

Original Article - Year 2017 - Volume 32 -
Incisional herniorrhaphy associated to abdominoplasty after gastroplasty
Herniorrafia incisional associada à abdominoplastia pós-gastroplastia
ABSTRACT
INTRODUCTION: Incisional hernias resulting from gastroplasty are a frequent occurrence, requiring planning, surgical technique and patient compliance after surgery for an appropriate outcome.
OBJECTIVE: To demonstrate the treatment of incisional hernias in combination with dermolipectomy (anchor or classic) and pubic lifting, performed in 62 patients undergoing Roux-Y gastroplasty by open surgery and videolaparoscopy.
METHODS: This is a retrospective, cross-sectional study, based on the analysis of 382 patient records. Study plan, strategy, surgical techniques and results will be described.
RESULTS: Success was obtained in all cases, with no incidence of hernia recurrence.
CONCLUSION: The approach was effective, easily reproducible, with low complication rates.
Keywords: Obesity; Abdominoplasty; Gastroplasty; Herniorrhaphy.
RESUMO
INTRODUÇÃO: As hérnias incisionais decorrentes da gastroplastia são uma ocorrência frequente, exigindo planejamento, técnica cirúrgica adequada e colaboração do paciente no pós-operatório, para um adequado resultado.
OBJETIVO: Demonstrar o tratamento das hérnias incisionais em conjunto com as dermolipectomias (âncora e clássica) associadas ao lifting do púbis, realizado em 62 pacientes submetidos à gastroplastia em Y de Roux por via aberta ou por videolaparoscopia.
MÉTODOS: Estudo retrospectivo, transversal, baseado em análise de prontuários de 382 pacientes. Neste artigo será descrito o planejamento, táticas e técnicas cirúrgicas utilizadas e os resultados obtidos.
RESULTADOS: Obteve-se sucesso em todos os casos, sem nenhuma incidência de recidiva da hérnia tardiamente.
CONCLUSÃO: A abordagem adotada mostrou-se eficaz, facilmente reproduzível e com baixos índices de complicações ou intercorrências.
Palavras-chave: Obesidade; Abdominoplastia; Gastroplastia; Herniorrafia.
Obesity is considered the epidemics of the century by the World Health Organization (WHO). In Brazil, a recent survey by IBGE (Brazilian Institute of Geography and Statistic) and the Ministry of Health reveals that 38 million people are overweight (41% of the population) and 10 million are obese.
Thus, bariatric surgery has been established as more efficient and to have better long term results when compared to non-surgical methods for patients with morbid obesity. In this context, about a year after bariatric surgery, patients lose on average 45% of their baseline weight, leading to future excess skin, considerable sagging, and the presence of scars in the abdominal wall and ventral hernias1.
Gastric bypass or gastroplasty were introduced as an alternative treatment for the morbidly obese. A significant weight loss is observed after these procedures, causing excess skin and subcutaneous tissue throughout the body, especially in the abdominal region2. Another complication among bariatric patients is the frequency of abdominal hernias occur in the follow-up, which may be unnoticeable at the physical examination or may present as large herniations3.
The difficulty in dealing with their own image and the changes resulting from severe weight loss leads many patients to seek surgical correction, which is a great new challenge for the plastic surgeon4,5.
The evaluation by an appropriate professional must include a complete patient examination and adequate surgical planning, as well as rigorous pre-op screening, all of them essential for a successful procedure and less complications6.
The assessment should include the investigation of the patient's optimal clinical conditions, presence of anemia, electrolyte and nutritional disorders, presence of weight stability and psychological conditions for the procedure7.
It is known that obesity is a risk factor for incisional hernias, and that the hernia rate after gastric bypass laparotomy is around 4 to 54%8. Thus, the plastic surgeon must consider surgical correction of abdominal hernias as part of the treatment of deformities in these patients9,10.
Treatment of excess skin and subcutaneous tissue in the abdominal region may be achieved through low transverse incisions (classic abdominoplasty), combination of transverse and vertical incisions (anchor-like abdominoplasty) or a less used technique, an incision in the mammary fold (reverse abdominoplasty).
Thus, excess tissue is visible both in the cranio-caudal direction as well as in the latero-lateral view, preventing their compensation in a single horizontal scar, allowing for anchor-like incisions, along with horizontal and vertical incisions, to become widely applied for abdominoplasty in patients with massive weight loss after bariatric surgery. However, these incisions are subject to complications, especially in the confluence region of these scars, the "T" area3.
Currently, abdominoplasty has been adapting to meet the needs of so-called "ex-obese", including in addition to the resection of large skin blocks and treatment of muscle-aponeurotic sagging, the association with other surgeries, such as incisional hernia correction surgery3.
Along with weight loss there is a significant reduction of abdominal content, which is frequently not followed by a return of the herniary content to the cavity. Considering this intense muscle redundancy, abdominal hernias are usually only treated by aponeurotic plication, since the content-continent relationship of these patients is altered, without causing excessive tension to the abdominal wall10.
Therefore, the aim of this paper is to report the experience, as well as complications and changes in quality of life of patients undergoing abdominoplasty associated with the treatment of abdominal hernias after large weight loss in the Morbid Obesity Service, Hospital Regional Hans Dieter Schmidt, Joinville, SC.
OBJECTIVE
The aim of this study was to demonstrate the treatment of incisional hernias resulting from gastroplasty by open surgery and videolaparoscopy (Roux-en-Y bypass) along with dermolipectomy (anchor or classical) combined with pubic lifting report the study's results, complications and conclusions.
METHODS
Retrospective, cross-sectional study, based on the analysis of records of 382 former obese patients undergoing anchor or classic dermolipectomy the Obesity Surgery Service, Hospital Regional Hans Dieter Schmidt. The inclusion criteria was that only records of patients undergoing gastroplasty were analyzed, in a total of 352 patients from 2005 to 2016.
Preoperative preparation
Before undergoing plastic surgery all patients were evaluated and released by the multidisciplinary team (bariatric surgeon, hematologist, endocrinologist, dietician, psychologist and anesthesiologist). Preoperative tests used the following parameters: erythrocytes > 3.5, hemoglobin > 11 hematocrit > 35, tap and normal coagulation, albumin > 3.5, ferritin > 30 Serum iron > 50, vitamin B12 > 350, normal renal function test along with regular cardiologic activity. Refrain from the use of tobacco and total compliance to the treatment of obesity was also demanded.
Surgical Strategy/Technique
With the patient in standing position, markings of skin excess in the abdomen are made using the two-finger pinching maneuver. The extension of the hernia is identified and the limits of the horizontal incision and pubic lifting are marked (Figures 1 A and 1B). Excess skin is resected in block and the hernia is treated after rigorous hemostasis.
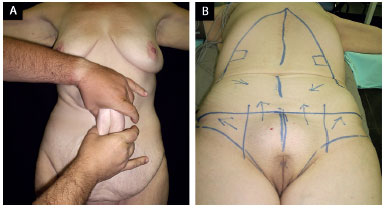
Figure 1. A: Bimanual maneuver; B: Traction vectors.
Part of the hernial sac was used to close the abdominal wall. Only in extreme cases, such as impossibility of a direct approximation the rectus sheaths and muscle, was the use of synthetic mesh required. The fixation of synthetic fabric is made on the posterior sheath of the rectus abdominis, below the muscle (Figures 2A and 2B).
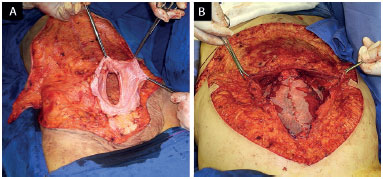
Figure 2. A: Closure using the herniary sac; B: Closure using a synthetic mesh.
After hernia correction, the approximation of the rectus abdominis muscles and plication to the previous aponeurosis is performed. In both cases, "U" shaped stitching was performed with nylon monofilament 2.0. Next, the pubis is lifted, fixing it to the aponeurosis of the rectus muscle, 2 to 3 cm from its original position (Figures 3A and 3B).
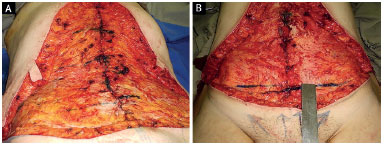
Figure 3. A: Plication of the rectus abdominis; B: Marking of pubic elevation.
Bilateral running suture in both sides, from the detached portion of the flaps to their distal portion is made, thus fixing them to the rectus abdominis muscle sheath (modified Baroudi suture). Vacuum suction drains were placed in layers and sutures were made (Figure 4A and 4B).

Figure 4. A: Modified Baroudi suture; B: Conclusion of abdominal closure.
RESULTS
Sixty-two incisional hernias were found and treated, with varying lengths, among the 352 abdominoplasties performed. In only two cases it was necessary to use synthetic fabric to close the incisional hernia. In both cases they were placed below the rectus abdominis muscles. In all other cases the closure was made through a direct approximation using part of the hernial sac.
We were successful in treating all cases without recurrences to date (Figures 5A-D, 6A-D, 7A-D). There were no major complications such as infection, deep vein thrombosis (DVT) or pulmonary embolism (PE), only complications such as seroma, scar hypertrophy, enlargement of scars and bruising, which are within the global statistics and did not affect the final result.
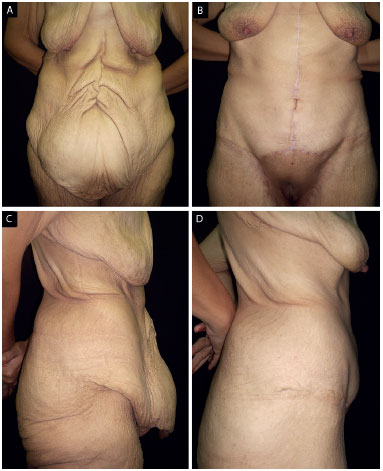
Figure 5. A: Pre-operative AP; B: Postoperative AP; C: Pre-operative - profile; D: Postoperative - profile.
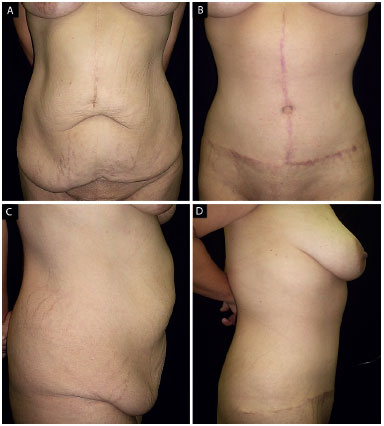
Figure 6. A: Postoperative AP; B: Postoperative AP; C: Pre-operative - Profile; D: Postoperative - Profile.

Figure 7. A: Pre-operative AP; B: Postoperative AP; C: Pre-operative - Profile; D: Postoperative - Profile.
DISCUSSION
Incisional hernias after bariatric surgery, especially when the open approach is used, is observed with a large statistical variation according to the literature data. Hernias were also observed at the incisions made for trocar introduction. Variations in technique or sutures used to close the laparotomy were not conclusive on what is the best approach to be used.
In our series, the presence of incisional hernias is according to worldwide standards. The association of abdominal dermolipectomy and repair of incisional hernias in the same surgical procedure improves patients' quality of life, thus avoiding two surgical procedures, namely: hernia repair and dermolipectomy later on.
Direct closure, with use of the hernial sac is possible in almost all cases. The use of synthetic meshes is mandatory in cases of wide openings of the rectus abdominis muscles or loss of the components of the abdominal wall, rectus abdominis sheath or muscle.
CONCLUSIONS
The treatment of incisional hernias resulting from open gastroplasties requires surgeons to have adequate knowledge, skills and experience for a proper and effective treatment. The way we have treated these patients at our service has proven to be satisfactory, easily reproducible and with good long-term results.
COLLABORATIONS
FSA Analysis and interpretation of the data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
BJ Analysis and/or interpretation of data; completion of surgeries and/or experiments.
MF Analysis and/or interpretation of data; statistical analyses; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
RSSA Statistical analyses; writing the manuscript or critical review of its contents.
FSSA Analysis and/or interpretation of data; statistical analyses; writing the manuscript or critical review of its contents.
REFERENCES
1. Fandiño J, Benchimol AK, Coutinho WF, Appolinário JC. Cirurgia bariátrica: Aspectos clínico-cirúrgicos e psiquiátricos. Rev Bras Psiq Rio Gd Sul. 2004;26(1):47-51. DOI: http://dx.doi.org/10.1590/S0101-81082004000100007
2. Tuma Jr P, Batista BPSN, Milan LS, Faria GEL, Milcheski DA, Ferreira MC. Abdominoplastia vertical para tratamento do excesso de pele abdominal após perdas ponderais maciças. Rev Bras Cir Plást. 2012;27(3):445-9. DOI: http://dx.doi.org/10.1590/S1983-51752012000300020
3. Roxo CDP, Roxo ACW, Labanca L, Martins CRP. Tratamento das hérnias incisionais nas abdominoplastias multifuncionais. Rev Bras Cir Plást. 2008;23(3):184-8.
4. Cavalcanti HA. Abdominoplastia após perda de peso maciça: abordagem, técnicas e complicações. Rev Bras Cir Plást. 2010;25(1):92-9.
5. Van der Beek ES, Te Riele W, Specken TF, Boerma D, van Ramshorst B. The impact of reconstructive procedures following bariatric surgery on patient wellbeing and quality of life. Obes Surg. 2010;20(1): 36-41.
6. Fotopoulos L, Kehagias I, Kalfarentzos F. Dermolipectomies following weight loss after surgery for morbid obesity. Obes Surg. 2000;10(5):451-9. DOI: http://dx.doi.org/10.1381/096089200321593959
7. Burgos L AM, Csendes J A, Papapietro V K. Resection gastric bypass in morbid obese patients aged less than 18 and over 65 years. Rev Med Chil. 2008;136(10):1247-54. PMID: 19194620
8. Speranzini MB, Deutsch CR. Grandes Hérnias Incisionais. ABCD Arq Bras Cir Dig. 2010;23(4):280-6. DOI: http://dx.doi.org/10.1590/S0102-67202010000400015
9. Souza F, Carneiro CP, Luitgasds B, Oliveira ML, Araújo M, Arruda SL. O que pode ser feito para reduzir a incidência de hérnia incisional pós-bypass gástrico em Y de Roux? Brasília Med. 2011;48(3):263-7.
10. Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg. 2004;240(4):578-83. DOI: http://dx.doi.org/10.1097/01.sla.0000141193.08524.e7
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Regional Hans Dieter Schmidt, Joinville, SC, Brazil
3. Hospital da Plástica, Joinville, SC, Brazil
4. Faculdade Evangélica de Medicina do Paraná, Curitiba, PR, Brazil
Institution: Hospital Regional Hans Dieter Schmidt, Joinville, SC, Brazil.
Corresponding author:
Fernando Sanfelice André
Rua Osvaldo Cruz, 128 - Boa Vista
Joinville, SC, Brazil Zip Code 89205-240
E-mail: sanfijlle@gmail.com
Article received: August 3, 2016.
Article accepted: February 3, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter