

Original Article - Year 2017 - Volume 32 -
Evaluation of 40 rhytidoplasties performed at the Federal Hospital of Andaraí to compare two different techniques: cervicofacial SMAS-plasty according to vector suturing and the sub-SMAS flap approach
Avaliação de 40 ritidoplastias realizadas no Hospital Federal do Andaraí segundo duas técnicas distintas: smasplastia cervicofacial mediante sutura de vetores e retalho subSMAS
ABSTRACT
INTRODUCTION: Rhytidectomy has become one of the most performed aesthetic surgeries in the world. Some surgeons prefer a more conservative approach, and others maintain that aggressive interventions are required to obtain results that are more durable and effective. This study aimed to compare the results of 40 rhytidectomies performed using either of two techniques, namely superficial musculoaponeurotic system (SMAS)-plasty according to vector suturing and the sub-SMAS flap approach, at the Federal Hospital of Andaraí over 22 months.
METHODS: This is a descriptive study that included 20 patients who underwent SMAS-plasty and 20 patients who received a sub-SMAS flap. An assessor identified some variables in specific regions of the face from an aesthetic point of view, and he rated improvements based on photographs obtained before and 6 months after operation. The data collected allowed to quantify complications of both techniques separately.
RESULTS: From an aesthetic point of view, the two techniques showed similar results in terms of facial rejuvenation, improvement of cervical flaccidity, and definition of face/neck transition. The flap provided better results regarding the attenuation in the nasogenian sulcus. A case of hematoma occurred in each technique. Nerve injury occurred in the SMAS-plasty group. However, neither facial nerve injury nor infection occurred in both groups . Edema for >3 months was more prevalent in the sub-SMAS flap group.
CONCLUSIONS: The two methods have advantages and disadvantages, and the best result depended on the degree of aging of the facial skeleton, the loss of supporting tissues in critical areas such as the malar region and next to the labiomandibular fold, the preoperative characteristic of the skin, and the surgeon's experience in the technique.
Keywords: Rhytidoplasty; Rejuvenation; Skin aging; Surgical flaps.
RESUMO
INTRODUÇÃO: A ritidoplastia se tornou uma das cirurgias estéticas mais realizadas no mundo. Alguns preferem uma abordagem mais conservadora e outros defendem que, para obter resultados mais duradouros e efetivos, necessitam de intervenções agressivas. O objetivo é comparar resultados de 40 ritidoplastias realizadas no Hospital Federal do Andaraí ao longo de 22 meses, utilizando duas técnicas distintas, smasplastia mediante sutura de vetores e retalho subSMAS.
MÉTODOS: Trata-se de um estudo descritivo em que 20 pacientes foram submetidas à smasplastia e outras 20 à retalho subSMAS. Um avaliador observou sob o ponto de vista estético algumas variáveis em regiões específicas da face e classificou a melhora baseado em fotografias pré-operatórias e 6 meses após o procedimento. A observação da ficha de coleta de dados possibilitou quantificar as complicações nas duas técnicas separadamente.
RESULTADOS: As duas técnicas demonstraram resultados semelhantes sob o ponto de vista estético com o objetivo de rejuvenescimento facial, melhora da flacidez cervical e definição da transição face/pescoço. Em especial, o retalho proporcionou melhores resultados na atenuação no sulco nasogeniano. Houve um caso de hematoma em cada técnica. Houve uma lesão nervosa na smasplastia. Não houve lesão do nervo facial, nem infecção. Edema superior a 3 meses foi mais prevalente naquelas submetidas ao retalho.
CONCLUSÕES: Os dois métodos possuem vantagens e desvantagens e o melhor resultado depende do grau de envelhecimento do esqueleto facial, da perda de apoio de tecidos frouxos em áreas críticas como a região malar e próxima ao sulco labiomandibular, da característica de pele no pré-operatório e da experiência do cirurgião na técnica empregada.
Palavras-chave: Ritidoplastia; Rejuvenescimento; Envelhecimento da pele; Retalhos cirúrgicos.
One of the major challenges in cosmetic plastic surgery is treatment of facial aging. Signs of aging start to appear from the fourth decade of life. Genetics, quality of life, changes in body mass, type of skin, hormones, diet, smoking, and gravity are the main factors to be considered1.
This process is found from the bone plane, with bone resorption observed in the orbital and malar edges, extending itself to the most superficial planes, with involvement of the ligamentous musculoaponeurotic, subcutaneous, and integumentary tissues2. The literature describes countless conservative approaches and more-invasive treatment techniques for the region of the lower third of the face.
Most conservative authors maintain that superficial musculoaponeurotic system (SMAS) plication alone is adequate to correct the signs of aging while avoiding complications, especially those associated with nerve injury3,4. Some authors put forward a more invasive intervention, with the manufacturing of the SMAS-platysma flap, as it would produce more lasting results5.6.
OBJECTIVE
This study aimed to compare the results of 40 rhytidectomies performed using either of two techniques, at the Federal Hospital of Andaraí, Rio de Janeiro, RJ. Twenty patients underwent SMAS-plasty according to vector suturing, and the other 20 received the SMAS-platysma flap.
METHODS
This is a descriptive study that compared the results of two surgical techniques used in the cervicofacial lift performed by the author. The patients included in this study comprised of those who consulted with the author at the plastic surgery clinic of the Federal Hospital of Andaraí, spontaneously seeking facial rejuvenation surgery.
The main complaints reported in the consultations were rhytids in the lower third of the face, especially in the cervical region, and adipose tissue accumulation lateral to the labiomandibular fold, breaking the linear contour of the jaw. Patients with comorbidities such as hypertension, diabetes, obesity, or other factors that pose risks to their global health were excluded from the study. Patients who smoked or stopped smoking less than 24 months prior to this study were also excluded.
This study was approved by the ethics and research committee of the Federal Hospital of Bonsucesso, under CAAE record No. 56735516.7.0000.5253, and conducted in accordance with the principles of the Declaration of Helsinki. All the patients signed the informed consent form.
A data collection file was made by the author to register information relevant to the study, such as postoperative evolution, period of hospital stay with the drain, and record of possible complications.
The surgeries were performed in female patients aged between 45 and 70 years (mean, 57.5 years), between April 2014 and January 2016. Twenty patients underwent the cervicofacial SMAS-plasty technique according to vector suturing, and the other 20 patients received a sub-SMAS flap.
All the patients received general anesthesia only and local infiltration with 2% lidocaine and adrenaline 1:200,000. In each hemiface, 75 ml of solution was infiltrated, and 50 ml of solution was infiltrated in the neck region, followed by a 10-minute waiting time for vasoconstriction. A 4.8-caliber suction drain was used in all the rhytidoplasties. Hemostasis was performed with a bipolar scalpel to minimize damage to nerve structures and employ radiant thermal action of the monopolar scalpel.
The results were evaluated from the aesthetic point of view by a plastic surgeon, who compared photographs obtained preoperatively and 6 months postoperatively. The parameters considered from the aesthetic aspect were as follows:
• Improvement of the nasogenian sulcus
• Improvement of cervical flaccidity
• Improvement of mandibular contour
• Global facial improvement
The results were classified as very good, good, poor, and very poor. In addition, the observer had no prior knowledge of the surgical technique used for the patient he was assessing.
In addition to the evaluation of aesthetic results, analysis of the data collected allowed to quantify the occurrence of complications such as hematoma, necrosis, blood serum collections, unaesthetic scars, prolonged edema (for over 3 months), infection, and nerve damage in the two patient groups.
Surgical Techniques
Demarcation of the skin
The marking of the flap at the neck region extends 4-5 cm below the angle of the jaw. In the middle third and jowl regions, dissection is limited to 3-4 cm of the labial commissure, where buccal branches become more superficial, running 3 cm parallel with the nasogenian sulcus before reaching the malar fat pad and 2-3 cm from the external bony orbit until it reaches the orbicularis oculi muscles, where it surrounds the lateral orbital rim (Figure 1).
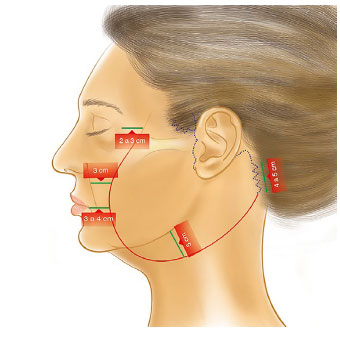
Figure 1. Margins of dissection of the skin flap (red) and dotted areas of incision (blue).
Dissection of the subcutaneous flap first starts at the retroauricular and occipital areas, by using a cold scalpel blade 15 × 2-3 cm in size and scissors. The flap consists of skin with 2 to 3 mm of subcutaneous fat. A small temporal incision is performed, with anterior convexity of approximately 4 cm, cephalic to implantation of the helix.
The incision continues caudally along the implantation of the helix to the tragus, which goes along the edge of the tragus, and then proceeds along the prelobular fold before it goes around the lobe and retroauricular fold. The incision follows the course of the retroauricular fold up to the height of the projection of the tragus. An S-shaped detour is made in the occipital region, following the line of implantation of the occipital hair for approximately 4-5 cm.
In the post-auricular area, the flap is firmly attached to the deep cervical fascia of the sternocleidomastoid and mastoid. As it is the most common site of necrosis, the flap must be detached under direct vision, maintaining the dissection over the underlying deep fascia, always palpating the thickness of the flap to maintain uniformity.
SMAS-plasty technique according to vector suturing
The suturing of the SMAS is performed per five vectors with specific guidelines; two of the vectors are cervical, and three are facial. Vector I is positioned in the midline cervical region to treat bands of the platysma muscle, after submentonian access of approximately 4 cm, situated in a less apparent position, adjacent and parallel to the submentonian fold.
The incision is usually performed in the fold itself or slightly caudally to the fold to remain hidden as much as possible. It includes two lines; each one is positioned on the cutaneous projection of two flanges of the platysma muscle. In patients with a single apparent band, the first demarcation lies on the band and the second lies parallel to it, approximately 3-5 cm away from it.
In the absence of the two flanges, though with flaccidity compromising the mandibulocervical angle, vector I is routinely applied in this technique. The plication of the platysma in the midline extends from the submentonian incision to the upper edge of the thyroid cartilage, performed with separate points and a Monocryl 3.0 thread (Figure 2).

Figure 2. Vector I. Suture of the bands of the platysma muscle approximated in the midline.
Vector II is positioned in parallel, approximately 2-3 cm below the jaw, and fixed in the mastoid. The three facial vectors have the same upper base positioned in the sector closest to the zygomatic arch, with the root of the helix and sideburn, when naturally implanted in women. Vector III, in the highest position of the face, is directed at the midline of the nasogenian sulcus. Vector IV is more easily inclined, following a midline between the corner of the mouth and the edge of the jaw (correction of jowl). Vector V is verticalized and located 1-2 cm far from the line of implantation of the ear, extended on the jaw angle.
Vectors I and V vary according to the degree of sagging, type of containment, and effectiveness of vectors II, III, and IV. Sutures are conducted with simple nylon 3.0 stitching, with the knot inside. Figure 3 shows a schematic representation of the direction of vectors II, III, IV, and V.
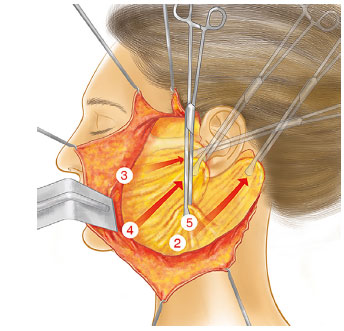
Figure 3. Cervicofacial SMAS-plasty by suturing according to vectors. Positioning of vectors, II, III, IV, and V.
The Sub-SMAS Technique
After the dissection of the subcutaneous plane, the manufacturing of the sub-SMAS flap begins. The incisions for this dissection begin approximately 1 to 2 cm below the zygomatic arch to ensure preservation of the frontal branch of the facial nerve. Such horizontal incision continues for some centimeters ahead until the region where the zygomatic arch joins the body of the zygoma.
A vertical incision is projected along the preauricular region, extending along the anterior border of the sternocleidomastoid until 4-5 cm below the mandibular border (Figure 4). Full release of the SMAS of the zygomatic adhesions is an important aspect in the mobility necessary to superiorly reposition the soft malar tissue.
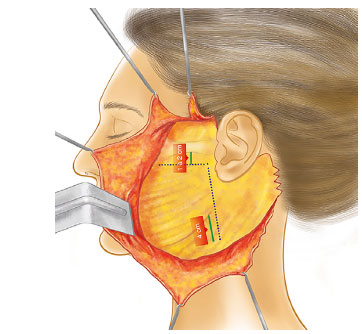
Figure 4. SMAS flap. The dotted area (inverted L) represents the region of the SMAS incised with a cold scalpel.
The dissection of the SMAS flap is interrupted approximately 2 cm anteriorly in relation to the subcutaneous dissection plane in the nasogenian sulcus region. Leaving the adhesions between the skin and the SMAS intact allows resuspension of the anterior facial skin that was not dissected at the time of rotation and fixation of the SMAS. The flap of the malar SMAS is advanced laterally and superiorly over the zygomatic prominence in a direction perpendicular to the nasogenian sulcus.
The malar flap is fixed with a nylon 3.0 thread, employing interrupted sutures, near the zygomatic arch region. The most superomedial portion of the dissection of the SMAS affects the contour around the nasogenian sulcus, whereas the most lateral portion of the dissection of the SMAS is used to re-elevate the fat of the jowl cephalically on the cheek (Figure 5).
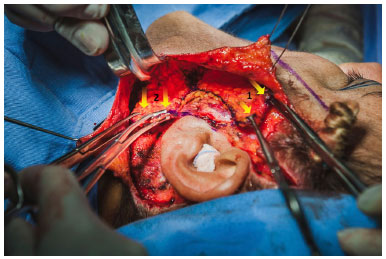
Figure 5. SMAS flap. Division of the SMAS flap at the level of the earlobe, indicated with yellow arrows in 1 to indicate the traction in the region of the zygoma, and in 2 to indicate traction toward the mastoid.
After its division at the level of the earlobe, part of the flap of the SMAS is rotated to the retroauricular region as a transposition flap, with the vector of rotation of this SMAS dissection portion affecting the cervical and submental contours. Fixation of that portion of the flap is performed in the mastoid (Figure 5). The direction of the repositioning of the SMAS face tends to be more cephalic in its orientation, in opposition to the repositioning of the skin flap, which is directed onto a more horizontal vector (Figure 6).
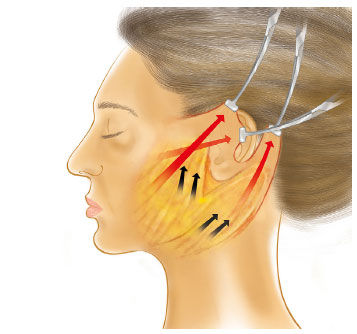
Figure 6. Direction of repositioning of the SMAS (black arrows) and skin flap (red arrows).
The SMAS flap repositioning vectors are determined in accordance with the preoperative evaluation of the patient; however, they are generally more cephalic than the repositioning of the skin flap. The skin flaps are rotated, positioned with a minimum degree of tension applied. The first point of fixation is always fixed in the highest retroauricular region. Then, the excesses of the flaps of the skin are excised with a degree of redundancy between the key points of suture to minimize tension along the incision sites.
RESULTS
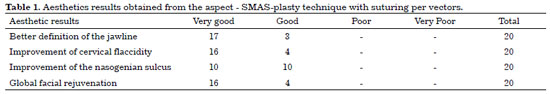
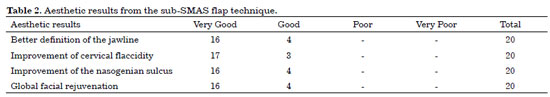
The aesthetics results were preoperatively evaluated by using photographs and postoperatively evaluated after 6 months. This was performed according to improvement in specific points of the face and in the global aspect of facial rejuvenation. Tables 1 and 2 show the results obtained with the two techniques used in this study.
Figures 7 and 8 illustrate the quantitative analysis of the complications, based on the patients' data collection file for the two techniques used.
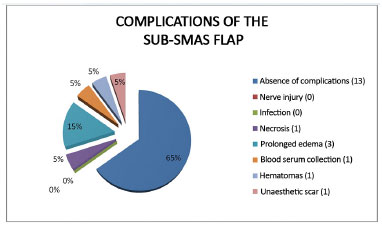
Figure 7. Complications of the SMAS flap.
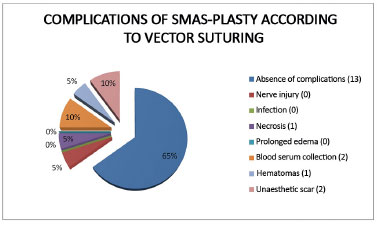
Figure 8. Complications of SMAS-plasty.
The vacuum drain was removed the morning after surgery in 17 patients in the SMAS-plasty group and in 16 patients in the sub-SMAS flap group.
The mean length of hospital stay was 72 hours for 95% of the patients, except for two patients who returned to the surgical center for drainage of hematoma.
The mean surgical duration was 5 hours for SMAS-plasty with plication of the vectors and 6 hours for the sub-SMAS flap approach.
None of the patients had an infection or facial nerve damage.
A case of change in sensitivity of the lobe and external side of the ear occurred in a patient in the SMAS-plasty group.
Figures 9 and 10 illustrate some of the cases included in this study.

Figure 9. A, B and C: Appearance before SMAS-plasty; D, E and F: Appearance 6 months after SMAS-plasty.

Figure 10. A, B, and C: Appearance before SMAS flap placement. D, E and F: Appearance 6 months after SMAS flap placement.
DISCUSSION
The so-called facial rejuvenation surgery has no precise date of emergence, making its first performance quite controversial. The first techniques consisted of resection of skin in the pre-tragus region (preauricular region)7. The results were assessed as poor, with little lasting improvement and possibly scar enlargement7.
Skoog is considered a great innovator of rhytidoplasty, having devised a deeper rhytidectomy approach (subplatysmal plane). In 1968, he developed a flap to elevate the platysma of the cervical region and the lower third of the face. This subplatysmal flap offered an advantage of greater longevity for traction made from deeper structures. This technique was published in 19748,9.
Another fundamental contribution to the evolution of rhytidoplasty originated from the deepening of anatomical knowledge. In 1976, Mitz and Peyronie10 consistently described the SMAS, including radiological and anatomopathological studies. This discovery was of great value because it corroborated the importance of this plane for manufacturing deep flaps in rhytidoplasty.
Some authors strongly criticize the use of more-invasive procedures, as they advocate that the postoperative edema is prolonged and the risk of hematoma is higher. They include as disadvantage the late return of patients to their routine activities. In addition, more-aggressive approaches such as the use of a SMAS flap carry the risk of other complications such as nerve damage and flap necrosis11.
The cervicofacial SMAS-plasty technique according to vector suturing is considered easily reproducible by the authors. Non-mobilization of the SMAS not only reduces surgical trauma but also offers greater safety and long-term efficacy. Other advantages would be reduction of operative time, maintenance of the quality of effects in patients of different age groups, absence of lesions of the facial nerve, and great reduction of the incidence of hematomas and postoperative recovery time. This has motivated authors to execute and indicate the procedure3,4.
Conversely, other researchers advocate that the correct dissection of the SMAS and its elevation allow a safe detachment, traction, lifting, and repositioning of structures in the opposite direction to the tissue injury, thus enhancing surgery efficiency. They indicated that in the dissection of skin flaps, uniform flaps should be obtained during the subcutaneous detachment and surgeons should be attentive as to leave some fat intact along the superficial layer of the SMAS.
If the skin flaps are dissected until no fat is left along the superficial layer of the SMAS, the flaps become more difficult to elevate, thinner, and prone to tear12. According to Stuzin13, the more substantial the SMAS flap, the more frequently better long-term results can be obtained in terms of facial contours. The capacity of re-elevating and re-suspending the facial skin through SMAS rotation produces a better aesthetic result in most patients and preserves part of the peripheral vascularization of the facial skin flap.
In the literature, we found authors who used the SMAS-platysma flap and reported that the incidence of hematoma was much rarer when the plane of dissection was deeper, subcutaneous vessels were absent in the dissection plane above the parotidomasseteric fascia, and the flap was thicker with greater tension. In rhytidoplasty involving two anatomical planes (subcutaneous and sub-SMAS), the bruises are more commonly located in the subcutaneous plane. The disadvantages include a more time-consuming procedure because two surgical planes are developed and longer time for regression of the edema14.
Castro et al.15 reported that the period of observation of late results should be evaluated 4 to 6 months after surgery. During this period, the edema decreases and the scars should not be so apparent. According to the authors, in the absence of complications, postoperative photographs may be performed. In this study, we used the period of 6 months after the procedure to obtain pictures and analysis from an aesthetic point of view by the assessor, who largely considered satisfactory results.
The aesthetic results were similar among the assessors, especially those with the sub-SMAS flap promoting a more significant improvement of the nasogenian sulcus. This might be due to the aesthetic versatility of vectoring of the SMAS in one direction regardless of the repositioning of the skin flap and the superomedial rotation, which best attenuates this region.
The presence of hematoma was registered in this series in 5% of the cases with surgical rapprochement, which is above the average according to the studies of Baker16 in 1983, in which 3.5% of cases presented bruises, and in 2005, along with that of Baker et al.17, in which the presence of bruising occurred in 4.25% of cases.
A patient reported a decrease in sensitivity of the external side and in the earlobe, probably due to a lesion in the great auricular nerve during employment of the of SMAS-plasty technique with suturing per vectors. This corresponds to 2.5% of the cases in this study, which is close to the average described in the literature of approximately 1% to 2%18. Permanent sensory impairment of the ear is usually due to the deep dissection of the average portion of the sternocleidomastoid muscle19.
An edema persisting for 3 months occurred in three patients in the sub-SMAS flap group, which is in line with literature studies that justify a faster regression in subcutaneous rhytidectomies because of the absorptive capacity of the subcutaneous fat. In addition, a less profound lymphatic damage may justify its lower persistence14.
The literature states that cutaneous necrosis presents in 3.6% of subcutaneous rhytidectomies and in 1% of those with a more profound plane of dissection20. The author obtained two cases of cutaneous necrosis, equally divided for each technique proposed in the study. In both cases, the subcutaneous tissue necrosis was related to the formation of hematoma.
The monitoring of patients who participated in this study will be continued for at least 2 years postoperatively to assess and observe the aesthetic results achieved.
CONCLUSION
Most apparently different technical procedures share a common theme. Contour restoration is more predominantly performed by re-elevating facial fat than skin traction. While good results are possible through various techniques, in my opinion, all methods have advantages, disadvantages, and limitations, with the best result always depending on the underlying skeletal support and the quality of the facial soft tissues for each patient.
The key to good results in facial rejuvenation procedures is not the technique used but a combination of preoperative aesthetic analysis, individualization of surgical plan in accordance with the patient's aesthetic needs, and the surgeon's experience in the technique used.
COLLABORATIONS
DVC Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
REFERENCES
1. Riascos A, Baroudi R. A rythidoplasty technique without resultant periauricular scarring. Rev Bras Cir Plást. 2012;27(2):260-5.
2. Hudson DA. An analysis of unsolved problems of face-lift procedures. Ann Plast Surg. 2010;65(2):266-9. DOI: http://dx.doi.org/10.1097/SAP.0b013e3181c2a7bb
3. Letizio NA, Anger J, Baroudi R. Rhytidoplasties: cervicofacial SMAS-plasty according to vector suturing. Rev Bras Cir Plást. 2012;27(2):266-71.
4. Berry MG, Davies DJ. Platysma -SMAS plication facelift. Plast Reconstr Aesthet Surg. 2010;63(5):793-800. DOI: http://dx.doi.org/10.1016/j.bjps.2009.02.067
5. Stuzin JM, Baker TJ, Gordon HL, Baker TM. Extended SMAS dissection as an approach to midface rejuvenation. Clin Plast Surg. 1995;22(2):295-311.
6. Warren RJ. Lifting de face: introdução às técnicas de tecidos profundos. In: Neligan PC, ed. Cirurgia Plástica: Estética, volume 2. Rio de Janeiro: Elsevier; 2015, p. 208-15.
7. Castro CC. Evolução Histórica. In: Castro CC, ed. Cirurgia de Rejuvenescimento facial. Rio de Janeiro: MEDSI; 1998. p. 21-6.
8. Zimbler MS. Tord Skoog: face-lift innovator. Arch Facial Plast Surg. 2001;3(1):63.
9. Skoog T, ed. Plastic Surgery: New Methods and Refinaments. Philadelphia: W.B. Saunders; 1974. 500 p.
10. Mitz V, Peyronie M. The superficial musculoaponeurotic system (SMAS) in the parotid and cheeck area. Plast Reconstr Surg. 1976;58(1):80-8.
11. Menezes MVA, Abla LEF, Dutra LM, Junqueira AE, Ferreira LM. Modified minilifting results: prospective study. Rev Bras Cir Plást. 2010;25(2):285-90.
12. Mendelson BC. Surgery of the superficial musculoaponeurotic system: principles of release, vectors, and fixation. Plast Reconstr Surg. 2002;109(2):824-5. DOI: http://dx.doi.org/10.1097/00006534-200202000-00076
13. Stuzin JM. Rejuvenescimento Facial por meio do sistema musculoaponeurótico superficial: restauração do formato facial com rejuvenescimento facial. In: Aston SJ, Steinbrech DS, Walden JL. Cirurgia Plástica Estética. Rio de Janeiro: Elsevier; 2011. p. 87-99.
14. Hamra ST. Composite Rhytidectomy. Plast Reconstr Surg. 1992;90(1):1-13. PMID: 1615067 DOI: http://dx.doi.org/10.1097/00006534-199207000-00001
15. Castro CC, Aboudib JHC, Gianquino MGC, Moreira MBL. Evaluation of long-term results of rhytidoplasty. Rev Bras Cir Plást. 2005;20(2):124-6.
16. Baker DC. Complications of cervicofacial rhytidectomy. Clin Plast Surg. 1983;10(3):543-62. PMID: 6627843
17. Baker DC, Stefani WA, Chiu ES. Reducting the incidence of hematoma requiring surgical evacuation following male rhytidectomy: a 30-year review of 985 cases. Plastic Reconstr Surg. 2005;116(7):1973-85. DOI: http://dx.doi.org/10.1097/01.prs.0000191182.70617.e9
18. Sanctis MA, Funaro E, Nunes PHF, Passeri LA. Alterações nervosas na ritidoplastia: uma revisão sistemática. Rev Bras Cir Plást. 2014;29(3):450-5.
19. McCollough EG, Perkins SW, Langsdon PR. SASMAS suspension rhytidectomy. Rationale and long-term experience. Arch Otolaryngol Head Neck Surg. 1989;115(2):228-34. PMID: 2643976 DOI: http://dx.doi.org/10.1001/archotol.1989.01860260102023
20. Barton FE Jr. Aesthetic surgery of the face and neck. Aesthet Surg J. 2009;29(6):449-63. DOI: http://dx.doi.org/10.1016/j.asj.2009.08.021
Hospital Federal do Andaraí, Rio de Janeiro, RJ, Brazil
Institution: Hospital Federal do Andaraí, Rio de Janeiro, RJ, Brazil.
Corresponding author:
Diego Vigna Carneiro
Rua Leopoldo, 280 - Andaraí
Rio de Janeiro, RJ, Brazil Zip Code 20541-170
E-mail: diegouffmed@yahoo.com.br
Article received: September 9, 2016.
Article accepted: November 14, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter