

Original Article - Year 2017 - Volume 32 -
The use of a microporous tape for fixing skin grafts
Fita microporosa para fixação de enxertos cutâneos
ABSTRACT
INTRODUCTION: Fixing a skin graft is essential to its integration in the recipient bed. The literature presents several fixation techniques. However, only few reports on the use of microporous tape are available. This study aims to demonstrate and promote the use of microporous tape in fixing skin grafts.
METHODS: A prospective study was performed from January 2014 to January 2016. In 40 patients, a sterilized microporous tape was used as an isolated method to fix skin grafts.
RESULTS: The use of skin graft immobilization showed satisfactory results and consequently good integration.
CONCLUSION: The use of a sterilized microporous tape is an excellent method for fixing skin grafts because it is easy, fast, and safe to use.
Keywords: Surgical tape; Skin transplantation; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A fixação do enxerto cutâneo é essencial para sua integração no leito receptor. A literatura apresenta várias técnicas de fixação, porém, o uso da fita de microporosa é pouco relatado. O objetivo é demonstrar e divulgar o uso da fita microporosa na fixação do enxerto cutâneo
MÉTODOS: Estudo prospectivo, realizado de janeiro de 2014 a janeiro de 2016. Em 40 pacientes foi utilizada a fita microporosa esterilizada como método isolado para a fixação do enxerto
RESULTADOS: Enxertos cutâneos apresentaram resultado satisfatório sem mobilização e, consequentemente, boa integração.
CONCLUSÃO: O uso da fita microporosa esterilizada é um excelente método para a fixação de enxertos cutâneos, por ser simples, rápido e seguro.
Palavras-chave: Fita cirúrgica; Transplante de pele; Procedimentos cirúrgicos reconstrutivos.
The skin, the largest organ of the human body, has important physical, chemical, microbiological, and thermal properties and is essential for the survival of an organism. Skin graft is the transfer of an unvascularized segment of the skin from a donor region to a recipient region. Any connection with the region of origin should be eliminated, and it must receive nutrition from the recipient bed1.
A recipient bed must be clean and vascularized and cannot be infected. These are the main factors for skin graft integration. However, fixing skin grafts is also essential to avoid its mobilization and contribute to its integration in the recipient bed2.
Based on the literature, several techniques, whether isolated or associated among themselves, are used to fix skin grafts, such as suturing, surgical staples, fibrin glue, and vacuum therapy3. However, the microporous tape technique that is used to fix skin grafts is not often cited in the literature.
OBJECTIVE
The present study aimed to demonstrate that the use of microporous tape is safe for fixing skin grafts in the recipient bed.
METHODS
Forty patients who needed autologous skin grafting were included in this prospective study conducted from January 2014 to January 2016. The sterilized microporous tape was used as an isolated method for fixing skin grafts.
This study was performed at the plastic surgery clinic of the Felício Rocho Hospital, Belo Horizonte, Minas Gerais (MG) according to the ethical principles of clinical research in humans by the World Medical Association Declaration of Helsinki revised in 2000. All patients signed the informed consent, thus authorizing the procedure and its inclusion in the study.
The related literature was obtained from the PubMed database. The authors declare no conflict of interest in the present study.
The inclusion criteria of the study were those patients to which were established favorable conditions of the recipient bed to skin grafting: bed granulation in good aspect; vascularized; without infections or collections; absence of foreign body; absence of devitalized tissues, and control of hemostasis. The exclusion criteria include conditions that are not favorable for local infections; foreign body; hematoma; tendon without paratenon; cartilage without perichondrium; bone without periosteum, and presence of devitalized tissues.
Surgical technique
A microporous tape that is sterilized in ethylene oxide was used for fixing skin grafts in raw areas, such as the lower limbs, with chronic ulcers after the excision of cutaneous tumors (Figure 1). Moreover, it was used for covering the donor area with skin flaps in post-traumatic wounds and burn patients. After obtaining a partial thickness skin graft, this was placed on the recipient bed of the surgical wound (Figure 2). The skin around the recipient bed was dried.

Figure 1. Raw area in the lateral distal topography of the left lower limb.

Figure 2. Partial thickness skin graft placed on the bed of the surgical wound
A thin layer of benzoin tincture was applied on the skin around the bed for better fixation of the tapes. The previously sterilized microporous tapes were pressed lightly on the skin graft, and their edges were glued on the skin around the recipient bed of the surgical wound, coapting edges of the skin grafts, and surgical wound edges (Figure 3). The compressive dressing was made of Vaseline gauze, dry gauze, and crepe.
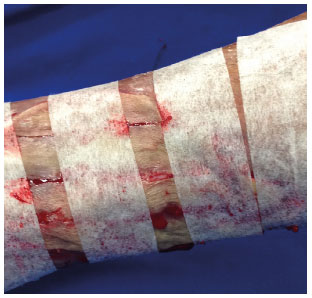
Figure 3. Sterilized microporous tapes lightly pressed on the skin graft, and its edges glued on the skin around the recipient bed of the surgical wound.
The first dressing change was performed on the fifth postoperative day, and the subsequent healing dressings were changed every other day. In general, the microporous tapes were removed from the fifth to seventh postoperative day. The patients were assessed based on the mobilization of skin graft in the recipient bed, fluid collected under the microporous tape, and pain associated with the withdrawal of the means of attachment (Figure 4).

Figure 4. Removal of microporous tape on the fifth day post-grafting with good fixation and integration.
RESULTS
In 39 patients who underwent skin grafting and fixation with sterilized microporous tape, good graft integration was obtained. We also observed a fast-surgical time, and the mobilization of skin grafts on the beds was not needed. Moreover, an absence of secretions under the microporous tape and during tape removal was noted, and none of the patients complained of pain or discomfort. However, one of the patients had pseudomonas infection in the grafted area, which inhibited graft integration.
The skin grafts performed using this method showed satisfactory results.
DISCUSSION
In the 1960s, Golden4 first described the development of a surgical tape designed for wound synthesis. After this study, Weisman5 (1961) used a microporous tape for other purposes, including skin grafting, with compelling and motivating results.
Previous studies conducted by Skoog6 (1963) and Gibson & Poate7 (1964) demonstrated the use of a special adhesive surgical tape (Steri-Strip®), which is highly recommended for wound approximation and closure. This sterile porous tape with polyester filaments is currently used with the same purpose and for extended graft fixation. However, it is costly.
Staple fixation was a fast and reliable method for graft fixation. However, it is expensive and not available at most hospitals, and patients often complain of pain during its removal8.
Fibrin glue and bandages with vacuum therapy are used to fix skin grafts. However, this method needs complex techniques compared with microporous tape for fixing skin grafts9,10.
Although a greater risk of graft mobilization in its recipient bed is observed, compressive dressing is a simpler method, thus promoting a lower integration degree11.
The use of sutures is the most commonly used technique in fixing a skin graft on the recipient bed. However, it causes a prolonged surgical time, and its process is laborious. Furthermore, it causes pain in patients during removal12.
The use of a microporous tape for fixing skin grafts was initially introduced in the 1960s. However, it is not used worldwide, despite its simple and effective implementation method (Figure 5).

Figure 5. Extensive raw area in the right lower limb: The skin graft is fixed with microporous tape.
CONCLUSION
The use of sterilized microporous tape is an excellent method for fixing skin grafts because it is easy, fast, and safe to use. In addition, it is made from low-cost materials available worldwide and considerably reduces the surgical time.
COLLABORATIONS
ACMA Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
NAP Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
AFSF Analysis and/or interpretation of data; completion of surgeries and/or experiments.
EHP Analysis and/or interpretation of data; statistical analyses.
RPLF Analysis and/or interpretation of data; completion of surgeries and/or experiments.
JCRRA Critical review of its contents.
REFERENCES
1. Mélega JM, Viterbo F, Mendes FH. Cirurgia Plástica: Os Princípios e a Atualidade. Rio de Janeiro: Guanabara Koogan; 2011.
2. Carreirão S. Cirurgia plástica: para formação do especialista. Rio de Janeiro: Atheneu; 2011.
3. Yenidünya OM, Ozdengil E, Emsen MI. Split-thickness skin graft fixation with surgical drape. Plast Reconstr Surg. 2000;106(6):1429-30. DOI: http://dx.doi.org/10.1097/00006534-200011000-00046
4. Golden T. Non-irritating, multipurpose surgical adhesive tape. Am J Surg. 1960;100:789-96. PMID: 13706489 DOI: http://dx.doi.org/10.1016/0002-9610(60)90429-3
5. Weisman PA. Microporous surgical tape in wound closure and skin grafting. Br J Plast Surg. 1963;16:379-86. PMID: 14077774 DOI: http://dx.doi.org/10.1016/S0007-1226(63)80142-3
6. Skoog T. Porous tape in wound closure, skin grafting and wound dressing. Acta Chir Scand. 1963;126:383-7. PMID: 14072320
7. Gibson EW, Poate WJ. The use of adhesive surgical tape in plastic surgery. Br J Plast Surg. 1964;17:265-70. PMID: 14191130 DOI: http://dx.doi.org/10.1016/S0007-1226(64)80042-4
8. Best T, Lobay G, Moysa G, Tredget E. A prospective randomized trial of absorbable staple fixation of skin grafts for burn wound coverage. J Trauma. 1995;38(6):915-9. PMID: 7602635 DOI: http://dx.doi.org/10.1097/00005373-199506000-00016
9. Buckley RC, Breazeale EE, Edmond JA, Brzezienski MA. A Simple preparation of autologous fibrin glue for skin-graft fixation. Plast Reconstr Surg. 1999;103(1):202-6. PMID: 9915185 DOI: http://dx.doi.org/10.1097/00006534-199901000-00033
10. Hoeller M, Schintler MV, Pfurtscheller K, Kamolz LP, Tripolt N, Trop M. A retrospective analysis of securing autologous split-thickness skin grafts with negative pressure wound therapy in paediatric burn patients. Burns. 2014;40(6):1116-20. PMID: 24438740 DOI: http://dx.doi.org/10.1016/j.burns.2013.12.007
11. Zanini M, Machado Filho CDAS, Timoner F. Uso de esponja cirúrgica para curativo compressivo de enxerto cutâneo. An Bras Dermatol. 2004;79(3):359-62. DOI: http://dx.doi.org/10.1590/S0365-05962004000300012
12. Gibran N, Luterman A, Herndon D, Lozano D, Greenhalgh DG, Grubbs L, et al.; FS 4IU Clinical Study Group. Comparison of fibrin sealant and staples for attaching split-thickness autologous sheet grafts in patients with deep partial- or full-thickness burn wounds: a phase 1/2 clinical study. J Burn Care Res. 2007;28(3):401-8. PMID: 17438504 DOI: http://dx.doi.org/10.1097/BCR.0B013E318053D389
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Monte Sinai, Juiz de Fora, MG, Brazil
3. Hospital e Maternidade Therezinha de Jesus, Juiz de Fora, MG, Brazil
4. Hospital Felício Rocho, Belo Horizonte, MG, Brazil
5. Instituto de Cirurgia Plástica Avançada, Belo Horizonte, MG, Brazil
6. Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brazil
7. Faculdade de Medicina da Universidade de Itaúna, Itaúna, MG, Brazil
Institution: Hospital Felício Rocho, Belo Horizonte, MG, Brazil.
Corresponding author:
Augusto César de Melo Almeida
Rua Ouro Preto, 617/1904 - Barro Preto
Belo Horizonte, MG, Brazil Zip Code 30170-040
E-mail: almeidaugusto@hotmail.com
Article received: October 30, 2016.
Article accepted: February 21, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter