for the surgeon due to the high degree of specialization of the tissues involved and the relative immobility of the proximal tissues.
METHODS: In the present study, we present our experience with the use of the flap based on the medial plantar artery to cover tissue defects in the foot, especially in the region of the calcaneal fat pad. Twelve medial plantar artery flaps constructed from 2001 to 2013 at the As a Norte Regional Hospital, Brasília, DF, were included.
RESULTS: Of the 12 patients with the medial plantar artery flaps, 10 were men and 2 were women. The indications were traumatic tissue loss of the plantar fat pad in 10 patients and of the dorsum of the foot in two cases. All flaps were elevated as fasciocutaneous pedicle flaps based on the medial plantar artery. All the flaps healed without major complications, except one case that involved partial loss . The donor area was covered with a partial skin graft and there was one case of partial graft loss. The flap displayed a slightly lower protective sensitivity than the normal side.
CONCLUSION: According to the results, the medial plantar flap is a good option for covering traumatic foot defects, especially those affecting the calcaneus. The versatility of the flap allows the coverage of defects of the calcaneus (e.g., the Achilles tendon and plantar fat pad regions), as well as those affecting the dorsum of the foot. The coverage of the plantar fat pad region with skin of similar texture and protective sensitivity confers to the medial plantar flap a large advantage over other flaps for reconstruction of this region.
Keywords: Calcaneus; Wounds and injuries; Reconstructive surgical procedures; Foot trauma.
RESUMO
INTRODUÇÃO: A cobertura do pé e especialmente da região do calcâneo são desafios técnicos para o cirurgião devido ao alto grau de especialização dos tecidos envolvidos e à relativa imobilidade dos tecidos próximos.
MÉTODOS: No presente estudo, apresentamos nossa experiência com uso do retalho baseado na artéria plantar medial para cobertura de defeitos teciduais no pé, especialmente na região de apoio plantar no calcâneo. Doze retalhos da artéria plantar medial feitos de 2001 a 2013 no Hospital Regional da Asa Norte, Brasília, DF, foram incluídos.
RESULTADOS: Dos 12 pacientes, 10 eram homens e dois eram mulheres. As indicações foram perda traumática do coxim do calcâneo em 10 pacientes e dorso do pé em dois casos. Todos os retalhos foram elevados como retalhos pediculados fasciocutâneos baseados na artéria plantar medial. Todos os retalhos cicatrizaram sem maiores complicações, exceto um caso com perda parcial. A área doadora foi coberta com enxerto de pele parcial e houve um caso de perda parcial do enxerto. Os retalhos apresentaram uma sensibilidade protetora levemente inferior ao lado normal.
CONCLUSÃO: De acordo com os resultados, o retalho plantar medial é uma boa opção para cobertura do pé, especialmente do calcâneo. A versatilidade do retalho permite a cobertura de defeitos no calcâneo sobre o tendão de Aquiles e apoio plantar, assim como o dorso do pé. A cobertura da região de apoio plantar com pele de textura similar e sensibilidade protetora confere a esse retalho uma grande vantagem sobre outros retalhos para reconstrução dessa região.
Palavras-chave: Calcâneo; Ferimentos e lesões; Procedimentos cirúrgicos reconstrutivos; Traumatismos do pé.
The reconstruction of the distal third of the lower limb is still a challenge for plastic surgeons. The anatomical characteristics, such as scarcity of tissues and skin, greatly hinder the treatment of soft tissue injuries in this location.
The use of fasciocutaneous flaps in the reconstruction of lesions of the distal third of the lower limb, especially of the foot, is well indicated due to similarities between the tissues of the region. The medial plantar island flap is one of the most important of these flaps1,2.
The medial plantar flap was initially described by Harrison and Morgan in 19813. It is based on the medial plantar artery and consists of a fasciocutaneous flap using the skin of the plantar arch of the foot, ideal tissue for covering defects in the region of the calcaneus and other regions of the foot due to their structural similarity. The innervation of this flap is preserved, which maintains sensitivity, an important protective factor4.
OBJECTIVE
The objective of this study is to present a series of cases involving patients with traumatic lesions of the foot who underwent surgical reconstruction with the medial plantar flap from 2001 to 2013.
METHODS
This is a retrospective study of all patients admitted to the plastic surgery service of a public hospital, who during the aforementioned period underwent reconstruction of limbs for loss of skin coverage using the medial plantar flap. The following variables were evaluated: gender, age, etiology of the trauma, presence and location of fractures, characteristics of the loss of substance, and presence of bone exposure.
The inclusion criteria were patients treated at the Plastic Surgery Service of the Asa Norte Regional Hospital in Brasília, DF, with lower limb trauma who underwent reconstruction with the medial plantar flap. All patients were evaluated with Doppler ultrasound of the arterial system of the foot. The dorsal artery of the foot and the posterior tibial artery were patent in all patients.
The exclusion criteria were hemodynamically unstable patients, and patients with lesions of the tibial nerve or with injury in the plantar donor area.
Only after the preparation of the recipient site was the defect measured and transferred to the donor site. The flap had to be slightly larger than the recipient area.
The study was approved by the Research Ethics Committee of the Secretary of State for Health of the Federal District (CAAE number: 47391715.6.0000.5553, opinion: 1.167.841).
RESULTS
During the study period, 12 patients with injuries generated by lower limb trauma who needed a medial plantar flap were treated to cover these lesions. These patients were admitted on an outpatient basis, after clinical/surgical control of their wounds was achieved by other specialties, such as orthopedic and/or general surgery. The mean age of the patients at the time of initial care was 32 years, ranging from 2 years to 53 years, with a predominance of the 20 to 29-year-old age group. There was a predominance of males, representing 83.3% of the sample (Figure 1).
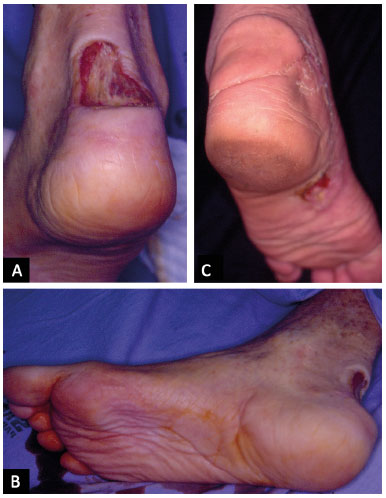
Figure 1. A: 53-year-old patient, victim of a motorcycle accident with loss of substance in the posterior region of the calcaneus; B: donor area of the flap; C: Medial plantar flap covering the Achilles tendon, 3 months after surgery.
Regarding the etiology of the traumas, the main cause was motorcycle accidents (50%), followed by run-over injuries (33.3%) and other motor vehicle accidents (16.7%). Regarding the location of the lesions, the predominant areas affected included the anterior calcaneus region (58.3%), the posterior calcaneus region near the Achilles tendon (25.0%), and the dorsum of the foot (16,7%). Regarding the presence of fractures, 83.3% of patients did not present with a fracture, while 16.7% suffered a metatarsal fracture (Figure 2). Bone exposure was present in 58.3% of patients and the other 41.7% presented with soft tissue loss without bone or tendon exposure. Regarding the surgical treatment, in 83.3% of the cases a medial plantar island flap was raised.
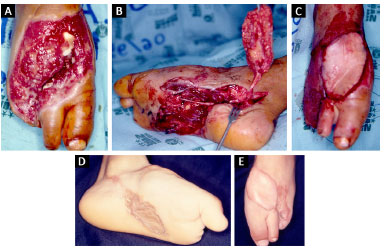
Figure 2. A: 5-year-old child, a victim of a run-over injury, with loss of substance on the dorsum of the foot with exposed metatarsal fracture; B: Medial plantar flap, in island, with its neurovascular pedicle; C: Flap positioned in the receiving area, on the dorsum of the foot; D: Donor area of the medial plantar flap with skin graft, 4 months postoperatively; E: Flap positioned on the dorsum of the foot, 4 months postoperatively.
In all cases, partial skin grafting was performed in the donor area, at the same surgical time. Surgical complications included partial loss of the skin graft in 1 case (8.3%) and partial loss of the flap in 1 case (8.3%). In the latter case, a reverse flow sural fasciocutaneous flap was performed subsequently, without intercurrences. In the other cases, use of the medial plantar flap was adequate to cover the lesion, allowing good aesthetic and functional results (Figures 1 to 5). Cutaneous sensation was preserved in every flap. No dysesthesia was detected.
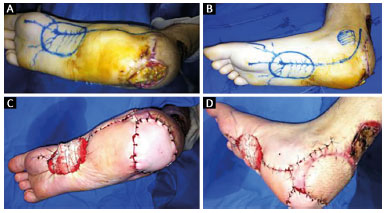
Figure 3. A: 26-year-old patient, victim of a motorcycle accident, with loss of calcaneal substance; B: Marking of the donor area of the medial plantar flap; C: Immediate postoperative positioning of the medial plantar flap in the calcaneus area; D: Lateral view of the reconstruction of the calcaneus with the medial plantar flap.
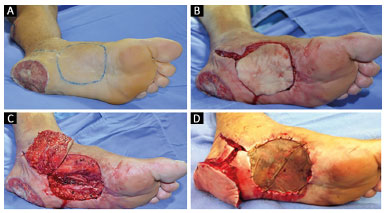
Figure 4. A: 35-year-old patient, victim of an automobile accident, with loss of calcaneal substance; B: Marking of the medial plantar flap in the donor area; C: Mobilization of the medial plantar flap of the donor area; D: Placement of the medial plantar flap in the recipient area and partial skin graft in the donor area.
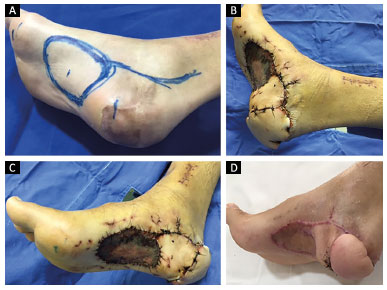
Figure 5. A: 31-year-old patient, victim of a motorcycle accident, marking of the medial plantar flap for reconstruction of the calcaneus; B: 7 days after placement of the medial plantar flap in the area of the calcaneus; C: View of the partial skin graft in the donor area of the medial plantar flap on the 7th postoperative day; D: Appearance of the reconstruction 4 months postoperatively.
DISCUSSION
The first choice for reconstruction of the plantar and calcaneal region of the foot should be the use of fasciocutaneous flaps. The medial plantar flap is a good option, as it provides a resistant skin covering with a similar appearance since it is a regional flap5. This allows "like tissue" to be manipulated with "like reconstruction," e.g., using glabrous skin with a fat pad and fibrous septae fixing skin resistant to shear and support trauma to the reconstruction area5,6.
The medial plantar flap is relatively easy to execute and is widely versatile, based on a well-defined pattern of vascular anatomy7. This flap has even been used in patients with diabetes mellitus8.
As for the reconstruction of soft parts of the calcaneus, it is important, from a practical point of view, that it be divided into a region exposed to weight (i.e., the anterior or plantar region) and a region not exposed to weight (i.e., the posterior region, on the Achilles tendon)9. The skin of the heel and plantar arch of the foot has the same characteristics; thus, this is the main reason for the preferential use of the medial plantar flap for lesions of the anterior region of the calcaneus.
An additional very important point is that this flap is innervated by the cutaneous branch of the medial plantar nerve that confers sensitivity, which is important for the ambulation of the patient. The flap is created slightly larger than or as the same size as the defect, as there is no significant primary contraction of the flap due to its specific fibroadipose characteristics.
The medial plantar flap has also been indicated for patients with diabetic neuropathy with chronic ulcers in areas of low sensitivity, demonstrating a low long-term recurrence rate of ulcers. As diabetic patients may have vascular problems, this flap is only indicated for diabetic patients with good vascular flow to the flap region8.
Locoregional fasciocutaneous flaps offer an alternative to free flaps for lower limb reconstruction, especially for the calcaneus. Free flaps would be indicated for more complex cases when none of the locoregional flaps are available9. Microsurgery may require longer surgical time than locoregional flaps and requires a specialized team10.
In calcaneal reconstructions, the reverse sural flap is also a good alternative11,12. This flap was successfully used in a case of partial loss of the medial plantar flap in the reconstruction of the calcaneus. The disadvantage of the reverse sural flap is the loss of sensation in the lateral malleolus, the lateral aspect of the foot, and fifth toe due to ligation of the sural nerve.
In this study, distal-based reverse flow flaps of the medial plantar artery were not used. This type of flap is indicated for the reconstruction of distal defects of the plantar region, in the area of the metatarsal heads. These flaps are based on retrograde blood flow from the distal medial plantar artery to the dorsal artery of the foot by communicating vessels from the first dorsal metatarsals. The disadvantage of this flap is its deficiency in sensitivity13.
The free flaps based on the medial plantar artery are also a good option for reconstruction of defects in the distal plantar region and may be innervated14,15. Moreover, the medial plantar flap can be used with the donor area of a flap from the opposite foot16.
The division of the posterior tibial artery into the plantar and lateral medial arteries occurs in the medial retromaleolar space, approximately 3 cm distal to the top of the medial malleolus. The medial plantar artery is usually of lower caliber than the lateral plantar artery (81% of cases), but can have higher caliber (3% of cases) or the same caliber (16% of the cases)5.
After emerging from the posterior tibial artery, the medial plantar artery enters the plantar compartment under the abductor muscle of the hallux. Below this muscle, at the height of the talonavicular joint, the medial plantar artery (MPA) presents three branching patterns: 1) Type A (54%), with the MPA dividing into two branches, exhibiting predominance of the superficial branch; 2) Type B (38%), with absence of a deep branch and the MPA remains a single artery (i.e., the superficial MPA); and 3) Type C (9%), with a calibrous deep branch reaching the hallux and a less calibrous superficial branch5. The superficial branch of the medial plantar artery continues distally in the muscular septum between the abductor muscle of the hallux and the short flexor of the toes. About three to four septocutaneous branches are directed to nourish the skin of the region, thus forming the anatomical basis of the medial plantar flap5-7.
One disadvantage of the flap based on the medial plantar artery is the sacrifice of an artery of the foot. However, the main plantar irrigation arch of the foot is the deep arch, which is formed mainly by the lateral plantar artery, which provides the formation of an anastomotic network between the two main arteries of the foot (the dorsal artery of the foot and the lateral plantar artery)17.
The deep plantar arch also gives rise to four plantar metatarsal arteries and some perforating arteries. The contribution of the medial plantar artery to the deep plantar arch is small and limited to the lateral branch of its deep branch17.
Another disadvantage of the medial plantar flap are its limitations in size and filling of deep defects and extensive cavities. Therefore, larger muscle or fasciocutaneous flaps should be used to cover such defects.
The reconstruction alternatives of complex lesions are numerous, but it is important to have adequate surgical planning which depends on the age, the gender, and the profession of the patient. In addition, the size and location of tissue loss must be considered. Furthermore, we should not forget the presence of associated trauma and injuries, especially in traumas caused by high-energy impact. There is a growing concern with the donor area and the quality of the results in the recipient area.
Regardless of the flap used in the reconstruction of limbs, its application should be performed as early as possible, since success is not exclusively associated with the success rate of the flaps, but also with the joint mobility of the limbs, the resumption of normal gait, and finally, with the return of the patient to work.
CONCLUSION
The medial plantar flap has proved to be a good option for treatment of wounds of the calcaneus and dorsum of the foot, leading to a low percentage rate of complications.
COLLABORATIONS
JLSM Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
SCR Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
AVRFN Analysis and/or interpretation of data; final approval of the manuscript; completion of surgeries and/or experiments.
AAS Final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments.
ACSA Final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments. IMB Final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments.
REFERENCES
1. Martins GB, Moreira AA, Viana FO. Reconstrução de lesões de partes moles do calcanhar com uso de retalhos fasciocutâneos. Rev Bras Cir Plast. 2009;24(1):104-9.
2. Benito-Ruiz J, Yoon T, Guisantes-Pintos E, Monner J, Serra-Renom JM. Reconstruction of soft-tissue defects of the heel with local fasciocutaneous flaps. Ann Plast Surg. 2004;52(4):380-4. PMID: 15084883 DOI: http://dx.doi.org/10.1097/01.sap.0000105520.24063.bb
3. Harrison DH, Morgan BD. The instep island flap to resurface plantar defects. Br J Plast Surg. 1981;34(3):315-8. PMID: 7272570 DOI: http://dx.doi.org/10.1016/0007-1226(81)90019-9
4. Mourougayan V. Medial plantar artery (instep flap) flap. Ann Plast Surg. 2006;56(2):160-3. PMID: 16432324 DOI: http://dx.doi.org/10.1097/01.sap.0000190830.71132.b8
5. Macchi V, Tiengo C, Porzionato A, Stecco C, Parenti A, Mazzoleni F, et al. Correlation between the course of the medial plantar artery and the morphology of the abductor hallucis muscle. Clin Anat. 2005;18(8):580-8. DOI: http://dx.doi.org/10.1002/ca.20147
6. FCAT, Federative Committee on Anatomical Terminology. Terminologia Anatomica- International Anatomical Terminology. Stuttgart: Thieme; 2011.
7. Rodriguez-Vegas M. Medialis pedis flap in the reconstruction of palmar skin defects of the digits: clarifying the anatomy of the medial plantar artery. Ann Plast Surg. 2014;72(5):542-52. DOI: http://dx.doi.org/10.1097/SAP.0b013e318268a901
8. Schwarz RJ, Negrini JF. Medial plantar artery island flap for heel reconstruction. Ann Plast Surg. 2006;57(6):658-61. DOI: http://dx.doi.org/10.1097/01.sap.0000235426.53175.e3
9. Barreiro GC, Batista RR, Busnardo F, Olivan M, Ferreira MC. Reconstrução de planta de pé de acordo com o conceito das subunidades anatômicas. Rev Bras Cir Plast. 2010;25(3 Suppl.1):81.
10. Siddiqi MA, Hafeez K, Cheema TA, Rashid HU. The medial plantar artery flap: a series of cases over 14 years. J Foot Ankle Surg. 2012;51(6):790-4. DOI: http://dx.doi.org/10.1053/j.jfas.2012.06.003
11. Garcia AMC. Retalho sural reverso para reconstrução distal da perna, tornozelo, calcanhar e do pé. Rev Bras Cir Plast. 2009;24(1):96-103.
12. Al-Qattan MM. The reverse sural fasciomusculocutaneous "mega-high" flap: a study of 20 consecutive flaps for lower-limb reconstruction. Ann Plast Surg. 2007;58(5):513-6. PMID: 17452835 DOI: http://dx.doi.org/10.1097/01.sap.0000244979.27265.d6
13. Coruh A. Distally based perforator medial plantar flap: a new flap for reconstruction of plantar forefoot defects. Ann Plast Surg. 2004;53(4):404-8. DOI: http://dx.doi.org/10.1097/01.sap.0000112287.56354.f8
14. Zelken JA, Lin CH. An Algorithm for Forefoot Reconstruction With the Innervated Free Medial Plantar Flap. Ann Plast Surg. 2016;76(2):221-6. DOI: http://dx.doi.org/10.1097/SAP.0000000000000564
15. Lykoudis EG, Seretis K, Lykissas MG. Free sensate medial plantar flap for contralateral plantar forefoot reconstruction with flap reinnervation using end-to-side neurorrhaphy: a case report and literature review. Microsurgery. 2013;33(3):227-31. DOI: http://dx.doi.org/10.1002/micr.22075
16. Acikel C, Celikoz B, Yuksel F, Ergun O. Various applications of the medial plantar flap to cover the defects of the plantar foot, posterior heel, and ankle. Ann Plast Surg. 2003;50(5):498-503. DOI: http://dx.doi.org/10.1097/01.SAP.0000044141.35292.A7
17. Ozer MA, Govsa F, Bilge O. Anatomic study of the deep plantar arch. Clin Anat. 2005;18(6):434-42. DOI: http://dx.doi.org/10.1002/ca.20126
1. Universidade de Brasília, Brasília, DF, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
3. Escola Superior de Ciências da Saúde, Brasília, DF, Brazil
4. Hospital Regional da Asa Norte, Brasília, DF, Brazil
Institution: Hospital Regional da Asa Norte, Brasília, DF, Brazil.
Corresponding author:
Jefferson Lessa Soares de Macedo
SQS 213, bloco H, Apto 104 - Asa Sul
Brasília, DF, Brazil Zip Code 70292-080
E-mail: jlsmacedo@yahoo.com.br
Article received: August 25, 2016.
Article accepted: February 21, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter