

Original Article - Year 2017 - Volume 32 -
Neoomphaloplasty with cutaneous graft
Neo-onfaloplastia com enxerto cutâneo
ABSTRACT
INTRODUCTION: The umbilical scar is due to the fall of the umbilical stump that occurs a few days after birth. Its presence, shape, and location on the abdominal wall provide the individual with an aesthetic and sensual connotation.
METHODS: A primary prospective interventional study. The sample was of convenience, from February 2006 to June 2016, and included patients of both sexes attending the outpatient clinic of the Hospital das Clínicas of the Federal University of Pernambuco (HC-UFPE), a private clinic . The inclusion criteria were patients with abdominoplasty indications presenting with compromised circulation to the skin of the umbilical and periumbilical region caused by hernia defects in this area. The study followed the criteria of Helsinki and the patients signed an Informed Consent Form.
RESULTS: Twenty-eight patients underwent surgery and good integration of the grafted skin was observed. This resulted in an umbilical scar with a natural appearance and without complications.
CONCLUSIONS: Neoomphaloplasty with a cutaneous graft is easy to perform and, in the long term, has shown to provide good aesthetic results, especially in thick abdominal flaps, thus proving to be an additional technical option for neoomphaloplasty procedures.
Keywords: Navel; Abdominoplasty; Umbilical hernia; Abdomen; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A cicatriz umbilical é decorrente da queda do coto umbilical, que ocorre alguns dias após o nascimento. Sua presença, formato e localização na parede abdominal fornecem ao indivíduo uma conotação estética e sensual.
MÉTODOS: Estudo primário, prospectivo, de intervenção. A casuística foi de conveniência, no período de fevereiro de 2006 a junho de 2016, incluindo pacientes de ambos os gêneros, alocados do ambulatório do Hospital das Clínicas da Universidade Federal de Pernambuco (HC-UFPE) e clínica privada. Os critérios de inclusão foram pacientes com indicação de abdominoplastia e que apresentavam um comprometimento da irrigação da pele da região umbilical e periumbilical devido a defeitos herniários da região. O estudo seguiu os critérios de Helsinki e os pacientes assinaram o Termo de Consentimento Livre e Esclarecido.
RESULTADOS: Foram operados 28 pacientes, sendo observada uma boa integração da pele enxertada, resultando em uma cicatriz umbilical de aparência natural e sem complicações.
CONCLUSÕES: A neo-onfaloplastia com enxerto cutâneo é de fácil execução e que, a longo prazo, tem demonstrado um bom resultado estético, principalmente nos retalhos abdominais espessos, demonstrando ser mais uma opção técnica na realização de neo-onfaloplastias.
Palavras-chave: Umbigo; Abdominoplastia; Hérnia umbilical; Abdome; Procedimentos cirúrgicos reconstrutivos.
The umbilical scar is due to the fall of the umbilical stump that occurs a few days after birth. The word navel derives from the Latin, umbilicus, which is the diminutive of umbo. It means rounded protrusion on a surface1. Its presence, shape, and location on the abdominal wall give the individual an aesthetic and sensual connotation2.
Concern with the aesthetics of the navel during abdominoplasty was first reported in the 1950s by Andrews and Vernon, who reconstructed or transposed it, performing circular incisions in the skin of the abdominal flap3-5. In Brazil, in 1975, Baroudi introduced a neoomphaloplasty technique that consisted of performing horizontal incisions in the flap while fixing it to the aponeurosis of the rectus abdominis muscle6. In 1990, in Japan, Matsuo described the first neoomphaloplasty procedure with a graft, in which he used a conchal cartilage graft7. In 2011, Pita et al.2 described a technique consisting of the association of cutaneous grafts from previously removed umbilical skin with an upper pedicle dermal flap.
In this study, a series of cases are described in which abdominoplasty was performed, associating a new technique known as neoomphaloplasty with a cutaneous graft without the association of the upper pedicle dermal flap.
OBJECTIVE
To present a technical option for the reconstruction of the umbilical scar in patients with umbilical hernias who have decreased circulation in this region and present with abdominoplasty indications.
METHODS
A primary prospective interventional study was performed. The sample was of convenience and 28 patients of both sexes underwent surgery between February 2006 to June 2016 at the outpatient clinic of the Hospital das Clínicas of the Federal University of Pernambuco (HC-UFPE), in Recife, PE, a private clinic. The inclusion criteria were patients with abdominoplasty indications and compromised circulation in the skin of the umbilical and periumbilical region due to hernia defects in this region (Figure 1). The study followed the criteria of Helsinki and the patients signed an Informed Consent Form.
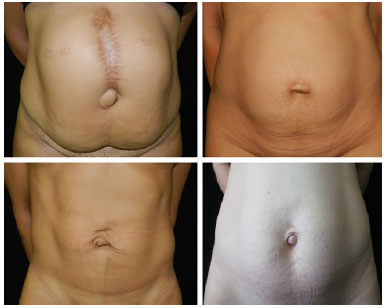
Figure 1. Pre-operative.
Surgical technique
After classic abdominoplasty is marked with the patient in the orthostatic position and then placed in dorsal decubitus, anesthetic blockade is performed. The surgery begins by marking a circle with bright green. On the skin, this measures approximately 1.5 cm in diameter and corresponds to the pre-existing umbilical scar in the abdominal flap. With a scalpel blade No. 15, the skin is resected with partial dermal thickness (Figure 2) and placed in a tank with saline solution for subsequent grafting.
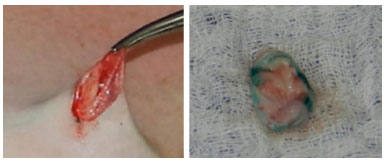
Figure 2. Umbilical scar skin.
A suprapubic incision of approximately 30 cm is performed, followed by supra-aponeurotic detachment of the abdominal wall flap from the pubis to the costal edge. Then, a traditional technique of abdominal dermolipectomy was carried out, which proceeded by closing the hernial ring and correcting the diastasis of the abdominal rectus with mononylon 2-0. Then, the new location of the umbilical scar was defined, which usually corresponds to the region of the intersection of the midline of the abdomen with a horizontal line connecting the anterior superior left iliac spine to the right, which is also marked with bright green.
The remaining skin of the umbilical scar is then perforated with a blade No 15 to facilitate the integration (handle) fixed in the region previously marked in the aponeurosis of the rectus abdominal muscles with 4-0 monocryl (Figure 3). Then, the new location of the umbilical scar is defined on the skin of the abdominal flap, which can be carried out by direct vision or with the aid of Pitanguy's forceps.
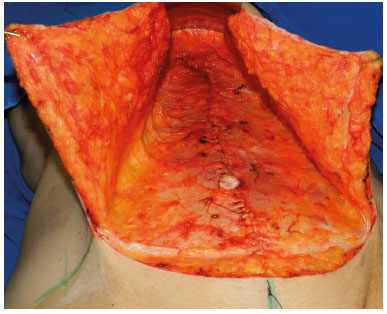
Figure 3. Umbilical scar skin graft.
After defining the new location, a diamond is drawn, approximately 0.5 cm distant from each edge. With scissors, the skin and subcutaneous tissue are then removed. Abdominoplasty is followed by the removal of the excess dermal-fat flap, fixation of the abdominal flap in the aponeurosis with Baroudi points, and suture of diamond edges of the abdominal wall to the graft using nylon 4-0 (Figure 4). Subsequently, the surgical wound is closed in each plane.

Figure 4. Immediate post-operative.
RESULTS
Twenty-eight patients underwent the surgery. A good integration of the grafted skin was observed, which resulted in an umbilical scar of natural appearance and without complications (Figure 5).
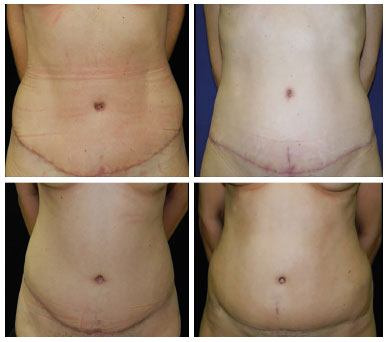
Figure 5. Late post-operative.
DISCUSSION
The first reports of umbilical reconstruction date back to the 1950s, with descriptions by Andrews and Vernon reconstructing or carrying out their transposition, and performing circular incisions on the skin of the abdominal flap3-5.
The use of grafts in performing neoomphaloplasty was first reported by Matsuo in 1990 in Japan, although this was a conchal cartilage graft7. Subsequently, in Brazil, in 2011, Pita et al. 2 described a technique consisting of the association of cutaneous grafts, from the umbilical skin previously removed, with a dermal flap of the upper pedicle. However, the authors modified the technique, eliminating the necessity of the dermal flap, with improvements in the final aesthetic result.
This neoomphaloplasty technique is easy to perform and can provide satisfactory aesthetic results. One of the reasons for its natural appearance is the use of local tissue as the graft donor area, applying one of the fundamental principles of reconstruction, namely the "like with like," which in Portuguese is "de igual para igual"8.
CONCLUSION
Neoomphaloplasty with a cutaneous graft is easy to perform and in the long term has shown to provide good aesthetic results, especially in thick abdominal flaps, demonstrating it is an option in performing neoomphaloplasty procedures.
COLLABORATIONS
PCCP Final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments.
RA Writing the manuscript or critical review of its contents.
JPM Writing the manuscript or critical review of its contents.
KK Writing the manuscript or critical review of its contents.
PSL Writing the manuscript or critical review of its contents.
REFERENCES
1. Ferreira ABH. Novo Dicionário Aurélio da Língua Portuguesa. 3a ed. Curitiba: Positivo; 2004.
2. Pita PCC, Lacerda AMR, Ferreira Filho JRA. Neo-onfaloplastia: técnica do enxerto da pele umbilical e retalho dérmico em "V" invertido. Apresentação de casos. Rev Bras Cir Plást. 2011;26(3 Suppl.1):78.
3. Ribeiro L, Muzy S, Accorsi A. Omphaloplasty. Ann Plast Surg. 1991;27(5):457-75. PMID: 1746865 DOI: http://dx.doi.org/10.1097/00000637-199111000-00008
4. Seung-Jun O, Thaller SR. Refinements in abdominoplasty. Clin Plast Surg. 2002;29(1):95-109. DOI: http://dx.doi.org/10.1016/S0094-1298(03)00088-9
5. Vernon S. Umbilical transplantation upward and abdominal contouring in lipectomy. Am J Surg. 1957;94(3):490-2. PMID: 13458618 DOI: http://dx.doi.org/10.1016/0002-9610(57)90807-3
6. Baroudi R. Umbilicoplasty. Clin Plast Surg. 1975;2(3):431-48.
7. Matsuo K, Kondoh S, Hirose T. A simple technique for reconstruction of the umbilicus, using a conchal cartilage composite graft. Plast Reconstr Surg. 199;86(1):149-51.
8. Southwell-Keely JP, Berry MG. Umbilical reconstruction: a review of techniques. J Plast Reconstr Aesthet Surg. 2011;64(6):803-8. PMID: 21145300 DOI: http://dx.doi.org/10.1016/j.bjps.2010.11.014
1. Faculdade de Medicina, Universidade Federal de Pernambuco, Recife, PE, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, Recife, PE, Brazil
3. Hospital Esperança, Recife, PE, Brazil
4. Hospital das Clínicas, Universidade Federal de Pernambuco, Recife, PE, Brazil
Institution: Hospital das Clínicas, Universidade Federal de Pernambuco, Recife, PE, Brazil.
Corresponding author:
Pedro Celso de Castro Pita
Rua Antônio Gomes de Freitas, 365 - Ilha do Leite
Recife, PE, Brazil Zip Code 50070-490
E-mail: pedro.pitta@hotmail.com
Article received: December 21, 2016.
Article accepted: February 21, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter