

Original Article - Year 2017 - Volume 32 -
Analysis of the treatment protocol for sternotomy wound infection after cardiac surgery
Análise crítica do protocolo de tratamento da ferida operatória complicada após esternotomia para cirurgia cardíaca
ABSTRACT
INTRODUCTION: Surgical wound complications after sternotomy in cardiovascular procedures include small dehiscences, mediastinitis, and sternal osteomyelitis. Mediastinitis and sternal osteomyelitis are high-risk complications associated with high rates of morbidity, mortality, and recurrence. Treatment of the most severe cases involves prolonged hospitalization. Moreover, the long-term use of antibiotics during hospitalization and after discharge significantly increases the overall cost of treatment. A recent treatment option involves extensive surgical debridement of the surgical wound, treatment of the wound bed with negative pressure therapy, and closure of the wound with myocutaneous or fasciocutaneous flaps. The advantages of this strategy include improvement of the patient's quality of life, less manipulation and less discomfort for the patient, less burden on staff involved in care, lower rate of infection recurrence, and an overall reduction of treatment morbidity.
METHODS: The objective of this study was to conduct a retrospective survey of patients with surgical wound complications who were treated according to a protocol developed and improved by the Heart Institute of the Clinic Hospital of the School of Medicine of the University of São Paulo (Instituto do Coração do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo-InCor/HC-FM-USP), and who underwent surgery by the same plastic surgeon. The epidemiological profiles and possible indicators of worse prognosis were determined from routine examinations performed on these patients. The medical records of patients treated at InCor/HC-FM-USP who presented with sternotomy infection in 2014 were assessed retrospectively. The analyzed variables included comorbidities, interval between surgical procedures, C-reactive protein (CRP) levels, wound closure procedures, and treatment complications, among others.
RESULTS: The data are predominantly descriptive and epidemiological. At least one comorbidity was present in 84% of cases. The mean number of surgical procedures per patient was 2.5, ranging from 1 to 7. The CRP levels decreased in 75% of patients after the first surgical procedure, and the mortality rate was 17%.
CONCLUSION: The standardized method adopted significantly decreased the overall mortality and the rates of recurrence and readmission. Indicators of worse prognosis, including CRP levels and the leukogram, were identified at the time of diagnosis and initiation of the treatment protocol.
Keywords: Mediastinitis; Osteomyelitis; Surgical wound infection; Surgical flaps; Wound treatment with negative pressure.
RESUMO
INTRODUÇÃO: As complicações de ferida operatória após esternotomia para acessos cirúrgicos para procedimentos cardiovasculares variam desde pequenas deiscências até mediastinite e osteomielite do esterno. Mediastinite e osteomielite do esterno associam-se a alto risco, alta morbidade e altas taxas de mortalidade, além de altas taxas de recidiva. O tratamento nos casos de maior gravidade envolvem internação hospitalar prolongada. A utilização de antibióticos por tempo prolongado, durante a internação, e após a alta, tem impacto importante no custo global do tratamento. Mais recentemente, uma opção de tratamento envolve o amplo debridamento cirúrgico da ferida em centro cirúrgico, preparo do leito da ferida com terapia por pressão negativa, seguida do fechamento da ferida com retalhos miocutâneos ou fasciocutâneos. Aparentemente, essa estratégia traz vantagens como a melhora na qualidade de vida do paciente, menor manipulação e menor incômodo ao doente, menos sobrecarga para os profissionais de saúde envolvidos nos cuidados, menor taxa de recidiva infecciosa e, assim, redução da morbidade do tratamento como um todo.
MÉTODOS: O presente estudo tem por objetivo realizar levantamento dos pacientes vítimas dessa grave complicação que tenham sido tratados segundo protocolo desenvolvido e aprimorado no Instituto do Coração do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (InCor - HCFMUSP), e que tenham sido operados por um mesmo cirurgião plástico, a fim de analisar o perfil epidemiológico, e eventual indicador de pior prognóstico dentre os exames colhidos habitualmente desses pacientes. Foram avaliados, retrospectivamente, os prontuários dos pacientes atendidos no InCor - HCFMUSP vítimas de infecção de esternotomia durante o ano de 2014. As variáveis analisadas foram comorbidades, intervalo entre abordagens cirúrgicas, valores de Proteína C Reativa (PCR), procedimento empregado no fechamento da ferida, complicações do tratamento, entre outros.
RESULTADOS: Os dados são essencialmente descritivos e de caráter epidemiológico: observa-se a incidência de ao menos uma comorbidade em 84% dos pacientes; média de 2,5 procedimentos cirúrgicos por paciente, variando de 1 a 7 procedimentos; queda nos níveis de PCR em 75% dos pacientes já após o primeiro procedimento cirúrgico e mortalidade de 17%, entre outros dados.
CONCLUSÃO: Os dados analisados nos permitem concluir que o método padronizado adotado trouxe impacto na redução da mortalidade global dos pacientes, além da redução de recidiva e reinternações. Identificamos, ainda, indicadores de pior prognóstico como PCR e leucograma no momento do diagnóstico e indicação da aplicação do protocolo.
Palavras-chave: Mediastinite; Osteomielite; Infecção da ferida cirúrgica; Retalhos cirúrgicos; Tratamento de ferimentos com pressão negativa.
Surgery in the thoracic cavity is very complex and requires specialized skills and extended training. In cardiac surgery, in particular, the complexity, expertise, and training involved are even greater, because the target of surgery, the heart, tolerates no errors, and because the clinical status of the patient is poor, with multiple comorbidities1, even among patients undergoing elective surgery. With an increase in life expectancy in Brazil, as reported by the Brazilian Institute of Geography and Statistics (Instituto Brasileiro de Geografia e Estatística - IBGE), and with greater access to healthcare, cardiac interventions have increased, and the absolute number of complications inherent to these procedures has also increased.
One of the complications inherent to any surgery is wound infection2.
In the case of cardiac surgery, the most frequently used approach is median sternotomy, which, similar to other surgical procedures, may present complications due to infection. The range of presentation of sternotomy wound infections varies considerably and includes mild hyperemia, pain and edema around the surgical wound (which regress with local care and simple antibiotic therapy), and severe mediastinitis, with involvement of the sternum (sternal osteomyelitis) and critical structures, including the heart3.
The most severe cases of sternotomy wound infection are always accompanied by global decompensation of associated baseline comorbidities, including diabetes, hypertension, and congestive heart failure, among others.
Severe infection combined with decompensation of comorbidities leads to high mortality, high morbidity, prolonged hospitalization, and extensive manipulation and invasion of the patient, which progressively worsens the prognosis3-5.
The adopted nomenclature also creates some confusion. A search of the ICD-10 (last revision in 2012, published by the Regional Council of Medicine of the State of São Paulo [Conselho Regional de Medicina do Estado de São Paulo - CREMESP]: http://www.cremesp.org.br/pdfs/cid10_ultimaversaodisponivel_2012.pdf), found no results for the terms "mediastinitis," "surgical wound infection," "sternotomy infection," and "sternal osteomyelitis." For this reason, these terms will be treated as synonyms in this study.
The Centers for Disease Control and Prevention of the United States (CDC) defined mediastinitis as the presence of at least one of the following criteria: 1 - culture isolation of a microorganism from the secretions or a fragment of the mediastinal wound collected for diagnostic evaluation; 2 - evidence of mediastinitis detected during surgery; 3 - one of the following conditions: chest pain, sternal instability, and fever (> 38 degrees), associated with purulent discharge from the mediastinal wound or enlargement of the mediastinum on imaging.
Sternotomy wound infections are caused by several factors1: previous colonization of the wound edges, lack of asepsis of the materials used during surgery, human failure in antisepsis, prolonged exposure to the external environment, immunosuppression due to underlying diseases, low efficacy of antibiotic prophylaxis, and failure to administer antibiotic prophylaxis.
The best strategy is prevention. Even with all the care taken to reduce the chances of failure, previous studies reported that the rate of mediastinitis varied from 0.5% to 10% and the mortality rate was higher than 50%4.
The recommended treatment for this complication consists of re-suturing of the sternum with steel wire, wound debridement, and continuous irrigation until second intention healing. This treatment is relatively effective but involves prolonged hospitalization, extensive wound manipulation, maintenance of an open wound with constant secretion because of the need for irrigation, bed confinement, high rate of recurrence, and chronicity of sternal osteomyelitis1,6.
Because of the need to improve the quality of patient care, reduce the length of hospitalization, improve quality of life, and reduce the overall cost of treatment5,7, an alternative approach to this condition was proposed: the protocol adopted by the Heart Institute of the Clinic Hospital of the School of Medicine of the University of São Paulo (Instituto do Coração do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo-InCor/HC-FM-USP). In general, this protocol involves aggressive debridement of the wound in the first surgical approach, negative pressure therapy (NPT), exchange of NPT kits, and repeated debridement as required. After adequate preparation of the wound, definitive closure with myocutaneous or fasciocutaneous flaps is performed to improve vascularization of the affected sternal areas and aid in treatment of the infection.
We evaluated three patients treated according to this protocol and provide imaging data to show the procedures adopted in each step:
- Patient 1: Figure 1A shows wound status in the first intervention. Skin sings revealed attempts for previous suture done by another specialist, but without success. Figure 1B shows the real status of the wound after simple opening of the skin, revealing a large dead space, with important sternal distancing, associated with devitalized tissue and fibrin. The figure 1C reveals the final aspect of the wound after end of the debridement, given the example of effectiveness of surgical cleaning. Figure 1D exemplifies the negative pressure therapy applied after adequate debriding. The figure 1E reveals the wound aspect immediately after removal of negative pressure therapy in the second approach. Figure 1F shows the final aspect of the wound, in the third surgery, after 14 days of negative pressure therapy. In figure 1G we observed final aspect of suture of the wound, revealing the adequate reestablishment of the patient and its routine activities.
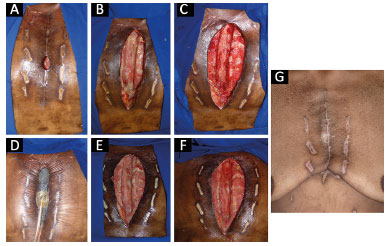
Figure 1. A: Initial evaluation; B: Appearance of the wound bed after skin incision. There was extensive devitalized tissue beyond the borders of the sternum, and a large area developed complete dehiscence of the sternotomy; C: Appearance of the wound after debridement; D: Use of negative pressure therapy in the wound; E: Appearance of the wound bed after 6 days of negative pressure therapy; F: Appearance of the wound bed after 13 days of negative pressure therapy, immediately before closure with surgical flaps; G: Final appearance, at a later follow-up, demonstrating the effectiveness of the protocol.
- Patient 2: Figure 2A shows in the initial wound a little before the first approach by surgical plastic. We observed distal and proximal dehiscence, but, apparently, with integrative of good part of sternotomy. After, in figure 2B, we can observe the real status of the wound after simple opening of the skin, revealing large dead space, and communication between two dehiscent extremities, with recovering bed by tecidual necrosis and purulent secretion. After large debridement approach in the routine, we observe in figure 2C the quality of surgical debridement, remaining only the viable tissue with good aspect of final surgical cleaning. The negative pressure therapy was applied routinely in this protocol, as shown in figure 2D. Nine days after surgical cleaning, the aspect of the wound can be observed in figure 2E. Figure 2F shows quality of suture and adequate resolution of complication 3 months after surgery.
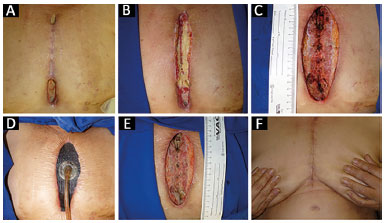
Figure 2. A: The appearance of the wound at the initial evaluation by the plastic surgery team; B: Appearance of the wound bed after a skin incision. There was extensive devitalized tissue; C: Appearance of the wound at the end of the initial debridement in the first surgical approach; D: Treatment with negative pressure therapy; E: Appearance of the wound bed after 9 days of negative pressure therapy; F: Appearance of the wound bed 3 months after closure of the sternal wound, with no signs of recurrence.
Patient 3: the aspect found immediately before the beginning of the first surgery is shown in figure 3A, in which we observed dehiscence of third distal of sternotomy with visualization in deep of exposed steel wires. Again, in figure 3B, we can observe the real status of surgical wound after simple opening of the skin. We can observe a dead space through the surgical wound, and its bed recovery by tecidual necrosis, purulent secretion, and exposition of steel wires used for closing the sternum. The figure 3C exemplify surgical debridement of the wound, in block, all devitalized tissue and frankly contaminated. The result after final surgical cleaning is observed in figure 3D. The figure 3E reveals the aspect just after resolution of the wound, in the third surgery, according to the protocol. Finally, the figure 3F reveals the final scaring aspect after 4 weeks of closing, and figure 3G, already with 3 months, without sings of recurrence or complication.
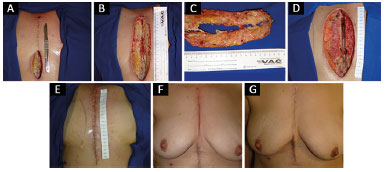
Figure 3. A: The image shows the appearance of the wound during the initial evaluation by the plastic surgery team; B: Appearance of the wound bed after a skin incision; C: Product of en bloc wound debridement; D: Appearance after 11 days of negative pressure therapy; E: Appearance after wound closure with surgical flaps; F: Appearance after 1 month in outpatient follow-up; G: Appearance after 3 months, without signs of infection recurrence in outpatient follow-up.
The thorough initial evaluation of the patient upon early suspicion of this complication plays a decisive role in the treatment outcome. All aspects of the wound should be thoroughly evaluated: extent of dehiscence, amount of secretions, appearance of the secretions, presence of dead space in the operative wound on physical examination, computed tomography findings (if available), and blood tests, including C-reactive protein (CRP) levels and the leukogram. In addition to the initial evaluation and physical examination, cultures of the wound secretions and blood cultures should be performed for a suspected infection.
Because of the high morbidity and mortality of this condition, a simple diagnostic suspicion after the initial evaluation is sufficient to indicate immediate and aggressive treatment of the complication.
OBJECTIVE
The objective of this study was to conduct a retrospective survey of patients who presented with a surgical wound infection after cardiac surgery and who were treated by a single plastic surgeon (the author of this study) in a cardiac surgery referral center. The epidemiological profile, possible prognostic factors, quality and effectiveness of the treatment, and measures to improve the systematic protocol of care for patients with this severe condition were assessed, with the aim of increasing knowledge about this condition and ultimately improving prevention strategies.
METHODS
The present study was approved by the Research Ethics Committee (REC) of the HC-FM-USP (Protocol No. 10.534). The REC granted a request for exemption from free and informed consent for all patients because the review of medical records was retrospective.
All study participants were evaluated, surgically treated, and monitored by a plastic surgeon (the author of this manuscript) at the InCor/HC-FM-USP.
Inclusion criteria
All patients with a sternotomy wound infection after cardiac surgery, who were identified using the criteria for the diagnosis of mediastinitis established by the CDC and underwent surgery by the author of this manuscript, were included. There were no exclusion criteria.
Analysis of medical records
The medical records of patients treated at InCor/HC-FM-USP in 2014 who presented with mediastinitis and were contacted by the plastic surgery team were evaluated.
The studied variables included age, sex, comorbidities (diabetes, hypertension, dyslipidemia), use of the internal thoracic (mammary) artery as the route of access, body mass index (BMI), previous history of smoking, result of bone sternal biopsy when available, length of hospitalization, duration of use of NPT, exchange interval of the NPT kit (sponge), and laboratory results, including CPR and leukogram.
Statistical analysis
Data were collected using Microsoft® Excel®. The statistical analysis of direct and descriptive data was conducted using Prism® 6 for Mac OSX®.
Analysis of the study sample and search for risk and prognostic factors
This study will serve as a reference for future research on correlations between comorbidities and prognostic factors for wound infection, and for the development of effective strategies for prevention.
Improvement of the care protocol
At the end of the study, based on findings and literature data, improvements and updates to the protocol of care for patients with surgical wound infections after cardiac surgery will be proposed to ensure the adoption of the best possible therapies and the continuous and sustained evolution of these therapies.
RESULTS
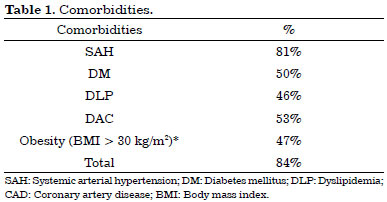
Of the 64 patients, 30 were women (47%) and 34 were men (53%), and the median age was 62 years. In addition, 84% of the patients (54 of 64) had comorbidities, including systemic arterial hypertension (SAH) (81%), diabetes mellitus (DM) (50%), dyslipidemia (DLP) (46%), and coronary artery disease (CAD) (53%). The rate of obesity (BMI > 30 kg/m2) was 47%, although this percentage did not include all patients, and 40% of the patients were smokers.
The mammary arteries were used as the route of access for myocardial revascularization in 37 patients who developed mediastinitis, corresponding to 57% of the total. The CRP levels decreased in 75% of patients after the first surgical approach (aggressive debridement) adopted by the plastic surgery team. The mean initial CRP level in the total sample was 76 mg/L, and decreased by 53% to a mean value of 36.2 mg/L after wound closure.
The mean interval between cardiac surgery and the first surgical approach was 35.7 days. The mean number of procedures performed by the plastic surgery team on each patient was 2.5, and the mean number of times a wound reopened after closure was 5. The most commonly chosen technique was a bilateral fasciocutaneous flap.
Eleven deaths occurred even after careful application of the protocol, corresponding to a mortality rate of 17%, and only one patient was readmitted after discharge because of surgical wound dehiscence and chronic osteomyelitis (recurrence). The median ages of the 11 patients who died and the survivors were 61 and 57 years, respectively (p = 0.91).
All 11 patients who died had at least one comorbidity; 81% of these patients had SAH (versus 81% in the survival group, p = 0.96), 63% had DM (versus 47% in the survival group, p = 0.32), 63% had CAD (versus 51% in the survival group, p = 0.44), and 45% had DLP (versus 47.2% in the survival group, p = 0.91). These results indicate that none of the evaluated comorbidities increased the risk of death after development of sternotomy wound infection.
The analysis of these comorbidities indicated that two patients (18%) had at least two associated comorbidities, and six (54%) patients had at least three comorbidities. In addition, approximately 72% of the patients had other comorbidities, including congestive heart failure, renal insufficiency, or immunosuppression after organ transplantation, among others. Furthermore, 36% of the patients who died were smokers (versus 39% in the survival group, p = 0.84) and 40% were obese. The rate of obesity was not compared between the two groups because of missing data in the medical records of the survivor group.
Internal thoracic arteries were used as the route of access for myocardial revascularization in 63% of the patients, and the most common cardiac surgery was myocardial revascularization with extracorporeal circulation in five cases (45%). Excluding six patients who did not have complete data, the CRP levels decreased after the first surgical approach in 71% of the cases.
The initial mean CRP level before plastic surgery was 143.2 mg/L, and decreased by 55% to 65.12 mg/L after wound closure. Moreover, the analysis at the initial evaluation by the plastic surgery team indicated that the mean CRP level in the 11 patients who died and in those who survived was 143.2 mg/L and 44.1 mg/L, respectively, and this difference was significant (p = 0.0053).
The mean interval between cardiac surgery and the first surgical approach was 22 days in the deceased group and 30 days in the survival group (p = 0.059). The mean number of procedures per patient was 3.0, and 36% of deceased patients died after wound closure with surgical flaps.
DISCUSSION
Comorbidities were present in 84% of patients overall, and in all patients who died (Table 1), indicating that comorbidities are common in patients who develop sternotomy infections8,9. In our series, hypertension was the most common comorbidity, accounting for 81% of all comorbidities. The rate with at least two comorbidities was also high and reached 73% among the patients who died. This rate is significant in absolute numbers.
However, our results indicated no significant differences in comorbidities between the study groups, suggesting that although some comorbidities are known to increase the risk of development of infection, they do not appear to increase the risk of death in cases in which comorbidities are already present. Notwithstanding, the sample size was small. Therefore, future studies should evaluate the effect of comorbidities in combination or isolation on the course of the disease. These studies should address improvements in the treatment strategies and routines and evaluate comorbidities in the patients who have already developed infections.
Among the analyzed variables, obesity and smoking are behavioral comorbidities, amenable to treatment before cardiovascular surgery in the elective cases. The study found a high prevalence of these variables among the analyzed patients, with rates of 47% and 40%, respectively. The ratio of these variables was also high in patients who died, corresponding to 40% and 36%, respectively. As in the case of nonbehavioral comorbidities, there were no statistical differences in these variables that would explain an increase in the risk of death in cases in which the infection had already been established. However, no definitive conclusions can be drawn because of the small sample size.
Internal thoracic arteries (previously designated mammary arteries) were used as the route of access in 57% of all patients. This procedure was used in 63% of the patients in the deceased group. However, no definitive conclusions can be made because of the limited number of cases. Notwithstanding the small sample size, our results provided no evidence that the use of the internal thoracic arteries is a factor in worse prognosis after the development of a sternotomy wound infection. It is well known that the use of the internal thoracic arteries is a risk factor for the development of infection8, but this did not appear to play a role in patient prognosis after the diagnosis of infection.
The measurement of CRP levels is a simple, accessible, and cost-effective procedure. The CRP curve during the treatment of infection (protocol application) could have a prognostic value. In this study, the CRP levels decreased after each procedure, and the levels decreased in 75% of the patients after the first surgical approach.
Despite the statistically significant difference between the study groups, CRP was suitable as a predictor of poor prognosis only at its initial measurement (143.2 vs. 44.1, p = 0.0053) (Table 2). The decrease in the CRP levels between the first and second surgical approach was not significantly different (mean decrease of 54.3 in the deceased group versus 8 in the survival group, p = 0.16).

As in the case of CRP, the total leukocyte count at the initial evaluation also had statistical power, with a mean initial count of 11,490 leukocytes in the deceased group, compared with 6,750 in the survivor group (p = 0.0374) (Table 2). This unexpected result reveals that the initial leukocyte count is a risk factor for worse prognosis in cases of sternotomy wound infection.
Another significant finding was the role of patient's sex: 81% of the patients who died and only 47.2% of the patients who survived were men (p = 0.0361; Figure 4). Therefore, male sex is a risk factor for worse prognosis in this type of infection.
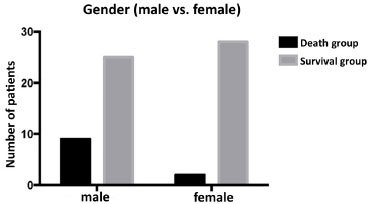
Figure 4. Differences in sex between the survival and death groups. The male patients are more likely to die than the female patients (p = 0.0361).
The surgical technique used for wound closure was either general or individualized, depending on the condition of the wound and the sternum, as is routine practice in surgery. The characteristics of the types of flaps (myocutaneous or fasciocutaneous) in cases in which they were used may be further analyzed, because of the structural differences of the flaps and relationship to the postoperative course. However, considering that the indication for each flap type is individualized, the advantages of one type over the other could not be easily identified because they were applied to distinct groups.
CONCLUSION
In a broader analysis considering deaths (11 cases, 17%) and readmissions (1 case, 1.5%), the adopted protocol was effective in absolute numbers. It should be noted that the numbers cannot be compared with literature data because our data represent a population selected a priori, corresponding to patients subjected to surgical treatment, and therefore only the most severe cases were selected among all cases of sternotomy infection. However, the mortality rate in our sample was within the expected range, compared with the rate in the literature, and tended to be in the lower values of the range.
The rate of recurrence in the study sample was low, although the rate reported in the literature for this condition is high. However, only one case of recurrence (1.5%) was found in this study, demonstrating the benefit of the application of a standard protocol for care and treatment.
The author made a prospective analysis of patient data in real time, and the presented data will be complemented soon. An increase in the study sample size may allow us to reach conclusions with a higher level of evidence and enable improvement of the adopted protocol.
COLLABORATIONS
STG Analysis and/or interpretation of data; statistical analyses; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
TTM Analysis and/or interpretation of data.
FMF Analysis and/or interpretation of data.
DMA Analysis and/or interpretation of data.
TMVS Conception and design of the study.
FBJ Conception and design of the study.
RG Conception and design of the study.
REFERENCES
1. Sjögren J, Malmsjö M, Gustafsson R, Ingemansson R. Poststernotomy mediastinitis: a review of conventional surgical treatments, vacuum-assisted closure therapy and presentation of the Lund University Hospital mediastinitis algorithm. Eur J Cardiothorac Surg. 2006;30(6):898-905. DOI: http://dx.doi.org/10.1016/j.ejcts.2006.09.020
2. Harrington G, Russo P, Spelman D, Borrell S, Watson K, Barr W, et al. Surgical-site infection rates and risk factor analysis in coronary artery bypass graft surgery. Infect Control Hosp Epidemiol. 2004;25(6):472-6. DOI: http://dx.doi.org/10.1086/502424
3. Singh K, Anderson E, Harper JG. Overview and management of sternal wound infection. Semin Plast Surg. 2011;25(1):25-33. DOI: http://dx.doi.org/10.1055/s-0031-1275168
4. Ennker IC, Ennker JC. Management of sterno-mediastinitis. HSR Proc Intensive Care Cardiovasc Anesth. 2012;4(4):233-41.
5. Gelijns AC, Moskowitz AJ, Acker MA, Argenziano M, Geller NL, Puskas JD, et al. Management practices and major infections after cardiac surgery. J Am Coll Cardiol. 2014;64(4):372-81. PMID: 25060372 DOI: http://dx.doi.org/10.1016/j.jacc.2014.04.052
6. Yu AW, Rippel RA, Smock E, Jarral OA. In patients with post-sternotomy mediastinitis is vacuum-assisted closure superior to conventional therapy? Interact Cardiovasc Thorac Surg. 2013;17(5):861-5. DOI: http://dx.doi.org/10.1093/icvts/ivt326
7. Graf K, Ott E, Vonberg RP, Kuehn C, Haverich A, Chaberny IF. Economic aspects of deep sternal wound infections. Eur J Cardiothorac Surg. 2010;37(4):893-6. DOI: http://dx.doi.org/10.1016/j.ejcts.2009.10.005
8. Buja A, Zampieron A, Cavalet S, Chiffi D, Sandonà P, Vinelli A, et al. An update review on risk factors and scales for prediction of deep sternal wound infections. Int Wound J. 2012;9(4):372-86. DOI: http://dx.doi.org/10.1111/j.1742-481X.2011.00896.x
9. Morisaki A, Hosono M, Sasaki Y, Hirai H, Sakaguchi M, Nakahira A, et al. Evaluation of risk factors for hospital mortality and current treatment for poststernotomy mediastinitis. Gen Thorac Cardiovasc Surg. 2011;59(4):261-7. PMID: 21484552 DOI: http://dx.doi.org/10.1007/s11748-010-0727-3
1. Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo, SP, Brazil
2. Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo, SP, Brazil
Institution: Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo, SP, Brazil.
Corresponding author:
Samuel Terra Gallafrio
Av. Dr. Enéas de Carvalho Aguiar, 44, 5º Andar, Bloco B - Cerqueira César
São Paulo, SP, Brazil Zip Code 05403-900
E-mail: samuel.gallafrio@gmail.com
Article received: October 14, 2016.
Article accepted: November 15, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter