

Original Article - Year 2017 - Volume 32 -
Reconstruction of complex lesions of the lower limbs with reverse fasciocutaneous flaps
Reconstrução de feridas complexas de membros inferiores com retalhos fasciocutâneos reversos
ABSTRACT
INTRODUCTION: Complex lesions on the lower limbs have always been challenging because of their difficult resolution. Microsurgical free flaps have been an excellent surgical option; however, they have limited use because there are an insufficient number of clinicians trained in such structured services. Fasciocutaneous flaps, specifically reverse flow, have been shown to be an excellent option in treating lower limb injuries as an alternative to complex microsurgical free flaps.
METHODS: From January 2012 to June 2015, nine patients underwent reconstruction of the lower limbs with reverse fasciocutaneous flaps. All had extensive lesions on these limbs.
RESULTS: In eight patients, the results were satisfactory, and there were no major complications. In one patient, there was total necrosis of the flap.
CONCLUSION: Because of the relative technical simplicity of performing such a technique, fasciocutaneous flaps are a viable option for the reconstruction of complex wounds of the lower limbs and are an additional therapeutic option for patients with these lesions.
Keywords: Surgical Procedures; Reconstructive surgical flaps; Lower extremity; Microsurgery.
RESUMO
INTRODUÇÃO: Lesões extensas em membros inferiores sempre foram desafiadoras devido a sua difícil resolução. Retalhos livres microcirúrgicos se mostraram como excelente opção cirúrgica, todavia, por carecer de equipe capacitada e serviços estruturados, têm seu uso restrito. Os retalhos fasciocutâneos, especificamente os de fluxo reverso, têm se mostrado excelente opção na abordagem de lesões de membros inferiores, numa alternativa aos complexos retalhos livres microcirúrgicos.
MÉTODOS: De janeiro de 2012 a junho de 2015, nove pacientes foram submetidos à reconstrução de membros inferiores com retalhos reversos fasciocutâneos. Todos eram portadores de lesões extensas nos referidos membros.
RESULTADOS: Em oito pacientes o resultado foi satisfatório, sem complicações maiores. Em um paciente houve necrose total do retalho.
CONCLUSÃO: Pela sua relativa simplicidade técnica, os retalhos fasciocutâneos de fluxo reverso vêm se consolidando como opção bastante viável na reconstrução de feridas complexas dos membros inferiores, sendo mais uma opção terapêutica para os pacientes portadores destas lesões.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Retalhos cirúrgicos; Extremidade inferior; Microcirurgia.
Complex injuries of the lower extremities, particularly of the feet and distal region of the leg, are increasingly common, mainly due to the growing number of motorcycle accidents1. The reconstruction of tissue, damaged by these lesions, is essential for the rehabilitation of the patients, bearing in mind that the exposure of tendons, bones, or neurovascular bundles can compromise the viability of these structures2.
For years, free flaps have been excellent therapeutic options for reconstructing complex injuries in the distal region of lower limbs3. However, the lack of skilled teams and structured services for such procedures hampers their routine use.
With the publication by Pontén4 in 1981 and by Masquelet5 in 1992, new technical options were disseminated, including the use of pedicled flaps, for the reconstruction of these injuries. Accordingly, fasciocutaneous flaps gained prominence and are currently commonly used in the reconstruction of tissues, damaged by these injuries5-15.
This type of injury continues to challenge plastic surgeons, with the scarcity of available local tissue to reconstruct the distal region of the lower limb being a major difficulty for such repairs.
The present study describes and discusses the technical options employed in the Plastic Surgery Department of the Hospital das Clínicas, Federal University of Pernambuco (HC-UFPE), in Recife, Pernambuco, using reverse fasciocutaneous flaps for the reconstruction of tissues, damaged by complex lesions of the foot and distal region of the leg.
OBJECTIVE
To describe a series of patients with lesions of the foot and distal region of the leg where reconstruction was performed with different fasciocutaneous flaps.
METHODS
All patients with complex lesions in the foot and distal region of the leg, with exposure of noble structures, and reconstructed with reverse fasciocutaneous flaps were enrolled in the study.
The records and photos of nine patients undergoing this type of reconstruction were analyzed retrospectively.
All patients underwent operation at the Department of Plastic Surgery of HC-UFPE between 2012 and 2015. The operations were performed by three plastic surgeons of the service.
Three flaps were used in reconstructions: reverse sural flap, lateral supramalleolar flap and posterior leg flap. These flaps are briefly described below.
Reverse Sural flap
A skin island was planned on the posterior surface of the leg, between the medial and lateral portions of the gastrocnemius muscle. The height was determined by the distance between the pivot point, 5 cm above the lateral malleolus, and the most distal part to the injury. Incisions were initiated on the top edge of the flap, which continues until the deep fascia, which should compose the flap. The flap was detached from the proximal portion to the distal portion, with the minor saphenous vein and medial sural nerve being identified during dissection and included in the flap5-9.
Lateral Supramalleolar flap
This flap must be prepared with a pivot point 5 cm from the lateral malleolus, where the perforating branch of the fibular artery penetrates the interosseous membrane10. During the marking, the anterior and posterior limits of the flap are the tendon of the tibialis anterior muscle and the medial aspect of the fibula, respectively. The flap was dissected in the subfascial plane while maintaining the integrity of the superficial fibular nerve.
Posterior calf flap
This is a bidepicular flap, with a pivot point located about 10 cm above the medial malleolus, and about 12 cm above the lateral malleolus11,12. The skin island was planned on the posterior surface of the leg. The incision was initiated at the upper border of the flap, dissecting the subfascial plane to the pivot point, which was the site of concentration of septal cutaneous vessels of the flap (medially, perforators of the posterior tibial artery, and, laterally, perforators of the fibular artery). During dissection, the medial sural nerve and the saphenous vein were visualized and sectioned. These structures were maintained in the flap.
The pedicle of the flaps was sectioned on the third or fourth postoperative week, where it could then be resutured to the donor area and grafted at the time of surgery.
RESULTS
Eight male patients and one female patient underwent surgery in this series. Their ages ranged from 22 to 66 years, with an average of 38.5 years.
The average size of the lesions was 27.2 cm2, ranging from 16 cm2 to 48 cm2.
Eight reconstructions were successful, with one minor complication. One case with distal epidermolysis was conducted on an outpatient basis, without generating any impairment to the viability of the flap.
Figures 1 and 2 show the intraoperative planning steps involving in creating a reverse sural flap and the late result of 5 months reconstruction of a neoplasm lesion.
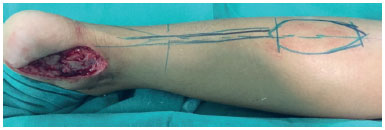
Figure 1. Oncologic wound in the medial calcaneal region and reverse sural flap planning.

Figure 2. Five months postoperative outcome of reverse sural flap.
Figures 3, 4, and 5 show the reconstruction of a chronic injury on the dorsum of the foot using the lateral supramalleolar flap. Note a slight distal epidermolysis on the flap.

Figure 3. Chronic wound on the dorsum of the foot and dissected supramalleolar flap.

Figure 4. Intermediate time of lateral supramalleolar flap showing slight distal epidermolysis.

Figure 5. Postoperative result 30 days after grafting of donor area.
As shown in Figure 6, which shows the planning involved in creating a posterior leg flap, an initial shorter marking and a subsequent longer marking are used to improve the suitability of the flap for transposition without tension. Figures 7 and 8 show the result before the section of the pedicle and the result 6 months later.
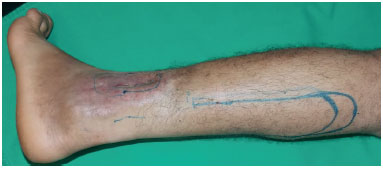
Figure 6. Traumatic wound with bone exposure in the distal third of the leg and planning of the posterior thigh flap.

Figure 7. Intermediate time point after creation of the posterior thigh flap.

Figure 8. End result of posterior thigh flap after 6 months.
There was one case that evolved into total necrosis of the flap, which was treated with debridement, wound dressings, and skin grafting, after tissue granulation of the base of the lesion 67 days after debridement.
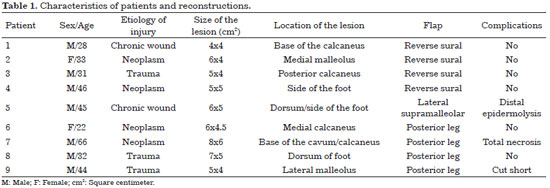
The characteristics of patients and reconstructions are presented in Table 1.
DISCUSSION
Treatment of complex lesions of the foot and distal region of the leg is difficult and prolonged, often requiring multiple surgeries and a multidisciplinary team. An early and efficient approach can prevent functional sequelae to the affected limb.
Free flaps are an excellent option for reconstruction of extensive foot lesions in order to provide abundant and richly vascularized tissue. The use of free flaps is advantageous in infected wounds, with osteomyelitis or delayed bone healing, due to its abundant vascularization and easier filling of dead spaces. However, it has the drawback of requiring experienced staff, adequate equipment, and longer surgical time13. The Plastic Surgery Service of the HC-UFPE performs such procedures in selected cases; however, currently, in the majority of cases, it has opted for fasciocutaneous flaps.
The circulation of fasciocutaneous flaps of the lower limbs is based on myocutaneous perforators: the fasciocutaneous arteries and the arteries from the intermuscular septa. Among these, flaps of the reverse flow type have gained greater relevance, since they are a good option in the reconstruction of the distal region of the lower limbs.
The vascular pedicle of these flaps derives from the septocutaneous perforating vessels that arise from the fibular and posterior tibial arteries. The posterior tibial artery, through its perforating vessels, dominates the posteromedial portion of the distal third of the leg. While the fibular artery, through its septocutaneous branches, dominates the posterolateral side14,15.
Considering the anatomical axis of the main vessels of the leg, one can empirically plan the longitudinal axis of the flap. The perforator closest to the margin of the lesion should be chosen to be the pivot point, since the position of the latter will define the final length of the flap. These perforating arteries are more likely to be located in a region four to seven centimeters above the malleolus, being the ideal pivot point for rotating the flap16.
Some studies mention the use of Doppler ultrasound for vascular mapping and identification of perforating branches of the main arteries17,18. This examination was not conducted in the surgical procedures presented in this study.
The Reverse Sural flap, described by Donski and Fogdestam14 in 1983, is widely used for reconstruction of the soft tissues of the lower third of the leg and foot. Moderate to large defects can be covered with this flap19. This flap has a wide rotation arc, compared with other regional flaps, and does not require the sacrifice of any essential vascular trunk for its preparation since its vascular supply arises from perforating branches of the common fibular artery13. Its pivot point is located about 5.0 cm superior and laterally to the lateral malleolus5-9.
El-Shazly and Yassin20 recommend fixing a pivot point about 7 cm above the lateral malleolus to provide greater vascular safety for the flap. However, most studies still recommend a pivot point of 5 cm above the lateral malleolus.
The flap used in the series by Chang et al.21 had dimensions of 25 cm x 10 cm (H x W). In our series, the largest flap was 21 cm x 7 cm2.
The presence of the vein is crucial to decreasing the chance of venous congestion. To cover the donor area, skin grafting may be used. It is important that this flap is not subjected to pressure or other mechanical forces, so as not to compromise the viability of the flap.
The lateral supramalleolar flap, as well as the reverse sural flap, also provides good coverage for lesions in the distal third of the leg and foot. Its vascularization is based on the anastomosis of the arterial arcade around the ankle with perforating branches of the fibular artery, which emerge from the interosseous membrane approximately 5 cm from the lateral malleolus. This anastomosis emits cutaneous branches at this point that anastomose with the plexus that accompanies the superficial fibular nerve, which, in turn, constitutes the septocutaneous territory of the anterior tibial artery22,23.
Venous congestion is more common in this flap given that it does not carry any major vein, which contributes to venous drainage of the flap24. This venous flow is obtained by valve insufficiency through the pressure gradient itself, the communicating capillary, and the collateral veins24.
In our series, this flap was used in a patient with a lesion located on the dorsum of their foot. We believe that this flap is quite satisfactory in the reconstruction of small to moderate lesions in the anterior or posterior region of the distal third of the leg and in the dorsal region of the foot because it is an easily reproducible option that involves an easy anatomical dissection that does not interfere in the possible construction of other flaps10.
The posterior fasciocutaneous leg flap, unlike previous flaps, has a higher pivot point in relation to the malleolus (10 cm from the medial malleolus and 12 cm from the lateral malleolus). This flap, initially described by Monteiro Júnior et al.11, associates concepts described by Donski and Fodgestan14, who, in 1983, described a similar flap that was based only on septocutaneous vessels originating from the fibular artery, with the flap based on septocutaneous vessels of the posterior tibial artery, as described by Amarante et al.15 in 1986. Given that it is a bipediculate flap, greater circulatory safety is guaranteed. It further enables the possible use of longer flaps that are capable of covering defects in the more distal topography of the lower limb in patients with comorbidities11.
As shown in the diagram, detailing flap planning, an initial marking that is smaller in length and a subsequent, longer marking provides greater convenience for transposition of the flap without tension. It is always important that the flap be slightly longer than is required.
All of these flaps described herein have constant vascularization and are safe for vascular supply. Even rotations of up to 180 degrees appear not to affect their vascular viability25.
The clinical condition of the patients interferes in the viability of the flap, particularly in the viability of the reverse sural flap. Comorbidities, such as hypertension, diabetes mellitus, peripheral arterial occlusive diseases, advanced age and obesity, are the main risk factors for failure with reverse flaps 26.
There is still no consensus in the literature regarding which flap type would be the most appropriate for a particular type of defect or location of the lesion. The surgeon's experience is important in choosing the type of flap.
Total necrosis of the flap in the posterior region in this series increased the risk of major complication development (11%). This necrosis occurred in the older patient from this series. This patient was 66 years old and smoked regularly. These factors may have contributed to the failure of the surgery.
Although the use of reverse fasciocutaneous flaps is well established in the literature, their use to treat distal lower limb lesions still causes uncertainty in most plastic surgeons. It is important that plastic surgeons have a greater knowledge of this important therapeutic option, considering its large clinical applicability and relative technical ease. When compared to free flaps, the ease of this technique demonstrates the feasibility of using reverse fasciocutaneous flaps in the restoration of complex lesions of the lower limbs.
In the patients reported in this series, the reverse flaps of the lower limbs were shown to be an excellent option for the reconstruction of complex foot and distal leg lesions.
COLLABORATIONS
RA Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
FAMAB Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
JZS Completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
ACCRB Completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
GTS Analysis and/or interpretation of data; completion of operations and/or experiments.
REFERENCES
1. Brasil. Ministério da Saúde. Sistemas de Informações Hospitalares do SUS (SIH-SUS). Morbidade Hospitalar do SUS por Acidentes de Transporte por Local de Internação de 2008-2010. [acesso 2017 Fev 13]. Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sih/cnv/fiuf.def
2. Rezende MR, Rabelo NTA, Benabou JE, Wei TH, Mattar Junior R, Zumiotti AV, et al. Cobertura do terço distal da perna com retalhos de perfurantes pediculados. Acta Ortop Bras. 2008;16(4):223-9. DOI: http://dx.doi.org/10.1590/S1413-78522008000400007
3. Hallock GG. Distal lower leg local random fasciocutaneous flap. Plast Reconstr Surg. 1990;86(2):304-11. DOI: http://dx.doi.org/10.1097/00006534-199008000-00018
4. Pontén B. The fasciocutaneous flap: its use in soft tissues defects of the lower leg. Br J Plast Surg. 1981;34(2):215-20. PMID: 7236984 DOI: http://dx.doi.org/10.1016/S0007-1226(81)80097-5
5. Masquelet AC, Romana MC, Wolf G. Skin island flaps supplied by the vascular axis of the sensitive superficial nerves: anatomic study and clinical experience in the leg. Plast Reconstr Surg. 1992;89(6):1115-21. DOI: http://dx.doi.org/10.1097/00006534-199206000-00018
6. Masquelet AC, Gilbert A. Atlas colorido de retalhos na reconstrução dos membros. Rio de Janeiro: Revinter; 1997. p. 160-6.
7. Nakajima H, Imanishi N, Fukuzumi S, Minabe T, Fukui Y, Miyasaka T, et al. Accompanying arteries of the lesser saphenous vein and sural nerve: anatomic study and its clinical applications. Plast Reconstr Surg. 1999;103(1):104-20. PMID: 9915170 DOI: http://dx.doi.org/10.1097/00006534-199901000-00018
8. Almeida MF, da Costa PR, Okawa RY. Reverse-flow island sural flap. Plast Reconstr Surg. 2002;109(2):583-91. DOI: http://dx.doi.org/10.1097/00006534-200202000-00027
9. Vendramin FS. Retalho sural de fluxo reverso: 10 anos de experiência clínica e modificações. Rev Bras Cir Plást. 2012;27(2):309-15. DOI: http://dx.doi.org/10.1590/S1983-51752012000200023
10. Batista JC. Retalho supramaleolar de fluxo reverso: aplicações clínicas. Rev Bras Cir Plást. 2011;26(1):140-6. DOI: http://dx.doi.org/10.1590/S1983-51752011000100025
11. Monteiro Júnior AA, Alonso N, Gomes CB, Lemos R, Ferreira MC. Reparação de perdas cutâneas na perna e no pé com retalho fasciocutâneo de pedículo distal. Rev Bras Cir Plast. 1991;6(1-2):33-40.
12. de Almeida OM, Monteiro AA Jr, Neves RI, de Lemos RG, Braz JC, Brechtbuhl ER, et al. Distally based fasciocutaneous flap of the calf for cutaneous coverage of the lower leg and dorsum of the foot. Ann Plast Surg. 2000;44(4):367-73. DOI: http://dx.doi.org/10.1097/00000637-200044040-00003
13. Franco D, D'Avila F, Arnaut Junior M, D'Avila B, Franco T. Tratamento das áreas cruentas de perna com retalhos locais. Rev Bras Cir Plást. 2015;30(2):264-72.
14. Donski PK, Fogdestam I. Distally based fasciocutaneous flap from the sural region. A preliminary report. Scand J Plast Reconstr Surg. 1983;17(3):191-6. PMID: 6673085
15. Amarante J, Costa H, Reis J, Soares R. A new distally based fasciocutaneous flap of the leg. Br J Plast Surg. 1986;39(3):338-40. DOI: http://dx.doi.org/10.1016/0007-1226(86)90043-3
16. Yang D, Morris SF. Reversed sural island flap supplied by the lower septocutaneous perforator of the peroneal artery. Ann Plast Surg. 2002;49(4):375-8. DOI: http://dx.doi.org/10.1097/00000637-200210000-00007
17. Hasegawa M, Torii S, Katoh H, Esaki S. The distally based superficial sural artery flap. Plast Reconstr Surg. 1994;93(5):1012-20. DOI: http://dx.doi.org/10.1097/00006534-199404001-00016
18. Imanishi N, Nakajima H, Fukuzumi S, Aiso S. Venous drainage of the distally based lesser saphenous-sural veno-neuroadipofascial pedicled fasciocutaneous flap: a radiographic perfusion study. Plast Reconstr Surg. 1999;103(2):494-8. PMID: 9950536 DOI: http://dx.doi.org/10.1097/00006534-199902000-00020
19. Ayyappan T, Chadha A. Supersural neurofasciocutaneous flaps in acute traumatic heel reconstructions. Plast Reconstr Surg. 2002;109(7):2307-13. DOI: http://dx.doi.org/10.1097/00006534-200206000-00022
20. El-Shazly M, Yassin O. Increasing the success rate of the reversed flow fasciocutaneous island sural flap: a clinical experience in 26 cases. Ann Plast Surg. 2006;57(6):653-7. DOI: http://dx.doi.org/10.1097/01.sap.0000235475.74372.67
21. Chang SM, Zhang F, Yu GR, Hou CL, Gu YD. Modified distally based peroneal artery perforator flap for reconstruction of foot and ankle. Microsurgery. 2004;24(6):430-6. DOI: http://dx.doi.org/10.1002/micr.20069
22. Whetzel TP, Barnard MA, Stokes RB. Arterial fasciocutaneous vascular territories of the lower leg. Plast Reconstr Surg. 1997;100(5):1172-83. DOI: http://dx.doi.org/10.1097/00006534-199710000-00016
23. Saad FT, Almeida KG, Almeida PYNG, Silva TF, Balbuena MB, Coutinho BBA, et al. Reconstrução de dorso de pé com retalho supramaleolar lateral de fluxo reverso em menor de 4 anos de idade. Rev Bras Cir Plást. 2015;30(2):324-8.
24. Wee JT. Reconstruction of the lower leg and foot with the reverse-pedicled anterior tibial flap: preliminary report of a new fasciocutaneous flap. Br J Plast Surg. 1986;39(3):327-37. PMID: 3730678 DOI: http://dx.doi.org/10.1016/0007-1226(86)90042-1
25. Demir A, Acar M, Yldz L, Karacalar A. The effect of twisting on perforator flap viability: an experimental study in rats. Ann Plast Surg. 2006;56(2):186-9. PMID: 16432329 DOI: http://dx.doi.org/10.1097/01.sap.0000196561.92828.d7
26. Parrett BM, Pribaz JJ, Matros E, Przylecki W, Sampson CE, Orgill DP. Risk analysis for the reverse sural fasciocutaneous flap in distal leg reconstruction. Plast Reconstr Surg. 2009;123(5):1499-504. PMID: 19407622 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181a07723
1. Hospital das Clínicas, Universidade Federal de Pernambuco, Recife, PE, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Hospital das Clínicas, Universidade Federal de Pernambuco, Recife, PE, Brazil.
Corresponding author:
Rafael Anlicoara
Av. Prof. Moraes Rego, 1235 - Cidade Universitária
Recife, PE, Brazil Zip Code 50670-901
E-mail: rafaelanlicoara@hotmail.com
Article received: June 7, 2016.
Article accepted: February 3, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter