

Original Article - Year 2017 - Volume 32 -
Mammoplasty/mastopexy using implants: the Lockpocket technique
Mamoplastia/mastopexia com implante: técnica Lockpocket
ABSTRACT
INTRODUCTION: Mammoplasty is the most commonly performed plastic surgery procedure in Brazil, which is second only to the United States in terms of the number of mammoplasties performed. Several techniques based on increasing volume using breast implants are used to correct breast ptosis. We aimed to describe a technical variation of implant mammoplasty: isolation of the implant in a closed pocket of fascioglandular tissue (Lockpocket).
METHODS: This prospective study was carried out between June 2013 and June 2016. Forty-three patients underwent (1) augmentation mammoplasty using a silicone implant that was isolated from the external environment by a closed pocket of fascioglandular tissue, and (2) resection of excess dermoglandular tissue to correct mammary ptosis. Were subsequently analyzed statistically.
RESULTS: Of the 43 patients, the majority (22 patients) presented grade II ptosis according to the Regnault classification. The volume of glandular tissue removed was similar to the volume of the prosthesis introduced. A total of seven complications were observed: partial dehiscence (n = 4), discrete asymmetry (n = 2), and residual ptosis (n = 1).
CONCLUSION: Augmentation mammoplasty with correction of mammary ptosis (the Lockpocket technique) is a good option because it allows the surgeon to choose in advance the volume of the implant to be used. The method also isolates the implant in a totally closed plane of fascioglandular tissue, and involves the precise removal of breast tissue.
Keywords: Mammoplasty; Breast implant; Breast.
RESUMO
INTRODUÇÃO: A mamoplastia foi o procedimento em cirurgia plástica mais realizado no Brasil, ficando em segundo lugar no mundo, logo atrás dos Estados Unidos. Existem diversas técnicas para correção de ptose das mamas associado a aumento do volume com implantes mamários. O objetivo é descrever uma variação técnica de mamoplastia com prótese, isolando o implante em um bolsão fechado de tecido fascioglandular (Lockpocket).
MÉTODOS: Realizado um estudo prospectivo entre junho de 2013 e junho de 2016 totalizando 43 pacientes que foram submetidos à mamoplastia de aumento com prótese de silicone, isolado do meio externo por um bolsão fechado de tecido fascioglandular, e ressecção de tecido dermoglandular excedente para correção de ptose mamária, sendo realizada análise estatística.
RESULTADOS: Das 43 pacientes, a maioria (22 pacientes) apresentaram ptose grau II, segundo a classificação de Regnault. Os volumes de tecido glandular retirado e volume das prótese introduzidos foram semelhantes, sendo observado um total de sete complicações: deiscência parcial (n = 4), assimetria discreta (n = 2) e ptose residual em um caso.
CONCLUSÃO: A mamoplastia de aumento com correção de ptose mamária - técnica Lockpocket - é uma boa opção, permitindo a escolha prévia do volume do implante utilizado, isolando-o em uma loja totalmente fechada de tecido fascioglandular, e exérese exata de tecido mamário.
Palavras-chave: Mamoplastia; Implante mamário; Mama.
In 2013 alone, 11,599,336 plastic surgery procedures were performed in Brazil. According to data from the International Society of Aesthetic Plastic Surgery and the Brazilian Society of Plastic Surgery, mammoplasty was the most common procedure, with 1,773,584 operations, followed by liposuction. In addition, Brazil occupies second place in terms of the number of breast procedures performed (14.9%) Specifically, 14.9% of women in Brazil have undergone a breast procedure-that places the country just behind the United States, where the figure is 15%1.
Furthermore, among all cosmetic surgery procedures, augmentation mastoplasty with the placement of a silicone implant was performed most often in Brazil, comprising 21% of operations, according to a survey carried out by Datafolha together with the Brazilian Society of Plastic surgery in 20092.
However, some women who present themselves to surgeons as requiring a breast implant are actually seeking to correct breast ptosis associated with increased breast volume. In this regard, the placement of breast implants followed by mastopexy is a controversial subject among plastic surgeons because breast enlargement can in fact mask moderate ptosis in some patients.
However, in most patients, including those with flaccid skin, pseudoptosis, or glandular ptosis, as well as those with grade I or II ptosis and even mild or moderate hypertrophy, breast enlargement mastoplasty may be impractical. In fact, it can even lead to undesirable or poor results3,4. In such cases, simultaneous mastopexy may help in the positioning of the nipple-areolar complex (NAC), as well as in the resection of excess skin and ptosed and/or hypertrophic breast tissue.
Moreover, the correction of breast ptosis using volume increase or replacement may be equally necessary to achieve good results in patients with ptosed or hypertrophic breasts. Mastopexy and breast volume augmentation using implants were first described by Regnault5,6 and by Gonzalez-Ulloa7 five decades prior. The procedure has changed since then, with variable approaches that are tailored to the different forms of each patient's breasts5-7.
The classification system that is currently used most often in cases of breast ptosis was introduced by Regnault in 19765. The system is based on the position of the NAC in relation to the mammary sulcus, and it involves three distinct grades. Furthermore, in addition to real ptosis, two other intermediate forms have been described-partial ptosis and pseudoptosis (Chart 1)5.
On a different note, an increasing number of breast procedures have involved the silicone implant in recent years. For this reason, the number of complications inherent to the procedure has also risen. For example, infections-one of the most feared complications after breast implant surgery-occur in between 1% and 2% of cases, with the most common etiological agents being Staphylococcus aureus and coagulase negative Staphylococcus spp3.
Furthermore, although they occur only infrequently, post-operative infections after breast implant cause great morbidity to the patient: long treatment periods using oral or venous antibiotics, new surgical procedures for implant removal, not to mention the esthetically unsatisfactory results. Other, more frequent, complications include recurrent ptosis, bruises, capsular contracture, poorly positioned implants, poor scars, and a poorly positioned areola.
Several articles have described the correction of breast ptosis using volume increase, removal of excess skin, or both. Nonetheless, correction is difficult for surgeons, especially in terms of planning and execution, and a number of different techniques are used.
OBJECTIVE
The objective of this study was to describe a technical variation in implant mastoplasty: isolation of the mammary implant from the external environment in a closed region of the fascioglandular tissue under the fascia of the pectoralis major muscle (the Lockpocket technique). The procedure uses the initial inframammary approach and allows the surgeon to define the volume of the breast implant prior to the mammoplasty/mastopexy.
METHODS
This prospective study was conducted between June 2013 and June 2016 at the Daher Lago Sul Hospital, Brasília, DF, Brazil. It included a total of 43 patients, who were selected based on the following criteria: (1) primary breasts; (2) ptosis grade I, II, or III, according to the Regnault classification; (3) mild (up to 200 g) or moderate (200-500 g) hypertrophy-also based on the Regnault classification-since to achieve the desired result, it was necessary to remove the tissue, that is, the skin and mammary gland. Statistical analysis was performed using Fisher's exact test, with a 95% confidence interval. All p-values < 0.05 were considered statistically significant.
The surgical planning and operative technique involved marking the skin with the patient in a standing position. In this way, the surgeons defined the breast meridians (hemiclavicular line and breast median), inframammary groove, and Pitanguy point A, which is defined through bidigital marking in the projection of the inframammary groove.
In all cases, general anesthesia and antibiotic prophylaxis were performed using intravenous cefazolin (2 g) 30 minutes before surgery. Antisepsis was ensured using a solution of 4% chlorhexidine and 2% alcohol; sterile fields were also prepared.
With regards to the procedure itself, first, the breasts were infiltrated with a physiological solution that contained adrenaline at a ratio of 1:300,000. An incision of approximately 5 cm in length was made in the bilateral mammary sulcus, and detachment was performed, with the production of the region, within the subfascial plane of the pectoralis major muscle. Tests were carried out using sterile molds until the optimal size of the implant was identified.
Next, the implants were inserted bilaterally, and the region was closed (Figure 1). With the patient in a dorsal decubitus, semiflexed position (30º), a circle was drawn from Pitanguy point A, and points B and C were marked using a bidigital maneuver (pinch-test). The Schwartzman maneuver was used to decorticate the skin in the periareolar region, and an incision was made along the anterior markings. Excess dermoglandular tissue was then excised in accordance with Pitanguy mammoplasty. This technique preserves the muscular fascia surrounding the breast implant and allows local hemostasis.
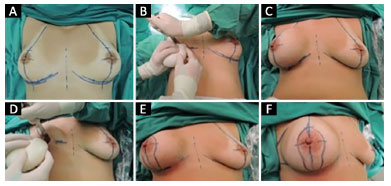
Figure 1. A: Skin marking; B: Production of the subfascial plane and placement of the mold; C: View after mold placement; D: Placement of the silicone implant; E and F: General view after definitive implant placement and closing of the plane.
The NAC was then repositioned using a superomedial pedicle flap (Silveira Neto). Subsequently, pillar assemblies were created using 3-0 and 4-0 mononylon thread, and skin synthesis was performed using 4-0 (intradermal) and 5-0 (subdermal) mononylon thread (Figure 2). Finally, occlusive dressing and bandaging of the breasts were performed. During the post-operative period, antibiotic therapy was performed using second-generation cephalosporin for 7 days.
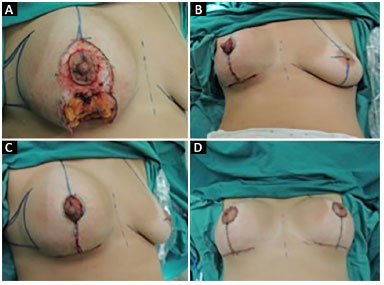
Figure 2. A: Removal of excess breast tissue and skin; B and C: General appearance after resection of excesses; D: Final results.
A total of 43 pairs of breast implants were used: 14 of the brand Silimed® and 29 of the brand Eurosilicone®, both of which were round with a very high profile.
The present study presented no conflicts of interest, and the work conformed to the principles of the Declaration of Helsinki, which was adopted by the 18th World Medical Assembly in Helsinki, Finland, in June 1964 and corrected by the 29th Medical Assembly, Tokyo, Japan, in October 1975, and by the 35th World Medical Assembly, Venice, Italy in October 1983, and by the 41st World Medical Assembly, Hong Kong, China, in September 1989.
RESULTS
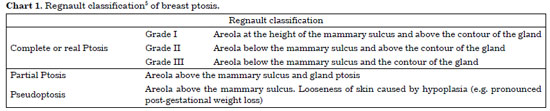
A total of 43 patients were analyzed. All were aged between 21 and 65 years, with an average body mass index (BMI) of 24.6, and all cases involved primary breast surgery (Figure 3). Of the 43 patients, four presented ptosis grade I, 22 had ptosis grade II, and 17 exhibited ptosis grade III. The average volume of tissue removed was 290 g from the right breast and 291.3 g from the left breast, varying between 100 g and 470 g. Six patients presented mild hypertrophy, and 37 exhibited moderate hypertrophy.
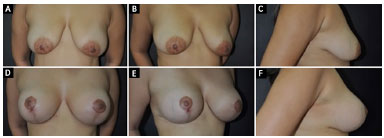
Figure 3. A, B and C: Pre-operative period of a 20-year-old patient with breast ptosis and asymmetry; D, E and F: Post-operative view 6 months after mammoplasty with breast implant and the Lockpocket technique.
A total of 43 pairs of silicone prostheses were used: 14 of the brand Silimed® round with a super high profile and an average volume of 271.5 ml) and 29 of the brand Eurosilicone® (same specifications, with a volume of 275.17 ml). It should be noted that, in a follow up period of 1 year, there were two cases of discrete asymmetry using the Eurosilicone® brand.
The mean volumes of the prostheses used varied according to the patient's desire and the expected size during the pre-operative period. However, the final size was chosen during the operation itself. The average volume of the implants was 273.25 ml, ranging from 240 ml to 400 ml. The post-operative follow-up period varied from 3 to 9 months (Figures 4 and 5).
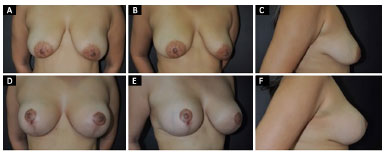
Figure 4. A, B and C: Pre-operative period in a 30-year-old patient with breast ptosis; D, E and F: Post-operative view 1 year after mammoplasty with breast implants and the Lockpocket technique.
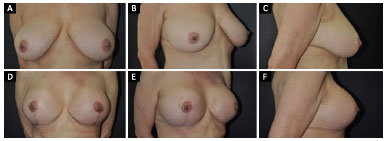
Figure 5. A, B and C: Pre-operative view in a 52-year-old patient with breast ptosis and moderate hypertrophy; D, E and F: Post-operative view 1 year after mammoplasty using the Lockpocket technique.
Seven complications were observed: partial dehiscence of the inverted T (n = 4), discrete asymmetry (n = 2), and residual post-operative ptosis (n = 1). There were no cases of breast infection, hematoma, seroma, or other complications. Cases of partial dehiscence of the scar junctions in the T were treated using serial dressings with Kolagenase®. The only case where repeat surgery was necessary was due to ptosis of the NAC. This was easily resolved by new mastopexy, which was performed in an outpatient clinic.
In all patients but one, the volume of breast tissue removed resembled the volume of the breast implant introduced, with a mean implant size of 273.95 ml and a mean resected volume of 290 ml.
The results obtained in this study were subjected to statistical analysis. However, no significant difference was found among them using the statistical techniques described in the Methods.
To correct the degree of ptosis, in addition to mammoplasty techniques, the size of the prosthesis varied according to breast type. In cases of grade I ptosis, the mean volume used was 255 ml, while grade II and grade III ptosis involved a mean volume of 275.45 ml and 276.47 ml, respectively.
DISCUSSION
Several techniques, all of which present a high degree of difficulty, have been used to combine breast implants with mastopexy or mammoplasty. For a long time, we sought a technique that could yield satisfactory and long-lasting results along with good reproducibility.
Several authors have reported their own techniques. For example, Sanchéz et al.8 used the inferior pedicle to protect the breast implant, while Soares et al.9 prepared a double space for the implant within a subglandular and submuscular plan in the inferior portion. In contrast, Gomes10 described a technique for mastopexy and breast implant that used a superior pedicle flap. Mansur and Bozola11 also used the inferior pedicle to support and protect the implant without causing it to slide. Graf el al.12 demonstrated the subfascial plan for the placement of breast implants, adding a structure that was able to promote greater protection.
Reduction mammoplasty amounts to mastopexy with the removal of most of the breast tissue, while mastopexy itself is-or should be-only a small breast reduction. In breast ptosis correction, good surgical outcome relies on treatment of the excess skin and glandular tissue of the inferior pole, with adjustments of tissues serving to correct the ptosis. It follows that the result may be unpredictable when periareolar mastopexy or skin removal alone is used13. Indeed, after excess skin and breast tissue have been recognized, any maneuver that limits their removal becomes ineffective.
Breast reduction surgery is combined with insertion of breast implants in a subgroup of patients who wish to have a breast reduction, but who also want to fully improve their upper pole, which is often deficient in such patients. For this reason, these patients often report a better redistribution of the breast tissue from the lower to the upper poles.
The combination of Pitanguy mammoplasty with breast implants increases patient satisfaction, as the technique can improve the upper pole, confer adequate repositioning of the NAC, and yield lasting results. Both objectives-filling the upper pole while ensuring little projection of the lower pole-can be promoted using this technique; thus, the method provides a redistribution of the breast tissue between the lower and upper parts of the breast.
In the present study, attention was paid to the details of surgical planning and technique so that of the principles of Pitanguy mammoplasty could be used in addition to skin removal for mastopexy. This enabled effective emptying of the breast tissue, which led to a smaller accumulation of tissue at the inferior pole, combined with resection of the medial and side portions of the breast.
In addition, the current study placed the breast implants within a safe pocket (Lockpocket) in a previously prepared subfascial plane. Such an approach prevents extrusion of the breast implant in the case of wound dehiscence. It also prevents implant contact with the mammary gland. Another advantage of placing the breast implant before performing mammoplasty/mastopexy is that surgeons can predict the amount of tissue that can be safely resected without presenting risks during closure. Thus, they can properly plan the exact amount of skin and tissue to be resected.
Mammoplasty or mastopexy with breast implant is a technically challenging procedure. A recent meta-analysis, carried out by Khavanin et al.14 in 2014, included 23 studies (4,856 cases) involving mammoplasties with silicone implants. The study summarized the complication profiles and reoperation rates of the included studies, demonstrating that they were acceptably low in this kind of surgery-comparable to published results involving reductive mammoplasty without prosthesis. Specifically, the total complication rate was 13.1%. The most common complication was recurrent ptosis, with an incidence of 5.2%, followed by changes in the healing process. The reoperation rate, obtained from 13 studies, was 10.7%.
In the present study, the overall complication rate was 19%, with the main complication being surgical wound dehiscence (9%), followed by asymmetry and ptosis, with 5% of cases.
Several articles have reported different rates of surgical wound dehiscence, although the figure has been between 5%-16% in all cases15,16. In the present study, we found that all cases of partial dehiscence above 0.5 cm were treated at the local outpatient clinic. Treatment of this kind lasted 2 weeks at most, with excellent general results during a 1-year follow-up.
In a study by Khavanin et al.14 in 2014, breast ptosis occurred in approximately 2.5% of cases, which corroborates our own findings. It is understood that various factors, such as skin type and elasticity, age, and degree of breast liposubstitution can affect the final esthetic result and ptosis. In any case, the low values of ptosis recurrence are acceptable and in agreement with the current literature.
All patients in the present study received intra-operative antibiotic prophylaxis with cefazolin (1 g), as well as second-generation post-operative antibiotic therapy with cephalosporin for 7 days.
There were no cases of breast infection or post-operative scarring, contrary to the consensus of the American Society of Plastic Surgery, 2015, in which the infection rate in this type of surgery is 2.5% when associated with intra-operative antibiotic prophylaxis. In fact, the Lockpocket technique, in which the implant is inserted in a safe pocket of lipoglandular tissue, without contact with the mammoplasty or mastopexy environment, promotes another protective barrier against infectious processes in this type of surgery15-18.
In a study by Shah et al.,19 the overall rate of post-operative complications was higher in patients with a BMI above 3019. However, in the present study, all patients had a BMI under 30, and there was no statistically significant difference between general complications and BMI.
CONCLUSION
Placement of breast implants followed by Pitanguy mammoplasty using an initial approach through the mammary sulcus in the subfascial plane (Lockpocket) is a good option in cases of augmentation mastoplasty that are associated with the correction of pre-existing ptosis and light/moderate hypertrophy. Such an approach allows the surgeon to predetermine the volume of implant to be used. In addition, this method isolates the implant in a region that is totally closed; it also allows precise removal of redundant skin and breast tissue, with a lower risk of infection. So far, the results show that this is a safe technique that prevents tissue accumulation in the lower pole of the breasts. Most importantly, the method can be easily reproduced.
COLLABORATIONS
CADCF Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
LGM Analysis and/or interpretation of data; statistical analyses; conception and design of the study; completion of surgeries and/ or experiments; writing the manuscript or critical review of its contents.
CMA Analysis and/or interpretation of data; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
MCAG Analysis and/or interpretation of data; statistical analyses; conception and design of the study; completion of surgeries and/ or experiments; writing the manuscript or critical review of its contents.
GCS Analysis and/or interpretation of data; statistical analyses; conception and design of the study; completion of surgeries and/ or experiments; writing the manuscript or critical review of its contents.
DBP Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
FTM Statistical analyses.
JCD Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
REFERENCES
1. International Society of Plastic Aestethic Surgery (ISAPS). Quick Facts: Highlights of the ISAPS 2013 Statistics on Cosmetic Surgery [acesso: 2016 Maio 10]. Disponível em: http://www2.cirurgiaplastica.org.br/wp-content/uploads/2014/08/ISAPS_quick_facts.pdf
2. Pesquisa Datafolha. encomendada pela Sociedade Brasileira de Cirurgia Plástica. [acesso: 2016 maio 10]. Disponível em: http://www2.cirurgiaplastica.org.br/wp-content/uploads/2012/11/pesquisa2009.pdf
3. Haiavy J, Tobin H. Mycobacterium fortuitum infection in prosthetic breast implants. Plast Reconstr Surg. 2002;109(6):2124-8. DOI: http://dx.doi.org/10.1097/00006534-200205000-00051
4. Davison SP, Spear SL. Simultaneous breast augmentation with periareolar mastopexy. Semin Plast Surg. 2004;18(3):189-201. DOI: http://dx.doi.org/10.1055/s-2004-831906
5. Regnault P. The hypoplastic and ptotic breast: a combined operation with prosthetic augmentation. Plast Reconstr Surg. 1966;37(1):31-7. PMID: 5903218 DOI: http://dx.doi.org/10.1097/00006534-196637010-00004
6. Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976;3(2):193-203.
7. Gonzales-Ulloa M. Correction of hypotrophy of the breast by means of exogenous material. Plast Reconstr Surg. 1960;25(1):15-40. DOI: http://dx.doi.org/10.1097/00006534-196001000-00002
8. Sanchéz J, Carvalho AC, Erazo P. Mastopexia com prótese: técnica em "D" espelhado. Rev Bras Cir Plást. 2008;23(3):200-6.
9. Soares AB, Franco FF, Rosim ET, Renó BA, Hachmann JOPA, Guidi MC, et al. Mastopexia com uso de implantes associados a retalho de músculo peitoral maior: técnica utilizada na Disciplina de Cirurgia Plástica da Unicamp. Rev Bras Cir Plást. 2011;26(4):659-63. DOI: http://dx.doi.org/10.1590/S1983-51752011000400021
10. Gomes RS. Mastopexia com retalho de pedículo superior e implante de silicone. Rev Bras Cir Plást. 2008;23(4):241-7.
11. Mansur JRB, Bozola AR. Mastopexia e aumento das mamas com proteção e suporte inferior da prótese com retalho de pedículo inferior. Rev Bras Cir Plást. 2009;24(3):304-9.
12. Graf RM, Bernardes A, Rippel R, Araujo LR, Damasio RC, Auersvald A. Subfascial breast implant: a new procedure. Plast Reconstr Surg. 2003;111(2):904-8. PMID: 12560720 DOI: http://dx.doi.org/10.1097/01.PRS.0000041601.59651.15
13. Swanson E. A retrospective photometric study of 82 published reports of mastopexy and breast reduction. Plast Reconstr Surg. 2011;128(6):1282-301. DOI: http://dx.doi.org/10.1097/PRS.0b013e318230c884
14. Khavanin N, Jordan SW, Rambachan A, Kim JY. A systematic review of single-stage augmentation-mastopexy. Plast Reconstr Surg. 2014;134(5):922-31. PMID: 25347628 DOI: http://dx.doi.org/10.1097/PRS.0000000000000582
15. Xue AS, Wolfswinkel EM, Weathers WM, Chike-Obi C, Heller L. Breast reduction in adolescents: indication, timing, and a review of the literature. J Pediatr Adolesc Gynecol. 2013;26(4):228-33. DOI: http://dx.doi.org/10.1016/j.jpag.2013.03.005
16. Rubin JP, Gusenoff JA, Coon D. Dermal suspension and parenchymal reshaping mastopexy after massive weight loss: statistical analysis with concomitant procedures from a prospective registry. Plast Reconstr Surg. 2009;123(3):782-9. PMID: 19319040 DOI: http://dx.doi.org/10.1097/PRS.0b013e31819ba1a8
17. Wong C, Vucovich M, Rohrich R. Mastopexy and reduction mammoplasty pedicles and skin resection patterns. Plast Reconstr Surg Glob Open. 20148;2(8):e202. PMID: 25426385
18. Ariyan S, Martin J, Lal A, Cheng D, Borah GL, Chung KC, et al. Antibiotic prophylaxis for preventing surgical-site infection in plastic surgery: an evidence-based consensus conference statement from the American Association of Plastic Surgeons. Plast Reconstr Surg. 2015;135(6):1723-39. DOI: http://dx.doi.org/10.1097/PRS.0000000000001265
19. Shah R, Al-Ajam Y, Stott D, Kang N. Obesity in mammaplasty: a study of complications following breast reduction. J Plast Reconstr Aesthet Surg. 2011;64(4):508-14. PMID: 20682461 DOI: http://dx.doi.org/10.1016/j.bjps.2010.07.001
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Daher Lago Sul, Brasília, DF, Brazil
3. Sociedade Brasileira de Anestesiologia, Rio de Janeiro, RJ, Brazil
Institution: Hospital Daher Lago Sul, Brasília, DF, Brazil.
Corresponding author:
César Augusto Daher Ceva Faria
SGAS 610 bloco F, torre 2, salas 132/133/134 - Asa Sul
Brasília, DF, Brazil Zip Code 70200-700
E-mail: cesardaher@terra.com.br
Article received: October 14, 2016.
Article accepted: February 21, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter