

Original Article - Year 2017 - Volume 32 - Issue 2
Pectus excavatum and breast asymmetry: correction with breast augmentation
Pectus excavatum e assimetrias mamárias: correção com mamoplastia de aumento
ABSTRACT
INTRODUCTION: Pectus excavatum is defined as a depression approaching the sternum and costal cartilages to the spine. Several theories explain its etiology, the most accepted of which is the exaggerated growth of the costal cartilages, which causes a posterior displacement of the sternum and consequent depression. The treatment includes correction of breast asymmetries by using silicone breast implants in patients without cardiopulmonary symptoms, only with esthetic complaints.
METHODS: We reviewed the medical and photographic records of eight female patients diagnosed as having pectus excavatum, who underwent operation at a private hospital in the southern region of Brazil. These women sought consultation for local esthetic complaints and had no cardiorespiratory complaints.
RESULTS: Six patients submitted only for breast prosthesis placement. One patient had a prosthesis implanted 15 years before, which was replaced by a new implant in the same plane. Another patient had undergone pectus repair with Nuss surgery 10 years before, and the patient came to the hospital with a complaint of hypomasty and asymmetry. The preferred anesthesia was general anesthesia in five of the cases. The prosthesis inclusion plane in almost all the cases was subglandular. Only one patient had a complication (seroma).
CONCLUSIONS: In our sample, the placement of breast prostheses in the patients with pectus excavatum brought harmonic esthetic results, attenuating and/or masking the chest defect, with satisfactory esthetic results for the patients.
Keywords: Breast implant; Breast; Mammaplasty; Reconstructive surgical procedure; Sunken chest.
RESUMO
INTRODUÇÃO: O pectus excavatum é definido com uma depressão aproximando o esterno e as cartilagens costais à coluna vertebral. Existem diversas teorias em relação à etiologia; a mais aceita consiste no crescimento exagerado das cartilagens costais, causando um deslocamento posterior do esterno e consequente depressão. Dentre as formas de tratamento, encontra-se a correção das assimetrias mamárias utilizando próteses mamárias de silicone em pacientes sem sintomas cardiopulmonares, apenas com queixa estética.
MÉTODOS: Foram revisados os registros em prontuários e registros fotográficos de oito casos de pacientes femininas com diagnóstico de pectus excavatum operadas em um hospital privado na região Sul do Brasil, que procuravam o serviço com queixas estéticas locais, e não apresentavam queixas cardiorrespiratórias.
RESULTADOS: Seis casos foram submetidos somente à inclusão de prótese mamária. Uma paciente havia colocado prótese havia 15 anos, sendo essa substituída por novo implante, no mesmo plano. Outra paciente já havia realizado cirurgia de correção de pectus descrito por Nuss, 10 anos antes, vindo a consulta com queixa de hipomastia e assimetria. O tipo anestésico preferido foi a anestesia geral, em cinco dos casos. O plano de inclusão de prótese na quase totalidade dos casos foi o subglandular. Somente uma paciente apresentou complicação (seroma).
CONCLUSÕES: Evidenciamos, na nossa amostra, que a inclusão de prótese mamária em pacientes com pectus excavatum é capaz de trazer resultados estético harmônicos, atenuando e/ou mascarando o defeito torácico, com resultados estéticos satisfatórios para os pacientes.
Palavras-chave: Implantes de mama; Mama; Mamoplastia; Procedimentos cirúrgicos reconstrutivos; Tórax em funil.
Congenital chest wall deformities involve various musculoskeletal defects that alter chest contour and symmetry. They are generally classified into the following five categories: Poland syndrome, pectus excavatum, pectus carinatum, cleft sternum, and skeletal cartilaginous dysplasias1. Pectus excavatum is the most common subtype, with an incidence of 1:300 to 1:1000 live births, affecting the male sex more, in a ratio of approximately 3:1, with the white race being more commonly affected2-4.
Pectus excavatum is defined as a depression approaching the sternum and costal cartilages to the spine. The most frequent alteration occurs in the medial region of the anterior thorax and involves half or two-thirds of the lower portion of the sternum5,6. The anatomical alteration is already present at birth, in a discrete way, increasing at the beginning of puberty and showing progressive growth until the adult stage7.
Several theories explain its etiology, the most accepted of which is the exaggerated growth of the costal cartilage, which causes a posterior displacement of the sternum and consequent depression. The mechanism of the chondral overgrowth remains unexplained, but the ossification centers of the sternum and histological appearance of the costal cartilages are known to be normal8,9.
Most patients do not have systemic repercussions, but in cases of severe deformity of the thoracic cavity with cardiac and/or lung compression, they may present dyspnea, fatigue, syncope, arrhythmia, heart palpitations, and tachycardia, triggered mainly by physical effort10. Psychological problems may also be present because of the distortion of body image, which leads to difficulty in social interactions. Esthetic complaints are the most common, especially in women, and surgeons must pay much attention to thoracic deformities associated with asymmetry of the breasts11-13.
The correction of the defects of pectus excavatum is surgical, and the techniques are divided into two groups. For patients with severe deformities and anatomical and physiological changes, the most common techniques are the Ravitch procedure14 (which consists of subperichondrial resection of the cartilages involved in the defect) and the Nuss procedure15 (which involves placement of a pectus bar in the posterior portion of the sternum). In the second group of patients, who had fewer esthetic complaints, local tissue flaps, silicone prosthesis, fat grafts, or combinations of these may be used, with satisfactory results and less postoperative morbidity16.
Of patients with only esthetic impairment, most prefer a resolution with lower morbidity. Our study retrospectively evaluated patients diagnosed with pectus excavatum without significant anatomical and physiological alterations, treated exclusively with the use of silicone breast implants, for local esthetic improvement.
OBJECTIVE
To describe cases of breast asymmetry correction by using silicone breast implants in female patients diagnosed with pectus excavatum who had no cardiopulmonary symptoms, only esthetic complaints.
METHODS
The study was based on a review of the medical records of female patients with a diagnosis of pectus excavatum operated in a private hospital in the Southern region of Brazil. Women who sought the service because of local esthetic complaints between July 2001 and January 2016 were evaluated. The patients had no cardiorespiratory complaints, only esthetic deformity and/or breast asymmetries.
Surgeries were performed under general anesthesia using antisepsis techniques and intravenous injection of cefazolin 1 g during anesthetic induction. Prosthesis placement was performed through an inframammary sulcus incision, through the subglandular or submuscular plane. In the latter, careful dissection was performed between the major and minor pectoral muscles, as there is an increased chance of pneumothorax due to thoracic deformities. Minimum lateral detachment was performed; it is important to position the prosthesis medially, further concealing the thoracic depression. Round, textured Mentor silicone breast implants were used.
During the preoperative consultation, the approximate size of the prosthesis was discussed with the patient, but the final choice was defined during surgery by using molds. The prosthesis cavity was bathed with antiseptic solution (iodine polvidine), and the breast implant was bathed with a solution containing antibiotics (kefazol and gentamicin). Drains were not used. Three planes of suture with 4-0 monocryl were performed for the closure of the surgical wound. The patients were discharged on the same day and returned to the consultation after 1 week. All the patients received transoperative antibiotic prophylaxis.
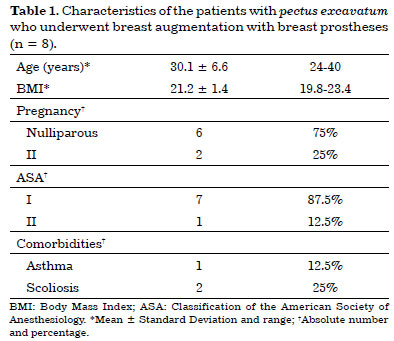
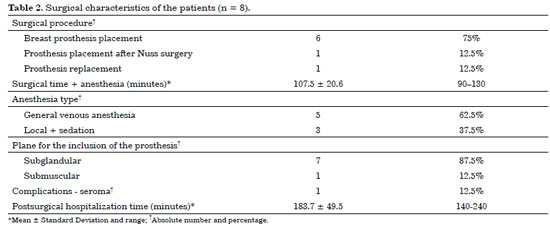
The following patient variables were analyzed: age (years), body mass index (BMI), number of pregnancies (pregnancy), and classification of the American Society of Anesthesiologists (ASA) and comorbidities; and with regard to surgery, the type of surgery (including breast augmentation, prosthesis placement after Nuss surgery, and prosthesis replacement), surgical and anesthetic times (minutes), type of anesthesia, plane for prosthesis placement, complications, length of hospitalization after surgery (minutes), and detailing of breast prostheses used (size and profile).
Statistical analysis was performed using SPSS (Statistical Package for the Social Sciences) version 19.0. Continuous variables were presented as mean and standard deviation, and categories as absolute number and percentage. The Student t test was used for comparison of means. A significance level (alpha) of 5% was adopted.
Regarding the ethical aspect of the work, we strictly followed the principles of the Declaration of Helsinki revised in 2000. The patients signed informed consent forms, allowing the use of their medical records and the publication of their images.
RESULTS
During the study period, we treated eight patients with clinical diagnosis of pectus excavatum. Their demographic characteristics are presented in table 1. The mean age was 30.1 ± 6.6 years (range, 24-40 years). All the patients had a BMI within the normal range, ranging from 19.8 to 23.4 kg/m2. Most (six, 75%) of the samples were nulliparous. Two patients had two sons. Regarding the American Society of Anesthesia classification, seven patients (87.5%) were classified as class I. With respect to comorbidities, one patient (12.5%) had asthma and two (25%) had scoliosis.
The characteristics of the procedures followed are presented in table 2. Six cases (75%) had breast prosthesis placement. One patient (12.5%) had a prosthesis 15 years ago, which was replaced by a new implant with greater volume in the same plane. One patient had undergone surgical correction of the pectus (Nuss) 10 years before seeking consultation for a complaint of hypomastia and asymmetry.
The mean length of time from induction, until the patient woke up, was 107.5 ± 20.6 minutes (range, 90-130 minutes). The longest procedure occurred when prostheses were placed in the submuscular plane in a patient who already underwent Nuss surgery. The anesthesia preferred was general anesthesia in five (62.5%) of the patients.
In almost all the cases (seven, 87.5%), the prostheses were placed in the subglandular plane. Only one patient (12.5%) presented with seroma as a complication. The mean (±SD) hospitalization time after surgery was 183.7 ± 49.5 minutes, and none of the patients was admitted more than 4 hours at the hospital.
Table 3 describes the volumetric data of each prosthesis. We can observe larger volumes, even if not statistically significant, to the right, where it is more common to present with chest depression. We observed a greater preponderance for ultra-high prostheses. Figure 1 shows an image of a patient diagnosed as having pectus excavatum who underwent augmentation mammoplasty for correction of the defect. The images are composed of preoperative, transoperative, and postoperative photographs.
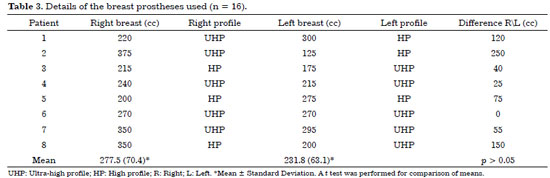

Figure 1. A patient with pectus excavatum who underwent augmentation mastoplasty. A and B: Preoperative frontal and oblique views; D and E: Postoperative frontal and oblique views; C and F: Transoperative lower view with a unilateral 240-cc prosthesis to the right, complementing that in F with a 215-cc prosthesis. Both had a super high profile in the subglandular plane.
Figure 2 shows the image of a patient who underwent surgical correction of the pectus (Nuss) 10 years before and had a complaint of hypomastia and asymmetry in the consultation. Breast augmentation in the retromuscular plane was used to correct the defect. Figure 3 shows the image of a patient with pectus excavatum and significant breast asymmetry treated with prostheses with a large volume difference (375 cc super high on the right and 125 cc high on the left) to mitigate the difference.

Figure 2. A patient who underwent Nuss surgery and after symmetrization with augmentation mastoplasty. A: Preoperative frontal view; B: Transoperative lower view with a silicone implant to the right, showing a thoracic deformity; C and D: Postoperative frontal and lower views. Placement of 270-cc silicone implants with a bilateral super -high profile in the retromuscular plane.
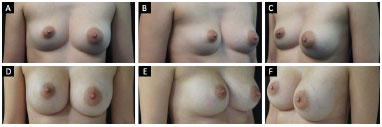
Figure 3. A patient with pectus excavatum who underwent symmetrization with a silicone prosthesis. A: Front view; B and C: Preoperative oblique view of the patient with pectus excavatum and significant breast asymmetry; D: Front view; E and F: Postoperative oblique view. In this case, 375-cc silicone implants were used: 125-cc super high profile (right) and high profile (left) in the subglandular plane.
DISCUSSION
A limited number of published studies evaluated women who received pectus excavatum esthetic correction surgery with silicone implants, although it is the most common congenital abnormality of the thoracic wall17. Breast asymmetry is the most common motivation for consultation of patients with pectus excavatum. They may also present with a retrosternal pain, easy tiredness, dyspnea, and palpitations, sometimes confused with emotional symptoms. There are several serious psychological alterations in these patients, including depression, anxiety, inferiority complex, shame in the practice of collective sports, body distortion, affective relationship difficulty, and social phobia, which lead to an important grievance in their life18,19.
The choice of surgical technique is tailored for each case. Patients with severe cardiac and/or pulmonary changes who develop dyspnea on exercise, palpitations, and chest pain related to pectus excavatum are candidates for costochondral reconstruction surgeries such as the Nuss and Ravitch procedures20.
The literature shows different treatment methods for patients with mild to moderate pectus excavatum and breast asymmetries without systemic consequences of the disease, such as silicone implants, fat grafts, or combinations of these procedures21. In this report, textured silicone breast implants were used with the inframammary incision access for placement of the prostheses, as already used by several authors, obtaining good results22-25.
The most common complication is seroma, which affected 65% of cases according to the literature, but with a much lower result in our work (12.5%)26. When the difference of the chest defect is greater than 3 cm between the sides, a prosthesis can be used to create a base for the breast implant. In our study, all the patients were treated with only one breast prosthesis for chest defect correction and breast asymmetry24.
CONCLUSION
Breast implants can be used to correct asymmetries in female patients with pectus excavatum who have no cardiopulmonary symptoms, only esthetic complaints. It is a simple, efficient, and safe procedure, with low postoperative morbidity and improved chest harmony, being a good treatment strategy.
COLLABORATIONS
PRSM Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
DOB Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
DFVA Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
DMS Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
REFERENCES
1. Park HJ, Gu JH, Jang JC, Dhong ES, Yoon ES. Correction of pectus excavatum with breast hypoplasia using simultaneous pectus bar procedure and augmentation mammoplasty. Ann Plast Surg. 2014;73(2):190-5. PMID: 23486122 DOI: http://dx.doi.org/10.1097/SAP.0b013e31826a1a93
2. Marks MW, Iacobucci J. Reconstruction of congenital chest wall deformities using solid silicone onlay prostheses. Chest Surg Clin N Am. 2000;10(2):341-55.
3. Spear SL, Pelletiere CV, Lee ES, Grotting JC. Anterior thoracic hypoplasia: a separate entity from Poland syndrome. Plast Reconstr Surg. 2004;113(1):69-77. DOI: http://dx.doi.org/10.1097/01.PRS.0000090727.07735.F5
4. Hodgkinson DJ. Anterior thoracic hypoplasia: a separate entity from Poland syndrome. Plast Reconstr Surg. 2005;115(3):960-1. DOI: http://dx.doi.org/10.1097/01.PRS.0000153805.22948.EC
5. Moriggl B, Kotzot D, Del Frari B, Schwabegger AH, Fatah F. Deformities of the anterior thoracic wall. In: Congenital Thoracic Wall Deformities. Vienna: Springer Vienna; 2011. p. 3-56. [acesso 2017 Abr 19]. Available from: http://link.springer.com/10.1007/978-3-211-99138-1_2
6. Margulis A, Sela M, Neuman R, Buller-Sharon A. Reconstruction of pectus excavatum with silicone implants. J Plast Reconstr Aesthet Surg. 2006;59(10):1082-6. PMID: 16996433 DOI: http://dx.doi.org/10.1016/j.bjps.2005.12.035
7. Snel BJ, Spronk CA, Werker PM, van der Lei B. Pectus excavatum reconstruction with silicone implants: long-term results and a review of the English-language literature. Ann Plast Surg. 2009;62(2):205-9. DOI: http://dx.doi.org/10.1097/SAP.0b013e31817d878c
8. Ravitch MM. Congenital Deformities of the Chest Wall and Their Operative Correction. Philadelphia: Saunders; 1977.
9. Haje SA, Harcke HT, Bowen JR. Growth disturbance of the sternum and pectus deformities: imaging studies and clinical correlation. Pediatr Radiol. 1999;29(5):334-41. PMID: 10382210 DOI: http://dx.doi.org/10.1007/s002470050602
10. Robicsek F. Surgical treatment of pectus excavatum. Chest Surg Clin N Am. 2000;10(2):277-96.
11. Beier JP, Weber PG, Reingruber B, Huemmer HP, Kneser U, Dragu A, et al. Aesthetic and functional correction of female, asymmetric funnel chest - a combined approach. Breast. 2009;18(1):60-5. DOI: http://dx.doi.org/10.1016/j.breast.2008.12.001
12. Kelly RE Jr, Cash TF, Shamberger RC, Mitchell KK, Mellins RB, Lawson ML, et al. Surgical repair of pectus excavatum markedly improves body image and perceived ability for physical activity: multicenter study. Pediatrics. 2008;122(6):1218-22. PMID: 19047237 DOI: http://dx.doi.org/10.1542/peds.2007-2723
13. Ravitch MM. The Operative Treatment of Pectus Excavatum. Ann Surg. 1949;129(4):429-44. PMID: 17859324 DOI: http://dx.doi.org/10.1097/00000658-194904000-00002
14. Nuss D, Kelly RE Jr, Croitoru DP, Katz ME. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg. 1998;33(4):545-52. DOI: http://dx.doi.org/10.1016/S0022-3468(98)90314-1
15. Bisbal Piazuelo J, De Barcia Valero JD. Pectus excavatum: aesthetic correction using customized implants. Cir Plást Iberolatinoam. 2010;36(4):345-53.
16. Rocha FP, Pires JA, Torres VF, Fagundes DJ. Treatment of bilateral mammary ptosis and pectus excavatum through the same incision in one surgical stage. Sao Paulo Med J. 2012;130(3):198-201. PMID: 22790553 DOI: http://dx.doi.org/10.1590/S1516-31802012000300010
17. Einsiedel E, Clausner A. Funnel chest. Psychological and psychosomatic aspects in children, youngsters, and young adults. J Cardiovasc Surg (Torino). 1999;40(5):733-6.
18. Haje SA, de Podestá Haje D. Orthopaedic approach to pectus deformities: 32 years of studies. Rev Bras Ortop. 2015;44(3):191-8. PMID: 27004171 DOI: http://dx.doi.org/10.1590/S0102-36162009000300003
19. Pinto EBS, Queiroz Filho W, Erazo P, Alves MAS, Wong LJ, Muniz AC. Pectus excavatum: Correção Cirúrgica Estética. Rev Bras Cir Plást. 1997;12(1):68-74.
20. Poupon M, Duteille F, Casanova D, Caye N, Magalon G, Pannier M. Le thorax en entonnoir: quelle prise en charge en chirurgie plastique? À propos de 10 cas. Ann Chir Plast Esthet. 2008;53(3):246-54. DOI: http://dx.doi.org/10.1016/j.anplas.2007.05.013
21. Carramaschi FR, Tanaka MP. Mastopexia Associada à Inclusão de Prótese Mamária. Rev Bras Cir Plást. 2003;18(1):26-36.
22. Johnson PE. Refining silicone implant correction of pectus excavatum through computed tomography. Plast Reconstr Surg. 1996;97(2):445-9. DOI: http://dx.doi.org/10.1097/00006534-199602000-00027
23. Hodgkinson DJ. The management of anterior chest wall deformity in patients presenting for breast augmentation. Plast Reconstr Surg. 2002;109(5):1714-23. DOI: http://dx.doi.org/10.1097/00006534-200204150-00039
24. Wechselberger G, Ohlbauer M, Haslinger J, Schoeller T, Bauer T, Piza-Katzer H. Silicone implant correction of pectus excavatum. Ann Plast Surg. 2001;47(5):489-93. PMID: 11716258 DOI: http://dx.doi.org/10.1097/00000637-200111000-00003
Hospital Universitário, Universidade Federal de Santa Catarina, Florianópolis, SC, Brazil
Institution: Hospital Universitário, Universidade Federal de Santa Catarina, Florianópolis, SC, Brazil.
Corresponding author:
Paulo Roberto da Silva Mendes
Rua Dom Joaquim, 885 - Centro
Florianópolis, SC, Brazil Zip Code 88015-310
E-mail: paulo@pmendesplastica.com
Article received: August 16, 2016.
Article accepted: February 21, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter