

Articles - Year 2003 - Volume 18 -
Zygomatic and Orbitozygomatic Fractures
Fraturas Zigomáticas e Orbitozigomáticas
ABSTRACT
Zygomatic fractures may cause major inconveniences for patients both functionally and esthetically Orbitozygomatic fractures are characterized chiefly by involvement of the orbit and they often lead to some ocular dysfunction. Zygotnatic fractures, on the other hand, correspond chiefly to damage to the zygoma with anatomic involvement of the orbit. With the objective of rationalizing the treatment of zygomatic fractures, this paper suggests a classification based on the experience of treating and following-up 148 cases for at least three months in the Instituto da Face, in São Paulo, Brazil. Etiology of the trauma,gender, age, direction of theforce vector, time after the fracture and the presence of functional changes were taken into consideration. Fractures were classified as type I (51 cases or 34%) type II (59 cases or 40%) and type III (38 cases or 26%). Type I fractures were treated with transcutaneous reduction, and 48 cases (94%) evolved with good projection of the zygoma. Fractures types II and III underwent direct reduction with visualization of the fracture line, and 55 cases (92%) and 34 cases (89.5%) evolved, respectively, with good projection of the zygoma.
Keywords: Zygomatic fractures; orbital fractures
RESUMO
As fraturas do zigoma podem produzir grandes transtornos para o paciente do ponto de vista funcional e estético. As fraturas denominadas orbitozigomáticas caracterizam-se pelo envolvimento primordial da órbita, sendo comum apresentar alguma disfunção ocular. Já as fraturas zigomáticas correspondem ao comprometimento principal do zigoma com o envolvimento anatômico da órbita. Com o objetivo de racionalizar o tratamento das fraturas de zigoma, este trabalho propõe uma classificação baseada na experiência de 148 casos tratados e preservados por um período mínimo de 3 meses no Instituto da Face, em São Paulo - Brasil. Foram levados em consideração a etiologia do trauma, o sexo, a faixa etária, a direção do vetor de força, o tempo decorrido após a fratura e a presença de alguma alteração funcional. As fraturas foram classificadas como tipo I (51 casos ou 34%), tipo II (59 casos ou 40%) e tipo III (38 casos ou 26%). As do tipo I foram tratadas através de uma redução transcutânea, sendo que em 48 casos (94%) evoluíram com boa projeção do zigoma. As dos tipos II e III tiveram redução direta com visualização dos traços de fratura e evoluíram, respectivamente, com 55 casos (92%) e 34 casos (89,5%) com uma boa projeção do zigoma.
Palavras-chave: Fraturas do zigoma; fraturas da órbita
The zygoma, due to its prominent position on the face, often suffers trauma, and, after the nose, it is the facial bone structure that is most likely to suffer fractures. It is a pyramidal bone that has a robust body with four processes: the frontosphenoidal, orbital, maxillary, and temporal. These processes are the zygoma's points of weakness, and often they are simply separated at the bone sutures with which they bond, as Barros and Manganello stated in 2000(1) (Figs. 1a-b).

Fig. 1a - Relation of the zygoma with adjacent anatomical structures (anterior view): 1) infraorbital foramen; 2) maxillozygomatic suture; 3) frontozygomatic suture; 4) infraorbital margin; 5) zygomatic
pillar; 6) zygomatic body; 7) maxillary sinus.

Fig. 1b - Relation of the zygoma with adjacent anatomical structures (lateral view): 1) temporozygomatic suture.
The decision whether to treat zygomatic fractures through open or closed reduction still leads to much doubt and controversy among surgeons. That is due to the fact that all of the existing classifications, including the best known-by Knight and North in 1961(2)- fail to provide concrete bases to determine the most suitable type of treatment, and there are surgeons who categorically contraindicate closed reduction.
An open reduction followed by rigid internal fixation provides greater safety and stability, reduces postoperative complications, and enables patients to quickly resume their functions. Klotch and Gilliland in 1987(3), Marciani in 1993(4), Sands et al. in 1993(5),highlighted the advantages of rigid internal fixation, especially for midface fractures, including the zygoma.
A study conducted by Kim in 1998(6), indicated the closed reduction with external fixation for 46 out of 124 patients with fractures to the zygomatic bone. For this author, the key requirements for its indication were the degree of bone displacement and presence or absence of comminution.
Rowe and Willians, in 1994(7), said that the insertion of the fascia of the temporal muscle into the zygomatic arch and in the zygoma itself exerts a force along the same line, but in the opposite direction, which neutralizes the traction of the masseter. It is important to recognize these forces and their role in the zygoma's stability after the reduction of the fracture based on its displacement.
The time elapsed after the trauma is another factor that deserves attention in the indication of the best treatment. Carr and Mathog, in 1997(8), found that in orbitozygomatic fractures it is possible, generaliy speaking, to get a primary reduction within 21 days after the trauma. Afterwards, they say osteotomies might be reguired, in addition to apposition bone grafts.
Zygomatic and orbitozygomatic fractures are the target of our work, along with suggesting a classification for them that enables surgeons to rationalize treatment in the most suitable manner.
PATIENTS AND METHODS
Between January 1995 and April 2002, 148 patients with zygomatic fractures were treated and followed up for at least three months in the Instituto da Face, in São Paulo, Brazil. The first requirement taken into account was that all fractures needed treatment due to facial asymmetry, functional changes, or the combination of both. The fractures visible in radiographic images without any clinical implications, that is, that did not need treatment, were not considered. Fractures affecting only the zygomatic arch without displacement of the zygoma should be treated alone, and for that reason they were not included in this study either.
As to the division between genders, 84% of the patients were male and 16% female, with a ratio of 5:1 respectively. Ages ranged from 3 to 69 yeas, with an average of 36 years. 75.5% of the patients were in the third or fourth decades of their lives. The most frequent etiological agents included: 41% of the frac tures resulted from physical aggression (punches, kicks, etc.), 38% of them resulted from traffic accidents, 17% from sport or occupational accidents, and 4% from perforations by fire weapons. Traffic accidents were divided as follows: 36% ear accidents, 32% run over by ears, 23% accidents with motorcycles, and 9% falls from bicycles. Based on the history of the trauma, we tried to relate the etiologieal agem with the direetion of the foree vector that caused the fracture, classifying them as either frontal or lateral.
As to the time elapsed after the trauma, fractures were divided into three graups: up to 20 days, 97 cases (66%), from 20 to 30 days, with 23 cases (15%), and more than 30 days, with 28 cases (19%).
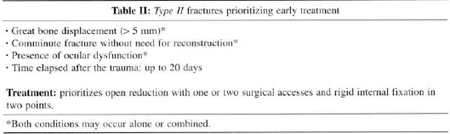
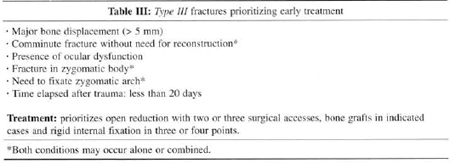
Considering all aspects mentioned above, fractures were classified as zygomatic (type I or type II) and orbitozygomatic (type III) (Tables I, II and III).
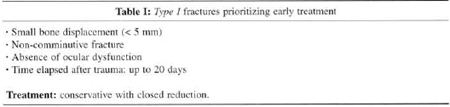
Type I fractures necessarily presented a small displacement of the zygoma, absence of ocular dysfunction and did not cause comminution (Figs. 2a-b). We defined a small displacement as a disjunction not greater than 5 mm on the fracture site. The fact that the zygoma rotated medially or laterally did not matter, but rather the magnitude of that displacement, and the presence or absence of ocular dysfunction. These fractures were treated in a conserva tive fashion through transcutaneous reduction and fixation with Kirschner thread for a period of 20 days.

Fig. 2a - TYPE I Fracture (anterior view): 1) fracture line going through infraorbital foramen; 2) broken zygomatic pillar; 3) uneven infraorbital margin; 4) small disjunction on frontozygomatic suture.

Fig. 2b - TYPE I Fracture (lateral view): 1) uneven infraorbital margin; 2) retro-positioning of zygomatic body; 3) disjunction on temporozygomatic suture; 4) small disjunction on frontozygomatic suture.
Type II fractures presented a signifIcant displacement of the zygoma (causing a disjunction greater than 5 mm between the fractured stumps on the frontozygomatic or maxillozygomatic sutures, regardless of the direction of the displacement), some degree of comminution without the need to reconstruct (anatomical reduction is more difficult if it is closed), or the presence of ocular dysfunction diagnosed in the absence of edema. These factors did not have to occur simultaneously, it was enough for one of them to be present for the fracture to be classified as type II (Figs. 3a-b). In these cases the treatment provided prioritized a reduction with direct visualization of the fracture line, using one or two surgical accesses and rigid internal fixation with mini-plates combined with 2.0 mm diameter screws in two points. If the internal fixation was done with steel thread, three points had to be fixated.

Fig. 3a - TYPE II Fracture (anterior view): 1) fracture line going through infraorbital foramen; 2) continuity solution on zygomatic pillar; 3) fracture on infraorbital margin; 4) large disjunction
on fromozygomatic suture.

Fig. 3b - TYFE II Fracture (lateral view): 1) fracture on infraorbital margin; 2) retro-positioning of zygomatic body; 3) small disjunction on temporozygomatic suture; 4) disjunction on frontozygomatic surure.
Type III fractures are called orbitozygomatic and differ from type II because they present the need for reconstruction of the orbit (usually the floor, due to loss of bone substance), fracture line on the zygomatic body, or the need to fixate the zygomatic arch due to intermediary fragments (Figs. 4a-b). Treatment consisted of rigid internal fixation in three or four points, depending on the need to fixate the zygomatic arch, with two or three surgical accesses. In cases that needed reconstruction, we used autogenous bone grafts from the skull, iliac crest or anterior wall of the maxillary sinus.

Fig. 4a - TYPE III Fracture (anterior view): 1) great loss of substance on orbital floor; 2) fragmems of orbital floor inside maxillary sinus; 3) dystopia.

Fig. 4b - TYPE III Fracture (lateral view): 1) fracture on infraorbital margin; 2) major retro-positioning of zygoma; 3) fracture with intermediary fragmem on zygomatic arch; 4) disjunction on frontozygomatic suture.
RESULTS
Type I fractures accounted for a total 51 cases (34%), type II yielded 59 cases (40%) and type III) 38 cases (26%). Among type III fractures, 26 cases (68.5%) needed reconstruction of the orbital floor.
As to the direction of the force vector that caused the fracture, 78% of type I fractures and 71.5% of type II fractures were caused laterally, and both were more related to physical aggression. On the other hand, in 79% of type III fractures, the direction of the trauma was frontal, and they were chiefly related to car accidents.
Forty-eight cases (94%) of type I fractures treated conservatively evolved with good projection of the zygoma when compared with the non-fractured opposite side. Among type II fractures, 55 cases (92%) had a good zygomatic projection without ocular dysfunction. Of type II fractures, 4 cases (8%) evolved with dystopia, and in 2 cases (4%) it was associated to diplopia and patients had to be operated again. 34 cases (89.5%) of type III fractures presented a good postoperative projection of the zygoma, and in 4 cases (10.5%) enophthalmos was detected in combination with dystopia and, in 3 of those cases (7.9%), there was also diplopia and patients had to undergo a new intervention.
DISCUSSION
Due to the anatomical relation of the zygoma and the orbit, it is necessary to differentiate the fractures that affect these structures in two types: orbitozygomatic and zygomatic. The first type is chiefly characterized by the involvement of the orbit, and often there is some ocular dysfunction such as diplopia, dystopia or enophthalmos. In these cases, treatment consists of repositioning the zygoma and reconstructing the orbit when necessary. In the second type, on the other hand, the principal structure involved is the zygomatic bone, with anatomical injuries to the orbital floor or lateral wall, and there could also be ocular dysfunction without need for reconstruction.
The zygomatic arch is important for keeping the antero-posterior projection of the zygoma; therefore, when there is a fracture of the zygomatic bone associated with a fracture or even bulging of the zygomatic arch, it is fundamental to reduce it correctly and, if necessary to fixate it.
We assumed that in fractures up to 20 days old, the amount of fibrosis formed does not affect bone mobilization and reduction. As the formation of fibrosis varies from one individual to the other, in fractures between 21 and 30 days old it may be difficult to perform the correct reduction, and sometimes, a fracture that would initially be treated with closed reduction, is indicated for open reduction. Fractures older than 30 days are considered sequelae and it is necessary to re-fracture the bone, conduct osteotomies, and sometimes even use grafts or inclusions.
Ocular dysfunction research must be very well directed and always conducted after the total regression of the edema, as it may mask this procedure. When there is zygomatic fracture combined with enophthalmos, dystopia, diplopia or association of both, open surgical treatment with exploration of the affected orbital walls will always be indicated.
When we compare the findings of this paper with those published in the literature on etiological agents, prevalence between genders and age, we noted that, generally speaking, the statistical percentages published by authors are equivalent, which is clear in Bataineh's studies in 1998(9).
Kim, in 1998(6), indicated transcutaneous reduction for 46 out of 124 cases of zygomatic fractures. Several authors prioritized this treatment approach to deal with a non-comminute fracture with small displacement(10-12).In our opinion, this conservative treatment approach presented several advantages such as, principally, the reduction of surgical time and the fact that it does not generally require the hospitalization of patients; however, ocular dysfunctions must be absent, and no more than 20 days should have elapsed after the trauma.
When Knight and North(2) published their classification of fractures of the zygomatic complex in 1961, they said that those that had medial rotation become unstable after reduction, and, therefore, a direct approach would be a good indication in these cases. In our view, it is not whether the displacement is medial or lateral that determines the best treatment approach, but rather, it is the amplitude of the displacement that is relevant. This classification(2), although didactically very good in order for us to understand the most likely possibilities of tridimensional zygomatic displacement, does not determine with certainty the best type of treatment for each one of its groups. Manganello et al., in 1982(13), modified this classification, removing group I, because, besides behaving like facial injuries, they are difficult to diagnose. They also removed group II, fractures of the zygomatic arch, because, as we have seen, they are a different entity.
The time elapsed after the trauma is a crucial condition to define treatment(8), and in fractures that are older than 20 days, reduction with direct visualization of the fracture line is always a very good indication.
In the event of a zygomatic fracture with presence of diplopia, dystopia or enophthalmos, the exploration of the orbital floor is always necessary(14), even if ir is a fracture with a small displacement, that is, with a disjunction smaller than 5 mm. In these cases it is unlikely that the ocular dysfunction may be corrected only with closed reduction.
Several classifications have been suggested for zygomatic fractures(8,13,15-17)however, we found that more importance has been placed on the image diagnosis of the fracture than on its resulting clinical signs and symptoms. We must understand that in the presence of any functional change, treatment cannot be limited to restoring facial esthetics and symmetry through the reduction and containment of the fracture, and, for that reason, clinical aspects must also be considered to classify zygomatic fractures.
CONCLUSION
Zygomatic fractures could be divided as to their seriousness in type I(34%), type II (46%) and type III (26%). Treatment is more complex depending on how serious the fracture is. Type I fractures were treated with transcutaneous reduction and fixation with Kirschner suture. Type II were treated through one or two surgical accesses with rigid internal fixation in two points or semi-rigid in three points. Type III fractures were treated with the use of two or three surgical accesses with rigid internal fixation in three or four points, depending on the need to fixate the zygomatic arch, with autogenous bone grafts in the indicated cases.
REFERENCES
1. Barros JJ, Manganello LCS. Fraturas do complexo zigomático. In: Traumatismo bucomaxilofacial. 2. ed. São Paulo: Roca; 2000. p. 357-72.
2. Knight JS, North JF. The classification of malar fractures: an analysis of displacement as a guide to treatment. British J ofPlast Surg. 1961; 13:325-39.
3. Klotch DW, Gilliland R. Internal fixation Vs conventional therapy in midface fractures. J Trauma. 1987; 27:1136-45.
4. Marciani RD. Management of midface fractures: fifty years later. J Oral Maxillofac Surg. 1993; 51:960-8.
5. Sands T, Symington 0, Katsikeris N, Brown A. Fractures of the zigomatic complex: a case reportand review. J Can Dent Assoe. 1993; 59:749-55.
6. Kim YO. Transcutaneous reduction and external fixation for the treatment o Noncomminuted zygoma fractures. J Oral Maxillofac Surg. 1998; 56:1382-7.
7. Rowe NL, Williams JL (ed). Fractures of the zygomatic complex and orbit. In: Maxillofacial injuries. Livingstone Churchill, 1994. p. 475-90.
8. Carr RM, Mathog RH. Early and delayed repair of orbitozygomatic complex fractures. J Oral Maxillofac Surg. 1997; 55:253-8.
9. Etiology and incidence of maxillofacial fractures in the north of Jordan. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86(1):31-5.
10. Kaastad E, Freng A. Zygomatico-maxillary fractures. Late results after traction-hook reduction. J Craniomaxillofac Surg. 1989; 17:210-4.
11. Stassen LF, Moos KF, El-Attar A. A comparison of the use of external pin and transnasal Kirschner wire fixation for the unstable tripod malar fractures: a prospective trial. J Oral Maxillofac Surg. 1989; 27:99-106.
12. Vriens JP, Van Der Glas HW, Moos KF, Koole R. Infraorbital nerve function following treatment orbitozygomatic complex fractures. A multitest approach. Int J Oral Maxillofac Surg. 1998; 27:27-32.
13. Manganello LCS, Soares CR, Santos LCB.Fraturas do malar: diagnóstico e tratamento. Rev Ass Paul Cirur Dent. 1982; 36:100.
14. Stanley RB, Sires BS, Funk GF, Nerad JA. Management of displaced lateral orbital wall fractures associated with visual and ocular motility disturbances. Plast Reconstr Surg. 1998; 102:972-9.
15. Laine FI, Conway WF, Laskim DM. Radiology of maxillofacial trauma. Curr Probl Diagn Radiol. 1993; 22:145-88.
16. Tarabichi M. Transsinus reduction and one-point fixation of malar fractures. Arch Otolaryngol Head Neck Surg. 1994; 120:620-5.
17. Zingg M, Laedrach K, Chen J, Chowdhury K, Vuillemin T, Sutter F, Raveh J. Classification and treatment of zygomatic fractures: a review of 1.025 cases. J Oral Maxillofac Surg. 1992; 50:778-90.
I - Bucomaxillofacial Surgeon. Plastic Surgeon.
II - Bucomaxillofacial Surgeon. Candidate member to the Brazilian College of Surgeons and Bucomaxillofacial Traumatology.
Study conducted at the Instituto da Face
Address for correspondence:
Luiz Carlos Manganello-Souza, MD
R. Itapeva, 500 - 1º andar - Conj. 1C
01332-000 - São Paulo - SP Brazil
Phone/Fax: (55 11) 288-7168
e-mail: magane@attglobal.net


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter