

Original Article - Year 2017 - Volume 32 -
A novel and simple technique for the treatment of protruding ears
Tratamento da orelha em abano, novas e simples táticas
ABSTRACT
INTRODUCTION: Protruding ears represent a common congenital deformity that can generate psychological implications from childhood. Several surgical techniques have been described to correct this defect; however, clinicians frequently observe the intercurrence of abrupt relief of the posterior crus of the anti-helix and a partial relapse of the original defect. The objective of this study was to demonstrate a surgical technique that minimizes these complications.
METHODS: Sixty-five otoplasties were performed at Mater Dei Hospital, Belo Horizonte, MG, between 1995 and 2015. A surgical instrument similar to a 16-cm hemostatic forceps was developed by the plastic surgery team. All patients were operated under local anesthesia and sedation, under the supervision of an anesthesiologist in a hospital setting.
RESULTS: Correction of the congenital defect was achieved in all cases using a common method that was performed using a simple, novel technique that facilitates surgery and obtains natural and satisfactory results.
CONCLUSION: The proposed techniques for otoplasty of protruding ears are simple, faster, and require easily obtainable and affordable materials. Satisfactory esthetic results were also achieved without observing the stigmas arising from atrial cartilage rupture.
Keywords: Ear/abnormalities; Ear/surgery; Therapeutics; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A orelha de abano é uma deformidade congênita frequente que pode gerar implicações psicológicas desde a infância. Várias táticas cirúrgicas são descritas para correção deste defeito, no entanto, intercorrências frequentemente observadas pela equipe eram a presença de relevos abruptos da cruz posterior da anti-hélice e as recidivas parciais do defeito. O objetivo deste trabalho é demonstrar uma tática cirúrgica que minimiza essas intercorrências.
MÉTODOS: Foram realizadas 65 otoplastias no Hospital Mater Dei, em Belo Horizonte, MG, no período entre 1995 e 2015. Utilizou-se um instrumento cirúrgico elaborado pela equipe de cirurgia plástica, semelhante a uma pinça hemostática de 16 cm. Todos os pacientes foram operados sob anestesia local e sedação assistida por anestesista em ambiente hospitalar.
RESULTADOS: A correção do defeito congênito foi alcançada em todos os casos com o uso de um método comum, mas que cursou com a proposição de táticas novas e simples visando facilitar o ato cirúrgico e adquirir os resultados que foram naturais e satisfatórios.
CONCLUSÃO: As táticas propostas para a cirurgia de otoplastia em abano são simples, de fácil realização, agilizaram o tempo operatório e utilizaram materiais simples, de baixo custo e de fácil aquisição. Também foram alcançados resultados estéticos satisfatórios sem se observar os estigmas decorrentes da quebra da cartilagem auricular.
Palavras-chave: Orelha/anormalidades; Orelha/cirurgia; Terapêutica; Procedimentos cirúrgicos reconstrutivos.
Prominent ears are a frequent familial congenital deformity that are usually bilateral and are characterized by an increase in the cephalo-conchal angle (or an increase in the escafoconchal angle from approximately 90º to 150º or more) and the erasure of the posterior crus of the anti-helix. This latter feature can occur in up to 75% of cases.
Although such deformity does not result in functional changes, the psychological implications since childhood are great and are often noted in the child's psychoemotional profile. The ideal time for surgery is around the age of 7, when the ears are fully formed and of an adult size.
Several approaches have been proposed for this type of surgery and generally have excellent results. However, clinicians frequently observe the intercurrence of abrupt reliefs of the posterior crus of the anti-helix and a partial relapse of the original defect. Thus, we proposed a novel and simply technique that minimizes such problems.
OBJECTIVE
The objective of this study was to demonstrate a surgical procedure that minimizes the intercurrences.
METHODS
A total of 65 otoplasties were performed per convenience sample, including all patients who sought the private clinic of Dr. Ronan Horta, in Belo Horizonte, MG, excluding only those with a prohibitive surgical risk. This surgical technique was used on 26 males and 39 females between 1995 and 2015 in patients with a mean age of 20.35 years.
This technique was developed after observing that the 16 cm hemostatic forceps exhibits a curvature that was similar to that of the posterior crus of the anti-helix. However, the rough and broad serration of the forceps and the width difference in its arms caused us to develop a similar instrument that was more delicate and uniform in width.
Critical evaluation by the plastic surgery team at the Mater Dei Hospital indicated the presence of irregularity in the middle portion of the ear that coincided with the access point of the scalpel for the entry of the hemostatic forceps. Thus, in the small group of patients who exhibited this feature, the upper end of the posterior crus was used as the access point since the natural curvature of the helix would cover this irregularity. All patients underwent operation under local anesthesia and sedation, which were provided by an anesthesiologist in a hospital setting.
After careful administration of anti-septic solution and local anesthesia (0.5% lidocaine and 1:300,000 epinephrine), a tattoo of the path of the posterior crus was drawn using methylene blue dots.
A posterior incision provided access to the auricular cartilage, which was stripped of its perichondrium. At this point, an incision was made in the upper end of the already marked cartilage using a number 11 scalpel (2 to 3 mm), which was followed by detachment of the anterior and posterior skin using delicate, fine-tip scissors.
With this path now free, the modified hemostatic forceps was introduced in an inferior direction with the cartilage being held between the arms of the forceps. In doing so, it was possible to observe the projection of the curvature of the forceps on the new, previously demarcated anti-helix (Figure 1). Pressure movements were performed on the cartilage to reduce its elastic stiffness and create a weakened zone, which, after careful hemostasis, was retro-angled with polypropylene sutures to create the new posterior crus of the anti-helix.

Figure 1. Projection of the forceps.
Then, cephalo-conchal angle closure procedures were performed using conventional techniques, when necessary. Skin synthesis was performed and final dressings were applied, which were removed 48 hours later when the ears were fixed in the mastoid region with small strips of adhesive paper tape. The patients used a containment strip when sleeping in order to avoid occasional folds.
RESULTS
Correction of the congenital defect was achieved in all cases with the use of a common method, but the use of this novel and simple technique, which facilitated surgery and the acquisition of natural and satisfactory results.
There was one case of hematoma, which was identified and drained within the first few hours. Additionally, there was one case of hypertrophic scarring that developed due to an act of aggression experienced by the patient shortly after operation; however, this did not compromise the results. Two other cases of partial and discrete defect recurrence were identified, but they did not trouble the patients to the point where the patient requested further surgery. Table 1 summarizes the characteristics of the patients. Figures 2 and 3 illustrate the pre- and post-operative patient condition following the use of the surgical technique described herein.
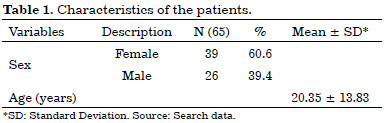

Figure 2. Pre-surgery.

Figure 3. Post-surgery.
DISCUSSION
When attempting to identify novel techniques that facilitate surgery and result in low rates of postoperative complaints, two observations led to the technique that is currently used in our clinic. First, we observed that the curved hemostatic forceps had the same curvature as that of the posterior crus of the anti-helix. Therefore, this technique could be used to create an angulation path by macerating the auricular cartilage in preparation for later suturing and folding, thereby forming the new contour of the posterior crus of the ears.
The second technique, which was created a few years later, followed from the observation that a small break point existed in the auricular cartilage where the two crus of the anti-helix met. Through this point, we could introduce the hemostatic forceps. Given its location in a surgically visible area in the medial portion of the ear, a small incision was made using a scalpel in this section of the cartilage until there was evidence of a break, provided that it did not occasionally show a natural contour.
Thus, we began using this new access point for the creation of the posterior crus, which was covered by the curvature of the upper portion of the helix. Past studies have demonstrated that the best location, as indicated by esthetic results, for an incision is in the groove of the anti-helix fold.
Within the various otoplasty techniques that can be used to correct prominent ears, several procedures have been proposed with the goal of developing a simple and fast technique that produces satisfactory and natural results1-5. In these studies, it was found that otoplasty can be performed in an average of 45 minutes, and therefore, did not lengthen the average time of its execution.
The hemostatic forceps is not a new instrument nor is it difficult to acquire. In addition, it features a curvature that is similar to that of the posterior auricular crus. This shared feature accelerates the surgery, while the subsequent modifications to the forceps allowed for improvements in the width of the instrument and pressure force applied. With these modifications, the forceps are more homogeneous in width throughout the instrument.
A natural look is achieved following weakening, but not breaking, of the auricular cartilage by gentle pressure movements using the modified hemostatic forceps. Damage, such as breaking, can occur when using a scalpel, cartilage scrapes, or even a curette6. In addition, cartilage scraping does not increase the rate of surgical complications, which makes the technique safe.
CONCLUSION
The technique proposed in this study for otoplastic correction of prominent ears is simple, easy to perform, shortens the operative time, and uses simple materials that are affordable and easy to acquire. Satisfactory esthetic results have been achieved without observing the stigmas arising from auricular cartilage rupture that occur in some techniques and that sometimes result in patient complaints of being unable to expose their ears without worrying about discomfort or social stigma7. When compared to the techniques used in other studies, the proposed technique demonstrated a lower rate of recurrence and a better location for scar development8.
COLLABORATIONS
ARHA Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
LRCI Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
MSDP Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
AVCM Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
REFERENCES
1. Furnas DW. Otoplasty. In: Grabb WC, Aston SJ, Smith JW, eds. Grabb and Smith's Plastic Surgery. Philadelphia: Lippincott Raven; 1997.
2. Mustardé JC. The treatment of prominent ears by buried mattress sutures: a ten-year survey. Plast Reconstr Surg. 1967;39(4):382-6. PMID: 5336910 DOI: http://dx.doi.org/10.1097/00006534-196704000-00008
3. Shokrollahi K, Au-Yeung K, Javed M, Sadri A, Molajo A, Lineaweaver W. The discrete scar in prominent ear correction: a digital 3-dimensional analysis to determine the ideal incision for otoplasty. Ann Plast Surg. 2015;74(6):637-8. DOI: http://dx.doi.org/10.1097/SAP.0000000000000421
4. Pitanguy I, Müller P, Piccolo N, Ramalho E, Solinas R. The treatment of prominent ears: a 25-year survey of the island technique. Aesthetic Plast Surg. 1987;11(2):87-93. PMID: 3630840 DOI: http://dx.doi.org/10.1007/BF01575492
5. Stenstrom SJ. A "natural" technique for correction of congenitally prominent ears. Plast Reconstr Surg. 1963;32:509-18.
6. Ruschel FF, Giglio A, Terres M, Weissheimer L, Costa LAL, Ferreira MT, et al. Comparação entre otoplastia com e sem raspagem de cartilagem. ACM Arq Catarin Med. 2007;36(Supl. 1):33-8.
7. Soares PW, Sanches PDC. O uso de condrotripsia na correção da orelha em abano. In: Stocchero IN, Tournieux AB, eds. Atualização em cirurgia Plástica Estética Reconstrutiva. São Paulo: Livraria e Editora Santa Isabel; 1994. p. 255-61.
8. Aki F, Sakae E, Cruz DP, Kamakura L, Ferreira MC. Complicações em Otoplastia: Revisão de 508 Casos. Rev Bras Cir Plást. 2006;21(3):140-4.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Mater Dei, Belo Horizonte, MG, Brazil
Institution: Hospital Mater Dei, Belo Horizonte, MG, Brazil.
Corresponding author:
Leandro Ramalho Chaves Isobe
Rua Martin Luther King, 783, Jardim Lago Parque
Londrina, PR, Brazil Zip Code 86015-300
E-mail: leandro_isobe@hotmail.com
Article received: March 1, 2016.
Article accepted: February 21, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter