

Original Article - Year 2017 - Volume 32 -
Minilipoabdominoplasty with umbilicus detachment: indications and comparison of surgical tactics for umbilicus reintegration, an prospective study
Minilipoabdominoplastia com desinserção umbilical: indicações e comparação de táticas cirúrgicas para reinserção de umbigo, estudo prospectivo
ABSTRACT
INTRODUCTION: The minilipoabdominoplastia with umbilicus detachment represents a surgical procedure restricted to cases in which isolated liposuction would cause worsening of sagging skin, while the conventional abdominoplasty would imply excessive skin resection. It allows xyphopubic plication of the rectus abdominis muscle and good resection of the excessive lower abdominal skin. The objective is to provide patients with high umbilucus treated with liposuction, mini-abdominoplasty with umbilucus detachment and reinsertion below, and comparison of two techniques for umbilical reinsertion.
METHODS: We included six women aged 32- to 50-year-old and who underwent surgery under spine and general anesthesia from January to June 2013 in the Hospital of the Federal University of Triângulo Mineiro, Uberaba, Minas Gerais, Brazil.
RESULTS: After surgery, patients had natural silhouettes of body contours and umbilicus repositioned without external scars.
CONCLUSION: The technique used allows treatment of moderate sagging skin of upper and lower abdomen with need of a small incision, the technique provides umbilicus scarring without external scarring and less chance of complications due to the small detachment.
Keywords: Umbilicus; Abdominoplasty; Abdominal wall; Cicatrix.
RESUMO
INTRODUÇÃO: A minilipoabdominoplastia com desinserção do umbigo representa uma tática cirúrgica restrita àqueles casos nos quais a lipoaspiração isolada causaria piora da flacidez, enquanto a abdominoplastia convencional implicaria em ressecção exagerada de pele. Permite plicatura xifopúbica dos retos abdominais e boa ressecção do excedente cutâneo abdominal inferior. O objetivo é apresentar pacientes com umbigo alto tratados com lipoaspiração, miniabdominoplastia com desinserção de umbigo e reinserção abaixo, e comparar duas técnicas para reinserção umbilical.
MÉTODOS: Foram operadas seis pacientes no período de janeiro a junho de 2013 no Hospital Escola da Universidade Federal do Triângulo Mineiro (UFTM), Uberaba, MG, todas do sexo feminino, com idades de 32 a 50 anos, submetidas à anestesia peridural e geral.
RESULTADOS: Pós-operatórios com contornos corporais de silhuetas naturais e cicatrizes umbilicais reposicionadas sem cicatrizes externas.
CONCLUSÃO: A técnica empregada permite o tratamento da flacidez moderada do abdome superior e inferior com uma incisão menor, proporciona cicatriz umbilical sem cicatriz externa e menores chances de complicações em virtude do menor descolamento.
Palavras-chave: Umbigo; Abdominoplastia; Parede abdominal; Cicatriz.
The body contouring contitutes an aesthetic and functional pattern that varies each time and today is very relevant. Deformities and dysfunctions of this contour lead to limitations in people's affective and social relationships. The body contouring surgery aims to give back self-esteem to individuals of a positive body image.
The mini-lipoabdominoplasty with umbilicus detachment is a restricted surgical technique for cases in which the isolated liposuction causes a deterioration of the sagging skin, while conventional exaggerated abdominoplasty would involve skin resection. The mini-abdominoplasty would treat only the lower abdomen sagging skin, leaving the excessive supraumbilical skin, and maintaining the umbilicus in its original position that would possess an undesirable effect of lower traction scar with "sad" aspect of the umbilicus.
The combination of liposuction with selective detachment of the diastasis area of rectus abdominis and umbilical detachment allow to perform a complete xyphopubic plication of the rectus abdominis and resection of the excessive skin over the lower abdomen, adding a treatment to the upper abdominal skin laxity.
Historic
Since 1899, several authors have described their techniques on abdominoplasty, with tactical variants that collaborate with the experts. Recently, Kelly1 described a horizontal elliptical resection with skin, subcutaneous tissue and umbilicus. In the following years we observe the evolution of abdominoplasty:
1906 - Babcok2,3 presented transverse and vertical resections, although without giving importance to the umbilicus;
1909 - Weinhold4 showed his technique with resection in three points of star shape;
1931 - Flesch-Tebbesius and Weinscheimer5 made a infraumbilical transverse resection, with triangular flap to preserve the umbilicus;
1939 - Thorek6,7 lowed the level of the scar of Flesch-Tebbesius and Weinscheimer, and preserved the umbilicus;
1940 - Somalo8 described the belt resection and perhaps he was the first to use the term dermolipectomy;
1942 - Thorek made the resection of epigastric fat presenting the inverted dermolipectomy;
1953 - Fournier9 presented horizontal elliptical resection;
1955 - Galtier10 preserved the umbilicus through resection cross;
1960 - Gonzales-Ulloa11 described his circular resection technique with sacrum and pubic triangle;
1964 - Pontes described his resection technique in block of all excessive skin located in the hypogastrium shaped ellipse;
1965 - Callia made an incision on the pubis with lateral extensions, which started to be used by surgeons;
1967 - Pitanguy12,13 made low horizontal incision with the ends outward and downward;
1970 - Franco14 and Rebello15 accomplished dermolipectomia with submammary incision called inverted abdomen;
1975 - Sinder16,17 published the abdomen tagging with triangle, removing only the bottom flap after the upper flap detachment positioning then the scar;
1978 - Planas18 described techniques similar to the Sinder, who called it "vest over pants";
1978 - Psillakis19 described the treatment of muscle-aponeurotic sagging, making the suture of the large oblique muscle on the fascia of the rectus abdominis muscle;
1980 - Yves Gerard Illouz20 presented for the first time in Brazil, at the Brazilian Congress of Plastic Surgery in Fortaleza, the liposuction technique, which allied the team of the abdominal dermolipectomias for a more satisfactory aesthetic result of body contouring;
1985 - Hakme and Wilkinson associated liposuction to partial abdominoplasty, calling it minilipoabdominoplastia and miniabdominoplasty;
1985 - Avelar21,22 described the association liposuction with abdominoplasty for patients with protruding abdomen, fat located above and below the umbilicus and muscle weakness;
1987 - Castro et al. published a work in order to avoid complications related to retail in miniabdominoplasty;
1998 - Baroudi23,24 et al. advocated the use of points from the xiphoid to the bottom edge of the pubic incision lines and columns.
2000 - Matarasso described the association of abdominoplasty with liposuction in order to protect the blood supply to the abdominal flap;
2000 - Avelar21,22 published his work of liposuction associated with abdominoplasty without detachment;
2001 - Saldanha25,26 et al., and Avelar, on its parallel work, released abdominoplasty techniques, without detachment, introducing lipoabdominoplastias techniques in our field;
2003 - Bozola27 emphasized the classification of cosmetic changes in the treatment of abdomen with their specific treatments;
2004 - Munhoz28 and Graf29 described the importance of perforating arteries in lipoabdominolplastia through Doppler flowmetry;
2007 - Resende published a Plastic Surgery in obesity compendium with valuable techniques for obese and former obese.
2008 - Uebel30 described the lipoabdominoplasty with removal of abdominal flap infraumbilical block, preserving a range of Scarpa's fascia and resection of suprapubic flap by superficial incision to the subcutaneous tissue.
These and other authors established the basic principles of abdominoplasty performed nowadays. With the advent of liposuction, this technique started to complement abdominoplasty, improving body contouring.
Matarasso classifies the abdomen into four categories, while Bozola and Psillakis28 classified into five groups.
I - Without excessive skin, with fat located in the lower part of the abdomen, normal muscle without diastasis.
II - Small or medium excessive infraumbilical skin with excessive adipose tissue and poorly distributed.
III - Small or medium excess of infra-umbilical skin and adipose tissue with small or moderate excess, with moderate upper and lower abdominal diastasis.
IV - Skin excess and adipose tissue and diastase the entire length of the abdominal musculature with high insertion umbilicus.
V - Excess skin marked in the upper and lower level, excess fat and diastasis of the rectus muscles and or obliques. Hernia carriers patients may be encompassed in this group. The umbilicus has low or regular insertion.
With this simple classification, we can indicate the procedure that most suits each case.
OBJECTIVE
To present a combination of surgical procedures for abdominal lipodystrophy treatment associated with moderate skin laxity and umbilicus high position associated with liposuction, miniabdominoplasty with umbilicus detachment and umbilicus reposition. In addition, the analysis and comparisons of two different techniques for the umbilicus reintegration will be present.
METHODS
Six women aged 32-50 years old underwent surgery under spinal and general anesthesia from January to June 2013 at the Hospital das Clínicas of the Federal University of Triângulo Mineiro, Uberaba-MG, Brazil. All patients signed the consent form. This study followed the principles of the Declaration of Helsinki.
The technique consists of the initial marking at the suprapubic incision, 5-7 cm from vulvar rhyme with variable length from 6 to 12 cm on each side of the abdominal midline as suggested by Baroudi, but more curvilinear (Figure 1).
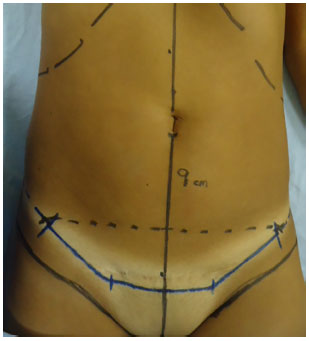
Figure 1. Suprapubic surgical incision marking - miniabdo-minoplasty.
The procedure initiated with the liposuction of back and flanks with the patient in prone position, and later shift to the supine position for liposuction all anterior abdomen in shallow and deep plan. We used the wet technique, infiltrating epinephrine solution 1: 500,000 in proportion 1: 1. After that, a curvilinear suprapubic incision was performed ranging from 12 to 24 cm, depending on amount of excessive skin. A supra aponeurosis detachment into the umbilicus was also performed (Figure 2).
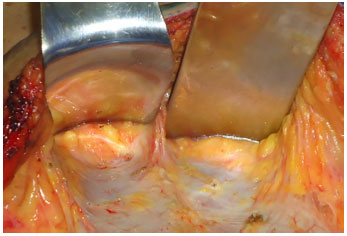
Figure 2. Supra-aponeurotic displacement until the umbilical scar.
The nave is detached (Figure 3). Initially we passed an x point with nylon 2.0 in the umbilicus the insertion point in the aponeurosis, and just below of this fixed suture an incision is made in the umbilicus detachment, which keeps connected to the abdominal flap.
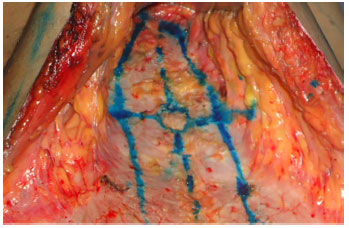
Figure 3. Marking of rectus abdominis muscle, and umbilical desinsertion.
This maneuver facilitates an exposure to supraumbilical detachment. Often a small opening in the aponeurosis arises and must be repaired with suture, avoiding future hernias of the abdominal wall. A restricted selective detachment to the medial edge of the rectus abdominis was done and it allowed the correct view of the area of muscle diastasis and subsequent plication xyphopubic of the rectus abdominis (Figure 4). This can be done with X inverted points with nylon 2.0, as well as continuous running anchor suture, with interruptions every 3 cm. The plication includes the old area of the umbilical pedicle.
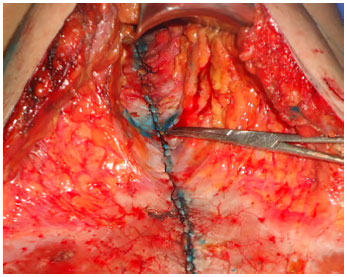
Figure 4. Aspect after xifo-pubic plicature of rectus bdominis muscle.
The next step involved the reinsertion of the umbilicus in the aponeurosis, which usually occurs 2-5 cm below the original position by 1 to 2 cm above the imaginary line passing through the anterior superior iliac spines (Figures 5 and 6). Special attention should be taken to avoid the inadequate low positioning of the umbilicus, leaving an unaesthetic appearance. This traction also allows improving of the upper abdominal skin laxity. Another important aspect to observe is the midline centralization during plication in order to avoid the umbilical reinsertion in an improper position with subsequent lateralization umbilicus, which is complication described in this type of surgery.
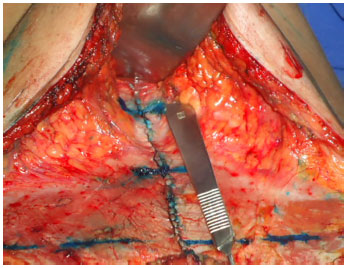
Figure 5. Umbilical reinsertion local, between 2 to 5 cm below original position.
Figure 6. Fixation of umbilical scar in aponeurosis.
We describe bellow two different manners for umbilical reinsertion in the aponeurosis, the results will be compared later.
The first way is carried out with 3 points arranged longitudinally (Figure 7), the first being the upper margin of the umbilicus, the other at the midpoint, and the last at the lower end of the umbilicus, allowing a more vertical appearance (Figures 8 and 9). The other technique used for umbilicus fixation includes 5 points, 4 cardinal points and a central point (Figure 10), ensuring a more circular appearance (Figures 11, 12, 13 and 14).
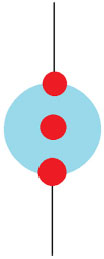
Figure 7. Umbilical reinsertion scheme with 3 fixing points, used in figures 8 and 9.

Figure 8. A and B: Before surgery; C and D: 6 months after surgery.
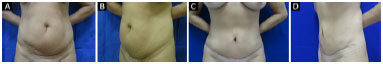
Figure 9. A and B: Before surgery; C and D: 6 months after surgery.
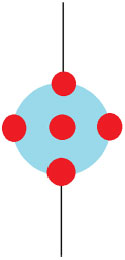
Figure 10. Umbilical reinsertion scheme with 5 fixing points, used in figures 11, 12, 13 and 14.

Figure 11. A and B: Before surgery; C and D: 6 months after surgery.

Figure 12. A and B: Before surgery; C and D: 6 months after surgery.

Figure 13. A and B: Before surgery; C and D: 6 months after surgery.

Figure 14. A and B: Before surgery; C and D: 6 months after surgery.
The highest number of points would be responsible for lower risk of detachment and the umbilicus fluctuation. The more practical sequence to perform this suture would be first the uppermost point, after the central, followed by side, and finally the bottom, for technical facility. In both cases we use U points with nylon 3.0 for suture.
Finally, we performed resection of surplus skin under slight traction and skin accommodation without tension (Figures 15 and 16). Baroudi´s points of contention are done with Vycril 3.0, and it does not enabled drainage. The suture is performed in 3 planes, subcutaneous, subdermal and intradermal (Figure 17).

Figure 15. Flap showing excessive skin.

Figure 16. Aspect after removal of excessive skin of abdominal flaps.

Figure 17. Final aspect after suture in 3 planes (subcutaneous, subdermal, and intradermal).
We use elastic compression garment from the immediate postoperative period for 60 days. Deep venous thrombosis prophylaxis used nonpharmacologic measures such as intermittent pneumatic compression stockings and early ambulation. In all cases antibiotic prophylaxis is mandatory, led by Cefazolin 2 g for 24 hours and treatment with cefadroxil for seven days. Another post-operative key care is the use of anatomical umbilical silicone orthosis to mold the umbilicus and keep it fixed to deep planes, over a period of two months.
RESULTS
The minilipoabdominoplastia with umbilical detachment has selective surgical indication and requires observance of surgical time, trained staff, early ambulation, lymphatic drainage application and use of elastic mesh. Postoperatively, there was a natural body contouring silhouette with evidence to waistlines, results that generated satisfaction for surgical patients and staff, with improved self-esteem and great benefit in social and professional aspects.
Among the complications associated with this technique are residual laxity in the upper abdomen, lower positioning of the umbilicus, lateralization of the umbilicus, scaring changes, and asymmetry and irregularities more associated with liposuction. The reported cases presented complications such as low positioning of the umbilicus in longilineal, and another case with lateralization of the umbilicus due to asymmetry. These tow complication were observations pointed out by surgical team and, but not complaints of patients who expressed satisfaction with the result. No other major complications were described.
When two techniques for rehabilitation of the umbilicus were compared, both proved to be effective, with good contour, aesthetically acceptable result. The greatest benefit was the the absence of external umbilical scar. The difference between both techniques was only the long term umbilicus format, one circular and one vertical. The decision of technique to be used may be based on individual preference of the type of umbilicus considered more aesthetical to the patient.
DISCUSSION
Aesthetic changes in abdominal wall can be easily corrected by isolated liposuction, only if there´s no abdominal skin laxity. The approach is also easy when dealing with patients with major abdominal volume and massive skin laxity over the conventional tuck or lipoabdominoplasty.
The umbilicus has been studied and described in a number of approaches by external incision as well as the release of the umbilicus of his aponeurotic deployment and subsequent reintegration. A thorough preoperative evaluation of abdominal addressed to the adipose tissue, the skin, the muscles, the position of the umbilicus and the abdominal scar is critical to diagnose, classify and correctly indicate the best technique for each case.
Liposuction is the technical basis to dissect and improve abdominal silhouette. The selective detachment and retail liposuction decrease surgical trauma, preserve perforating arteries and minimize dead space, replacing the large detachment of conventional abdominoplasty, the lipectomies, and reduce complications such as bruises, epiteliosis and necrosis of the skin30.
Another favorable factor is the fixing of the retail dermoadiposo the aponeurotic plane, by the adhesion points, providing significant reduction in tensile forces exerted by the flap over the pubic scar that reduces the incidence of dehiscence, misplacement and extended scars compared with traditional surgeries. Traction is also an important predisposing factor in the development of hypertrophic scars. Reduced traction exerted by the flap on the pubic scar showed significantly lower incidence of hypertrophic scars.
Minilipoabdominoplastia is a conservative technique that, anatomically, dissects and shapes the abdomen in plans with less surgical trauma, repositions and corrects all layers and structures of the abdominal region.
When we evaluate the high umbilucus, we take into account the landmarks: the umbilicus center and superior implementation of pubic hairiness (which may vary according to the body shape of the patient). Typically this distance should measure around 16 cm or more. It can be said that the umbilicus is the only scar in the body that individual wishes to possess and complains when it is not presented or eliminated.
The lack of umbilicus causes a severe dysmorphia, leading to impairment of own body image, with psychological consequences that could not be disregarded. The histological study of the umbilicus deployment area in the abdominal wall proved the absence of vessels which could permeable by nourishing the umbilical area or surrounding areas of the abdominal wall above the relevant tissue to the annulus fibrosus31.
This nutrition is ensured by minimum vessels and/ or imbibition through the peritoneal structures, which enables preservation of the umbilicus even in cases where it is "skeletonized", for example, in myocutaneous retail surgery of rectus muscle, situation which the umbilical pedicle is literally naked, bound only by their subsequent aponeurosis base and coated internally by umbilicus peritoneal.
A umbilicus scar has a rounded shape, depressed and deeper at the top. Its external and top is limited by rodete skin. For this reason, the edges are high, and the lower edge more flat, forming a smooth transition to the skin of the abdominal wall. In the bottom of the cavity, in its middle zone, an elevation (nipple) is seen that center corresponds to the scar of the umbilical cord.
Around the nipple there is a so-called umbilical groove circular depression that separates the nipple skin rodete. The attachment of the umbilicus in the abdominal wall allows clear delineation of the abdomen in two segments: an upper and lower abdomen. It is also important to remember about presence of superficial circumflex iliac arteries that help in flap security.
Both abdomen are accentuated by the depression of the umbilical region and, in the majority of young women, the lower abdomen is slightly more prominent and higher. According to Goss32, the umbilicus is the vertebrae L3 and L4. Dubuov33 studied the umbilicus situation in 100 non-obese patients, selected randomly, placed on supine position and found that in 96% of cases umbilicus position coincides with the imaginary horizontal line joining the iliac crests.
Despite considerable advances in lipoabdominoplastias with neoumbilicus, we observed that scars generated by these surgeries marking are still stigmatizing. In miniabdominoplastias, where there is detachment and reattachment of the umbilicus in the aponeurosis, the remaining orifice of the umbilical pedicle section always needs to be sutured and plicated in the midline, at least in mesoumbilical region, which turns it necessary to open detachment.
This maneuver may lateralized the umbilicus in the midline, even by taking all care in rehabilitation, since the plication may have little lateral deviation. Not always the original umbilicus shows satisfactory results in miniabdominoplasties in which there is no detachment of the umbilical pedicle and traction only the infraumbilical skin because the umbilicus does not allow supraumbilical skin to be tensioned and present good accommodation. In addition, fair-supraumbilical skin laxity and shape of the umbilicus, as the "sad umbilicus" (horizontal spindle) remain when there is no procedure to lower it in miniabdominoplasties.
This technique variation, in addition to provide greater security, enables patients to return to their normal activities after 15-30 days, without the need of forced bending positions (Fowler position). The low scar, which can be covered with clothes, as well as preservation of original patient's umbilicus aspect are two essential factors for the patients to decide to perform mini-lipoabdominoplasty.
CONCLUSION
The minilipoabdominoplastia with umbilical detachment and its umbilical reinsertion options is a valid technique to treat moderate skin laxity of the upper abdomen and lower with an incision with acceptable size. It does not present umbilical external scar, avoiding stigma. Still, it has low rate of complications compared to conventional abdominoplasty, and it constitutes an optional technique for the aesthetic treatment of the abdomen.
COLLABORATIONS
LRCCT Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
VTPP Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents.
MTRC Final approval of the manuscript.
MAOM Final approval of the manuscript.
MPSN Final approval of the manuscript.
CRRC Final approval of the manuscript.
TGMGS Final approval of the manuscript.
AGM Final approval of the manuscript.
JPS Final approval of the manuscript; writing the manuscript or critical review of its contents.
REFERENCES
1. Kelly HA. Excision of the fat of the abdominal wall lipectomy. Surg Gynecol Obstet. 1910;10:229-31.
2. Babcok WW. Plastic reconstruction of the female breasts and abdomen. Am J Surg. 1939;43(2):268-78. DOI: http://dx.doi.org/10.1016/S0002-9610(39)90845-7
3. Babcok WW. The correction of the obese and relaxed abdominal wall, with special reference to the use of buried silver chain. Am J Obstr. 1916;74:596-611.
4. Weinhold. Zentralb F Gynäk. 38, 1332-1909. Apud: Thorek M. Plastic surgery of breast and abdominal wall. Springfield: Charles Thomas, 1942.
5. Flesch-Thebesius e Weinscheimer. Chirurg. 1931;3:841. Apud: Thorek M. Plastic surgery of breast and abdominal wall. Springfield: Ch. Thomas; 1942.
6. Thorek M. Modern operative technique. London: Lippincott Phil; 1939.
7. Thorek M. Plastic surgery of breast and abdominal wall. Springfield: Charles Thomas; 1942.
8. Somalo M. Dermolipectomia circular del tronco. Sem Med. 1940;47:435.
9. Fournier M. Lipectomia abdominal. Cir Cir. 1953;21(8):443-8.
10. Galtier H. Traitment chirurgicale de l'obesité de la paroi abdominale avec ptose. Mem Acad Chir (Paris). 1955;81(12-13):341-4.
11. Gonzales-Ulloa M. Belt lipectomy. Br J Plast Surg. 1960;13:179-86. DOI: http://dx.doi.org/10.1016/S0007-1226(60)80035-5
12. Pitanguy I. Abdominoplastias. O Hospital. 1967;71(1):541-56.
13. Pitanguy I. Surgical reduction of the abdomen, thigh, and buttocks. Surg Clin North Am. 1971;51(2):479-89. PMID: 5550702 DOI: http://dx.doi.org/10.1016/S0039-6109(16)39391-4
14. Franco T, Rebello C. Abdominoplastia - Nem sempre uma cirurgia simples. Med Hoje. 1977;638-44.
15. Rebello C, Franco T. Abdominoplastia por incisão submamária. Rev Bras Cir. 1972;62:249-52.
16. Sinder R. Cirurgia Plástica do abdômen: técnica pessoal de abdominoplastia, com prévio descolamento de retalho supra-umbilical e uso de retalho dermoadiposo, VI International Congress of Plastic and Reconstrutive Surgery, Paris, França, 25 de agosto de 1975. Apud Rev Bras Cir. Plást. 2009;24(3):336-44.
17. Sinder R. Detalhe da técnica citada no livro de Cirurgia Estética de Talita Franco e Cláudio Rebello. Capítulo 9 (Abdominoplastia). Rio de Janeiro/ São Paulo: Atheneu; 1977. p.277.
18. Planas J. The "vest over pants" abdominoplasty. Plast Reconstr Surg. 1978;61(5):694-700. PMID: 643956 DOI: http://dx.doi.org/10.1097/00006534-197805000-00005
19. Psillakis JM. Abdominoplasty: some ideas to improve results. Aesthetic Plast Surg. 1978;2(1):205-15. DOI: http://dx.doi.org/10.1007/BF01577954
20. Illouz YG. Une nouvelle technique pour les lipodystrophies localisées. Rev Chir Esth Franc. 1980;6(9).
21. Avelar JM. Abdominoplasty combined with lipoplasty without panniculus undermining: abdominolipoplasty--a safe technique. Clin Plast Surg. 2006;33(1):79-90. DOI: http://dx.doi.org/10.1016/j.cps.2005.08.007
22. Avelar JM. Abdominoplasty without panniculus underming and resection. 1a ed. São Paulo: Hipócrates; 2002. DOI: http://dx.doi.org/10.1067/maj.2002.121961
23. Baroudi R, Keppke EM, Netto FT. Abdominoplasty. Plast Reconstr Surg. 1974;54(2):161-8. PMID: 4276452 DOI: http://dx.doi.org/10.1097/00006534-197408000-00007
24. Baroudi R. Management of the umbilicus in abdominoplasty. Presented at Society of Aesthetic Plastic Surgery: Newport Beach; 1973.
25. Saldanha OR, De Souza Pinto EB, Mattos WN Jr, Pazetti CE, Lopes Bello EM, Rojas Y, et al. Lipoabdominoplasty with selective and safe undermining. Aesthetic Plast Surg. 2003;27(4):322-7. PMID: 15058559 DOI: http://dx.doi.org/10.1007/s00266-003-3016-z
26. Saldanha OR, Pinto EB, Matos WN Jr, Lucon RL, Magalhães F, Bello EM. Lipoabdominoplasty without undermining. Aesthet Surg J. 2001;21(6):518-26. PMID: 19331937 DOI: http://dx.doi.org/10.1067/maj.2001.121243
27. Bozola AR, Psillakis JM. Abdominoplasty: a new concept and classification for treatment. Plast Reconstr Surg. 1988;82(6):983-93. PMID: 2974166 DOI: http://dx.doi.org/10.1097/00006534-198812000-00008
28. Munhoz AM, Kamamoto F, Saito FL, Menezes M, Gemperli R. Mapeamento anatômico dos vasos perfurantes abdominais e aplicação clínica no tratamento de deformidades estéticas da parede abdominal pela lipoabdominoplastia. In: Sadanha O, ed. Lipoabdominoplastia. Rio de Janeiro: Di-Livros Editora; 2004. p. 104-14.
29. Graf R, Freitas R, Fisher M, Bark A, Loureiro A, Pianowski R, Cruz GA. Lipoabdominoplastia - estudo de fluxometria doppler e variação técnica. In: Saldanha O, ed. Lipoabdominoplastia. Rio de Janeiro: Di-Livros Editora; 2004. p. 87-92.
30. Uebel CO. Lipoabdominoplasty: revisiting the superior pull-down abdominal flap and new approaches. Aesthetic Plast Surg. 2009;33(3):366-76. PMID: 19296152 DOI: http://dx.doi.org/10.1007/s00266-009-9318-z
31. Saldanha OR, Azevedo DM, Azevedo SFD, Ribeiro DV, Nagassaki E, Gonçalves Junior P, et al. Lipoabdominoplastia: redução das complicações em cirurgias abdominais. Rev Bras Cir Plást. 2011;26(2):275-9. PMID: 17524650 DOI: http://dx.doi.org/10.1590/S1983-51752011000200014
32. Goss CM. Grays Anatomy of the Human Body. Philadelfia: Lea and Fabinger; 1965.
33. Dubuo RT. Chirurgie Plastique de L'Abdomen. Paris: Mason; 1971.
1. Universidade Federal do Triângulo Mineiro, Uberaba, MG, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Hospital das Clínicas, Universidade Federal do Triângulo Mineiro, Uberaba, MG, Brazil.
Corresponding author:
Vinicius Teixeira De Paula Pignatti
Rua Barão da Ponte Alta, 237, Apto 5007 - Abadia
Uberaba, MG, Brazil Zip Code 38025-250
E-mail: viniciuspignatti@hotmail.com
Article received: April 2, 2016.
Article accepted: February 3, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter