

Original Article - Year 2017 - Volume 32 -
Comparison between surgical sutures and Prineo® in terms of esthetic result and scar formation
Comparação de resultado estético em cicatrizes com uso de fios cirúrgicos e Prineo®
ABSTRACT
INTRODUCTION: Wound healing is a well-organized, directed process of tissue repair. The process can be expedited using topical glues and adhesives, which offer a non-invasive, easily removable alternative to suturing. Furthermore, such products have good tensile strength and involve lower application time. In particular, the Prineo® adhesive is applied to a polyester mesh that covers the wound.
METHOD: We carried out a retrospective, cross-sectional study, with subsequent statistical analysis , involving 101 surgical procedures in which wound closure was performed using either nylon sutures or Prineo®. All the procedures were performed between 2012 and 2014.
RESULTS: Six patients had contact dermatitis after Prineo® was used, with statistical significance (p = 0.042). Furthermore, Prineo® decreased the rate of scar enlargement (p < 0.05) . There was no statistical difference between the Prineo® and suture groups in terms of scar quality (p = 0.068); in both groups, the scar result was mostly excellent (87 %) to good (27%).
CONCLUSION: Patients whose wounds were closed using Prineo® a system involving octyl-2-cyanoacrylate and an associated polyester mesh displayed lower rates of scar enlargement, which depended on whether the thickness of the dermis was satisfactory. However, the same patients had higher rates of contact dermatitis than those whose wounds were closed using surgical sutures. Both groups showed excellent to good scar quality, with no significant difference in terms of esthetic scar results.
Keywords: Healing; Wounds and injuries; Sutures; Nylons; Tissue adhesives.
RESUMO
INTRODUÇÃO: Cicatrização de ferida é um processo bem organizado que tem como finalidade a reparação tecidual completa. Colas e adesivos tópicos oferecem uma alternativa não invasiva, de retirada fácil e espontânea; boa força tênsil; menor tempo de aplicação, sendo o Prineo® uma cola adesiva associada a uma malha de poliéster aplicados sobre a ferida.
MÉTODO: Trata-se de um estudo transversal retrospectivo com análise de 101 procedimentos cirúrgicos no período de 2012 a 2014, nos quais a síntese da ferida operatória ocorreu com fios cirúrgicos de náilon ou Prineo®, sendo aplicada análise estatística.
RESULTADOS: Neste estudo, seis pacientes apresentaram dermatite de contato ao uso do Prineo® com significância estatística (p = 0,042). O uso desse sistema diminuiu a taxa de alargamento cicatricial (p < 0,05). O presente trabalho não apresentou diferença estatística (p = 0,068) na qualidade da cicatriz entre os pacientes que utilizaram Prineo® em relação ao grupo controle, demonstrando que em ambos os grupos o resultado cicatricial foi de excelente (87%) a bom (27%) na sua maioria.
CONCLUSÃO: Conclui-se no estudo que os pacientes que utilizaram o sistema de octil-2-cianocrilato associado a malha, Prineo®, apresentaram menores índices de alargamento cicatricial, dependentes de uma espessura de derme satisfatória, e maiores taxas de dermatites por contato em relação àqueles em que a ferida foi encerrada com fios cirúrgicos. Os dois grupos demonstraram qualidades cicatriciais excelentes a bons, sem diferença estatística em tais resultados estéticos cicatriciais.
Palavras-chave: Cicatrização; Ferimentos e lesões; Suturas; Nylons; Adesivos teciduais.
Wound healing is a well-organized tissue repair process in which platelets, keratinocytes, macrophages, microcirculation, and fibroblasts play key roles in restoring tissue integrity. The ultimate end of wound healing is to restore the structural and functional integrity of the skin. The success of this process depends partly on the personal characteristics of the patient, which clinicians cannot influence. However, good wound closure techniques also affect the outcome1.
Wound closure materials should primarily ensure good coaptation of the wound edges until the tissue heals. Premature failures of various types of wound closure can result in separation of the edges, which can lead to esthetically unpleasant scarring2. Furthermore, if the edges of the suture are incorrectly positioned, or if they are too tense, growth of epidermis inside the wound along the suture may cause fibrous tissue development. Loss of traction of the suture (degradation) before the scar has been properly consolidated can also cause changes in the wound3.
Topical adhesives offer an non-invasive alternative to sutures; they have the following advantages: (1) spontaneous removal from the system, bringing comfort to the patient; good tensile strength; antimicrobial barrier; non-invasive application and shorter implementation time; reduced post-operative pain, edema, and hyperemia due to less trauma in the dermis4,5.
Cyanoacrylate was first used for wound closure in 1959, having been approved by the Food and Drug Administration (FDA) of the United States (USA). In 2008, the FDA reclassified it from class III to class II; thus, it could be marketed in the USA5. Cyanoacrylate possesses strength equivalent to that of non-absorbable sutures and intra-dermal Monocryl® 4-06; its tension and malleability depend on the length of the alkyl chains.
Prineo® is a dual system comprising a polyester mesh and a 2-octyl cyanoacrylate skin adhesive; the latter has long alkyl chains, imparting high flexibility and a resistance to rupture, with low toxicity6. When applied to the wound, the cyanoacrylate initiates an intense molecular reaction in which the monomers become organized and polymerize quickly; when they come into contact with traces of water, they bind to the stratum corneum and thus to keratinocytes7.
Surgical complications, such as infection, dehiscence, and delayed healing continue to be a problem, with significant associated morbidity and high treatment costs8. Thus, this study aimed to compare conventional surgical sutures with the Prineo® system in terms of the healing of surgical wounds after plastic surgery; we analyzed intrinsic and extrinsic factors related to the healing process.
OBJECTIVE
To compare, 1 year after surgery, surgical sutures with 2-octyl cyanoacrylate (Prineo®) in terms of wound healing results in patients who had undergone abdominoplasty or mammoplasty between 2012 and 2014. All procedures were performed by the same surgeon.
METHODS
This was a cross-sectional study involving retrospective analysis of 101 cases of abdominoplasty and mammoplasty; all procedures were performed by the same surgeon at the Daher Lago Sul Hospital, Brasilia, DF, between 2012 and 2014. By analyzing clinical reports and pictures, we compared two groups of patients; in both groups, the subdermal plane was closed using simple 4-0 nylon sutures.
However, in the intradermal plane, the surgical wound was closed using either Prineo® (Group 1) or a Monocryl® 4-0 suture (control group). The Prineo® dressing was removed after 21 days in all cases. The quality of surgical wound infection was analyzed using medical records, as well as pre- and post-operative photos. The following complications were analyzed in the same way: infection, hyperchromia, enlargement and hypertrophy, dehiscence, necrosis, etc. Comorbidities such as diabetes mellitus and smoking were also assessed. Age, gender, skin color, and skin characteristics were studied and analyzed in both groups; in this way, the factors associated with a good and a poor wound healing were investigated.
The results were analyzed by the chi-square (χ2) test, the t-test, or Fisher's exact test, where appropriate.
The two groups were homogeneous in that they were organized according to similarities in physical biotype, such as skin color (using the Fitzpatrick classification), Body Mass Index (BMI), skin texture, and comorbidities.
The authors had no conflicts of interest, and the study followed the principles of the Helsinki Declaration, adopted by the 18th World Medical Association General Assembly, Helsinki, Finland, in June 1964 and corrected by the 29th World Medical Association General Assembly, Tokyo, Japan, in October 1975, the 35th World Medical Association General Assembly, Venice, Italy, in October 1983, and the 41st World Medical Association General Assembly, Hong Kong, in September 1989.
RESULTS
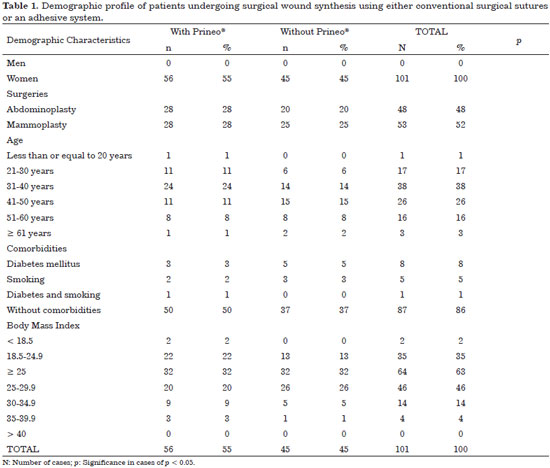
The demographic data of the study detail 101 surgical procedures performed from 2012 to 2014: 48 abdominoplasties and 53 mammoplasties; surgical closure was performed using either the Prineo® or surgical Monocryl® sutures; the patient distribution was homogeneous across all procedures, as described in the Methods a (Table 1).
All procedures were carried out in women, with 31-40 years being the most prevalent age group. The frequency of the comorbidities diabetes mellitus and smoking were low 3% and 2%, respectively. These did not significantly influence the esthetic end result of the scars. This fact can be ascertained by considering only the cases of active disease.
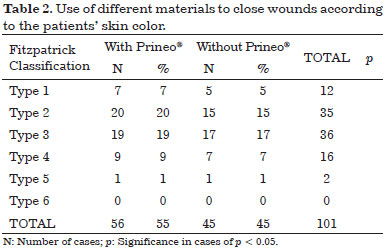
Most of the patients (63%) had a BMI between 25 and 29.9 kg/m2, classifying them as pre-obese (Table 1). With regards to skin color (using the Fitzpatrick classification), there was no statistical difference between the groups, indicating that skin color had no involvement in the final result of the scar (Table 2).
The thickness of the dermis, another variable described in the study, was significantly associated with the final result of the scar (p = 0.01; Table 3). Furthermore, there was a significant difference between the groups in terms of surgical complications: six cases of allergy occurred in the Prineo® group (p = 0.042; Figure 1), while scar enlargement was more frequent in the suture group, occurring in eight cases (p = 0.042; Table 4 and Figure 2).
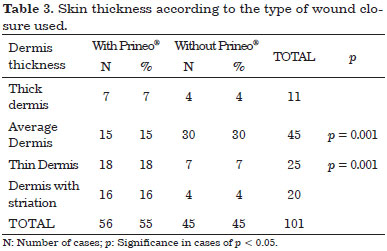
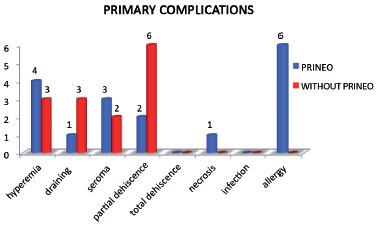
Figure 1. Graph showing that Prineo® caused an allergic reaction in 6% of all patients who underwent surgery, with statistical significance.
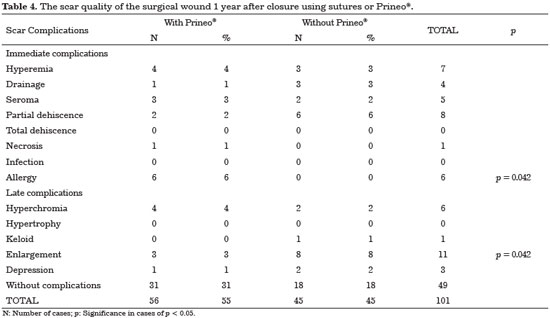
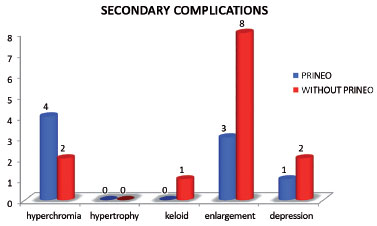
Figure 2. Graph demonstrating that scar enlargement mostly occurred in patients whose wound was closed using nylon 4-0 surgical sutures.
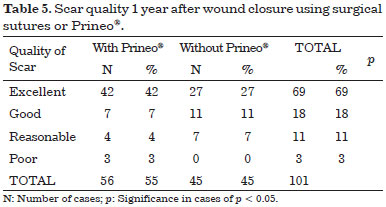
Both the Prineo® and conventional suture groups displayed good to excellent (18% and 69%, respectively) results in terms of the esthetic end result of the scar 1 year after surgery; there was no significant difference between the groups in this regard (Table 5).
DISCUSSION
The ideal suture material must display the following characteristics: ease of handling, minimal tissue reaction, adequate resistance to traction, hypoallergenicity, and low cost9. Prineo® technology consists of two components: a polyester mesh to connect the edges of the wound, and a surgical liquid adhesive (octyl-2-cyanoacrylate) which closes the wound.
Topical adhesives offer some advantages; for example, easy and quick application, good tensile strength along the wound, an antimicrobial barrier, and less pain during removal10,11.
In the present study, all patients (n = 101) were women aged between 31 and 40 years; at this age, the women had already borne children and were concerned about aging (Table 1). There was no significant difference between the groups in terms of smoking and diabetes, even though these factors negatively influence the healing process (Table 1).
The quality of a scar depends on racial characteristics, such as color and thickness of the dermis; usually, better scarring, from a cosmetic perspective, occurs in patients with lighter skin12. In this study, the skin color and thickness were homogeneous in both groups (Tables 2 and 3; Figure 3). Furthermore, considering hyperemia, hyperchromia, depressions, seroma, and dehiscence, there was no difference in the final quality of the scar between the groups (p > 0.05; Table 5). However, the thickness of the dermis around the wound did influence the final outcome of the scar (p = 0.001; Table 3).
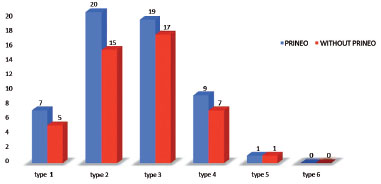
Figure 3. Patients of both groups were grouped homogeneously according to the color of their skin, defined using the Fitzpatrick classification.
Surgical wound infection is a serious complication, and both in vivo and in vitro studies suggest that polyester mesh has an antibacterial protection of up to 75%9. In the present study, there was no significant difference between the two groups in terms of infection, because antisepsis and antibiotic prophylaxis were administered to all patients (Table 4).
The Prineo® system is indicated in cases of longer wounds that involve higher tension; it distributes the tension more easily while maintaining a traction equivalent to that of 4-0 Monocryl®9. Our statistical analysis showed in agreement with the literature that this system decreases the rate of scar enlargement (p < 0.05; Table 4; Figures 4 and 5).
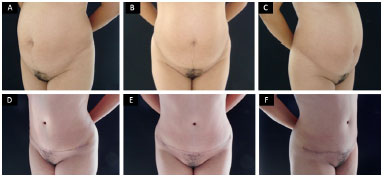
Figure 4. A, B, C: Patient in the preoperative period; D, E, F: Same patient 1 year after surgery for abdominoplasty using the Prineo® system; no scar enlargement can be seen.
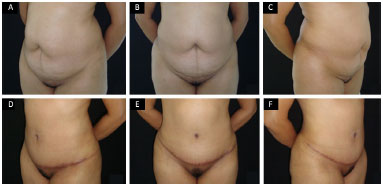
Figure 5. A, B, C: Patient during the pre-operative period; D, E, F: Same patient 1 year after surgery for abdominoplasty, when the wound was closed using with nylon; scar enlargement occurred during the post-operative period.
Contact between cyanoacrylate and the skin causes a polymerization reaction, releasing formaldehyde, which is probably what caused dermatitis in some patients in the present study4. Specifically, six patients developed contact dermatitis after Prineo® use. This was a significant number (p = 0.042); however, all the affected patients improved after clinical treatment, and the final scar result was not affected (Table 4; Figures 1 and 6).

Figure 6. A, B, C: Patient during the pre-operative period; D, E, F: Same patient in the post-operative period after mammoplasty, with wound closure performed using the Prineo® system. Initial phase of hyperemia (above) and late phase of hyperchromia (below) after allergic reaction of the skin.
There was no significant difference between the groups (p = 0.068) in terms of scar quality, indicating that, in both groups, the scarring result was mostly excellent (87%) to good (27%; Table 5 and Figure 7).
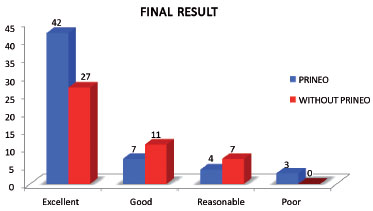
Figure 7. Graph showing that, despite the complications in each group, the esthetic result of the scar after 1 year was similar, with no significant difference between the two groups.
CONCLUSION
Patients whose wounds were closed using Prineo® a system involving octyl-2-cyanoacrylate and an associated polyester mesh displayed lower rates of scar enlargement, which depended on whether the thickness of the dermis was satisfactory. However, the same patients had higher rates of contact dermatitis than those whose wounds were closed using surgical sutures. Both groups showed excellent to good scar quality, with no significant difference in terms of esthetic scar results.
COLLABORATIONS
MC Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
LGM Analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
IRJ Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
RQL Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
CMA Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
LMCD Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
DASS Analysis and/or interpretation of data; completion of operations and/or experiments.
MCAG Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
FTM Statistical analysis.
JCD Analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
REFERENCES
1. Demidova-Rice TN, Hamblin MR, Herman IM. Acute and impaired wound healing: pathophysiology and current methods for drug delivery, part 1: normal and chronic wounds: biology, causes, and approaches to care. Adv Skin Wound Care. 2012;25(7):304-14. DOI: http://dx.doi.org/10.1097/01.ASW.0000416006.55218.d0
2. Issac C, Ladeira PRS, Rêgo FMP, Aldunate JCB, Ferreira MC. Physiological wound healing. Rev Med (São Paulo). 2010;89(3/4):125-31.
3. Silverstein P. Smoking and Wound Healing. Am J Med. 1992;93(1A):22S-24S. DOI: http://dx.doi.org/10.1016/0002-9343(92)90623-J
4. Bowen C, Bidinger J, Hivnor C, Hoover A, Henning JS. Allergic contact dermatitis to 2-octyl cyanoacrylate. Cutis. 2014;94(4):183-6. PMID: 25372253
5. Huemer GM, Schmidt M, Helml GH, Shafighi M, Dunst-Huemer KM. Effective wound closure with a new two-component wound closure device (PrineoTM) in excisional body-contouring surgery: experience in over 200 procedures. Aesthetic Plast Surg. 2012;36(2):382-6. DOI: http://dx.doi.org/10.1007/s00266-011-9819-4
6. Kent A, Liversedge N, Dobbins B, McWhinnie D, Jan H. A prospective, randomized, controlled, double-masked, multi-center clinical trial of medical adhesives for the closure of laparoscopic incisions. J Minim Invasive Gynecol. 2014;21(2):252-8. DOI: http://dx.doi.org/10.1016/j.jmig.2013.10.003
7. Sachse MM, Junghans T, Rose C, Wagner G. Allergic contact dermatitis caused by topical 2-octyl-cyanoacrylate. Contact Dermatitis. 2013;68(5):317-9. DOI: http://dx.doi.org/10.1111/cod.12027
8. Janis JE, Kwon RK, Lalonde DH. A practical guide to wound healing. Plast Reconstr Surg. 2010;125(6):230e-44e. PMID: 20517064 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181d9a0d1
9. Hung SH, Tseng TM, Hsu HT, Tseng H. Adhesive strength of ethyl-2-cyanoacrylate tissue adhesive: how strong is it? Surg Today. 2014;44(5):927-32.
10. Huemer GM, Schmidt M, Helml GH, Shafighi M, Dunst-Huemer KM. Effective wound closure with a new two-component wound closure device (PrineoTM) in excisional body-contouring surgery: experience in over 200 procedures. Aesthetic Plast Surg. 2012;36(2):382-6. DOI: http://dx.doi.org/10.1007/s00266-011-9819-4
11. Parvizi D, Friedl H, Schintler MV, Rappl T, Laback C, Wiedner M, et al. Use of 2-octyl cyanoacrylate together with a self-adhering mesh (DermabondTM PrineoTM) for skin closure following abdominoplasty: an open, prospective, controlled, randomized, clinical study. Aesthetic Plast Surg. 2013;37(3):529-37. DOI: http://dx.doi.org/10.1007/s00266-013-0123-3
12. Taylor SC. Skin of color: biology, structure, function, and implications for dermatologic disease. J Am Acad Dermatol. 2002;46(2 Suppl):S41-62. DOI: http://dx.doi.org/10.1067/mjd.2002.120790
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Daher Lago Sul, Brasília, DF, Brazil
3. Sociedade Brasileira de Anestesiologia, Rio de Janeiro, RJ, Brazil
Institution: Hospital Daher Lago Sul, Brasília, DF, Brazil.
Corresponding author:
Marcela Caetano Cammarota
SMHN, Quadra 2, Bloco C, Ed Crispim, sala 1315
Brasília, DF, Brazil Zip Code 70710-149
E-mail: marcelacammarota@yahoo.com.br
Article received: January 24, 2016.
Article accepted: February 3, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter