

Original Article - Year 2017 - Volume 32 -
Study of the relationship between cutaneous elastic fibers and breast ptosis in patients undergoing breast implant surgery
Estudo da relação entre as fibras elásticas cutâneas e a ptose mamária em pacientes submetidas à cirurgia de implante mamário
ABSTRACT
INTRODUCTION: Different techniques and approaches have already been described for the introduction of breast implants. However, these same studies do not take into account the nature of the cutaneous properties and its consequences. The presence of ptosis and degeneration of the elastic fibers can interfere in the contractility, elasticity, resilience of the skin and, consequently, the outcome of implant surgery for breast augmentation.
METHODS: A cross-sectional retrospective study was performed, with evaluation of the medical records of patients undergoing breast augmentation implant procedure from April 2011 to April 2013. Data on the degree of degeneration of the elastic fibers and breast ptosis were collected and a p value of 0.05 was considered for all statistical analyses.
RESULTS: Of the 70 eligible patients, the mean age was 33.2 ± 9.3 years. An absence of degeneration of the elastic fibers was present in 44.2% of the sample. A prevalence of 12.8%, 24.4% and 18.5% was found for level 1 (mild), 2 (moderate) and 3 (severe) ptosis, respectively. The correlation between ptosis and the degeneration of the elastic fibers was r = 0.67, p < 0.001.
CONCLUSIONS: The study of the elements of breast ptosis and cutaneous elastic fibers enabled the evaluation of their varying degrees of presentation. Prospective studies are suggested for a better understanding of the causal relationship between the degeneration of the elastic fibers and breast ptosis.
Keywords: Breast; Elastic fibers; Reconstructive surgical procedures; Breast implant.
RESUMO
INTRODUÇÃO: Diferentes técnicas e abordagens para a introdução de implantes mamários já foram descritas. Entretanto, estes mesmos estudos não levam em conta a natureza das propriedades cutâneas e suas consequências. A presença de ptose e alterações nas fibras elásticas cutâneas pode interferir na contratilidade, elasticidade, resiliência da pele e, consequentemente, no resultado da cirurgia de implantes para aumento mamário.
MÉTODOS: Por meio de um estudo transversal retrospectivo, foram avaliados os registros em prontuário médico de pacientes submetidas ao procedimento de implante de aumento mamário no período entre abril de 2011 a abril de 2013. Dados sobre o grau de falência das fibras elásticas e ptose mamária foram coletados e para todas as análises estatísticas foi considerado um valor de p de 0,05.
RESULTADOS: Das 70 pacientes elegíveis, a média de idade foi 33,2 ± 9,3 anos. A ausência de falência das fibras elásticas cutâneas estava presente em 44,2% da amostra. Para os níveis 1 (discreta), 2 (moderada) e 3 (acentuada), constatou-se as prevalências 12,8%, 24,4% e 18,5%, respectivamente. A ptose e a falência das fibras elásticas apresentaram correlação de r = 0,67 e p < 0,001.
CONCLUSÕES: O estudo dos elementos de ptose mamária e fibras elásticas cutâneas permitiu avaliar os seus variados graus de apresentação. Sugere-se a proposta de estudos prospectivos para o melhor entendimento da relação causal entre falência das fibras elásticas e ptose mamária.
Palavras-chave: Mama; Fibras elásticas; Procedimentos cirúrgicos reconstrutivos; Implante mamário.
The search for surgical interventions for aesthetic purposes, especially the implant of prostheses for breast augmentation, is currently a highly prevalent reality in Brazil1. With the improvement of surgical techniques and breast implants, there has been an improvement in the safety and quality in the use of this type of material and procedures2.
Nevertheless, there are several factors that may influence the postoperative result of breast prosthesis implantation. These factors include breast ptosis and alterations in the skin elastic fibers. Fachinelli et al.3 reported association between abdominal ventral hernia and degeneration of the elastic fibers of the anterior abdominal wall. In the scientific literature, little has been reported on changes in the skin elastic fibers of the breast and the prevalence of this tissue finding has not yet been described.
Breast ptosis is an aesthetic and anatomical disorder characterized by the descent of the breast by relaxation of its support4. This undesired breast alteration is one of the most common motives of patients to look for plastic surgery. The degree of breast ptosis may be directly linked to the degeneration of skin elastic fibers; however, it is not yet known how these two variables relate to each other.
The alterations in cutaneous elastic fibers are presented by degeneration or absence of the fibers and can interfere with the contractility, elasticity, and distensibility of the skin. According to Bonta et al.5, the degeneration of the elastic fibers is related to the aging process, a decrease in the vascularization in the dermis and occurs faster than the degeneration of the collagen fibers. This expression can be present in various parts of the skin throughout the body, which may interfere with the breast support and in its surgical treatments.
Different techniques and approaches have already been described for the introduction of breast implants. In the cases involving alteration of several anatomical features, the chances of finishing touches or reinterventions increase, which leads to unpredictability of the surgical outcome. Various studies6-8 suggest a best technique for each case of breast implants. However, these same studies do not take into account the nature of the cutaneous properties and its consequences.
Mastopexy is the adequacy of the breast content and has been performed frequently with the introduction of breast implants9-11. So far, there is no consensus in this procedure with ptosed breasts. Thus, the combination of techniques and a comprehensive assessment of the characteristics of the patient can optimize the predictability of the procedure.
OBJECTIVE
The objective of this study was to evaluate the relationship between cutaneous elastic fibers and breast ptosis, based on histological findings of surgeries for implantation of breast augmentation prostheses performed from April 2011 to April 2013.
METHODS
This was a cross-sectional retrospective observational study. Medical records of patients undergoing breast augmentation implantation were evaluated. All procedures were performed by the same surgeon at the Mãe de Deus Center Hospital and São Jerônimo Hospital, in Porto Alegre, RS, from April 2011 to April 2013.
Female patients who underwent surgery for implantation of prostheses for breast augmentation, nulliparous, primiparous and multiparous, who had or not breastfed in the post-gestational period, aged between 18 and 60 years, and with biological material (peri-incisional skin fragment biopsy) analyzed for assessment of degeneration or absence of elastic fibers by the Orcein method, were included in the data collection.
Patients whose breast alterations were inherited, patients with breast reconstruction due to cancer, and patients undergoing radiotherapy and/or chemotherapy were excluded from the data collection. This study was approved by the Research Ethics Committee (CEP) of the Mãe de Deus Hospital, under protocol number 1.144.567 of the Brazil Platform.
Data Collection
The data analyzed from the medical records of the patients were: age on the day of surgery, number of pregnancies, breastfeeding or not in the post-pregnancy period, degree of ptosis, and degree of absence or degeneration of elastic fibers. The age on the day of surgery was defined by the calculation between the date of birth and date of surgery.
The number of pregnancies was evaluated by health history and the number of pregnancies the patient already had was annotated. The data were classified as nulliparous, primiparous and multiparous. Breastfeeding (whether the patient breastfed or not in the post-pregnancy period) was also recorded.
Data on breast ptosis were collected from the evaluation described in the medical charts in the period prior to surgery. Ptosis was defined in this study according to the criteria established by Daniel12, which takes into account the location of the nipple, the lower mammary pole and the inframammary crease (Figure 1).
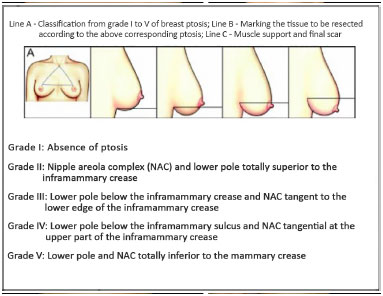
Figure 1. Representation of the visual classification of breast ptosis. Design extracted and adapted from figure 1 of the work proposed by Daniel12.
The degree of elastic fiber degeneration was collected from patients' medical records. The Orcein Goldner's trochrome method allows the evaluation of the degree of degeneration in 4 levels (0: absence of degeneration, 1: mild, 2: moderate, 3: severe).
Statistical Analysis
The sample included a review of medical charts of patients undergoing surgical procedure for breast implantation from April 2011 to April 2013, and who had biological material rated for the degree of degeneration of elastic fibers. The prevalences were described in the form of prevalence and continuous variables were described by means and standard deviations.
The differences between the groups with and without ptosis and degeneration of elastic fibers were evaluated by the Student's t-test or Mann-Whitney test for continuous variables and the chi-squared test or Fisher's exact test for categorical variables. The correlation was analyzed by the Spearman Correlation Coefficient (rs). An alpha level of 0.05 was considered for all statistical analyses, and the Statistical Package for Social Sciences (SPSS), version 19, was used for the evaluation of variables.
RESULTS
From April 2011 to April 2013, 92 patients underwent implantation of breast prostheses. Of these patients, 70 had material analyzed for the degeneration of elastic fibers. The description of the characteristics of the sample is shown in Table 1. Of the patients who had children, all breastfed and the breastfeeding period ranged from 1 to 48 months. Table 2 shows the association between ptosis and degeneration of the elastic fibers. Figure 2 shows the correlation between ptosis and degeneration of the elastic fibers.
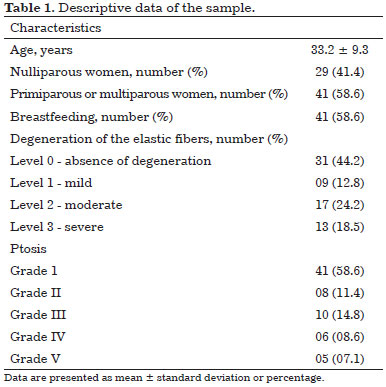
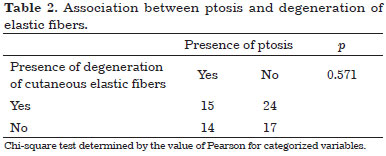
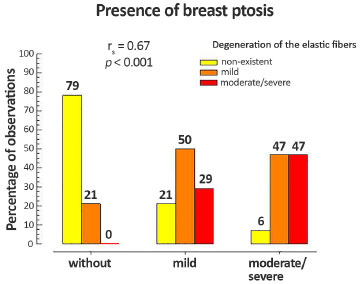
Figure 2. Correlation between ptosis and degeneration of elastic fibers.
The average period of follow-up reported in medical records was from 6 to 12 months. During this period, the following changes were recorded: six cases of reintervention with exchange of implant. The reasons involved were: spin of prosthesis (one case), early capsular contracture (one case), early postoperative ptosis (two cases), Paget's disease (neoplasia in situ, one case) and hypertrophic and flaccid scar (one case). In another eight cases, outpatient healing readjustments were carried out.
Figures 3, 4, 5 and 6 present the frontal and right profiles of the following cases, before and after surgery: Without ptosis and without degeneration of the elastic fibers; with ptosis and without degeneration of the elastic fibers; without ptosis and with degeneration of the elastic fibers; and with ptosis and with degeneration of the elastic fibers, respectively.
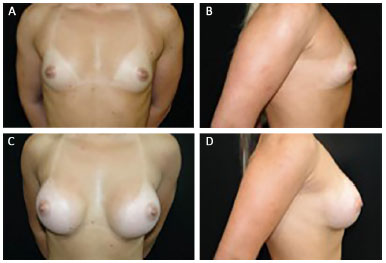
Figure 3. Front profile. A: Right profile; B: Preoperative, frontal profile; C: Right profile; D: Post-operative presentation without ptosis and without degeneration of elastic fibers.
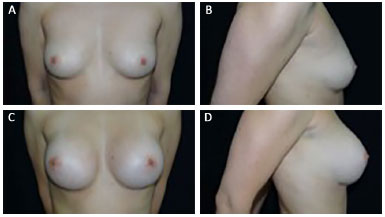
Figure 4. Front profile. A: Right profile; B: Preoperative, frontal profile; C: Right profile; D: Post-operative presentation without ptosis and with degeneration of elastic fibers.
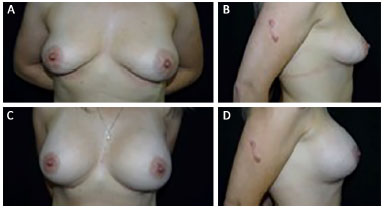
Figure 5. Front profile. A: Right profile; B: Preoperative, frontal profile; C: Right profile; D: Post-operative presentation without ptosis and with degeneration of the elastic fibers.
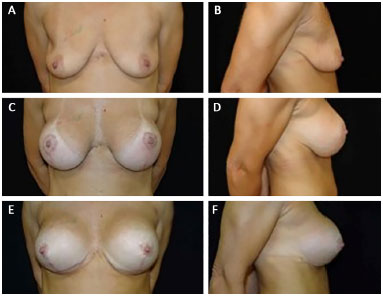
Figure 6. Frontal profile. A: Right profile; B: Preoperative, frontal profile; C: Post-operative 300 cc retro-glandular, frontal profile; D: Post-operative 300 cc retro-glandular, right profile; E: Post-operative aspect 6 months after exchange of implant with mastopexy by 350 cc retro-muscular, frontal profile; F: Postoperative aspect 6 months after exchange of implant with mastopexy by 350 cc retro-muscular, right profile.
DISCUSSION
The study of the relationship between changes in cutaneous breast elastic fibers and breast implant surgery is another attempt to establish the factors that are important in the surgical outcome. The accentuated changes, both in cutaneous elastic fibers and the degree of breast ptosis, showed that these variables interfere silently and significantly in the process and in the surgical outcome.
Thus, the understanding of the mechanisms involved is based on the attempt to elucidate the vulnerable and unpredictable outcomes, revealing the need of knowledge of these factors for a better management of cases.
Breast ptosis is one of the most studied, more frequent and more persistent breast alterations. When it presents in moderate and accentuated degrees, it leads the surgeon to seek combined treatments, associating a mastopexy to the breast implant surgery, to correct the outline excess of the mammary pocket13.
This combination of surgical tactics and techniques can change the desired outcome, interfering in the result, thus needing a second intervention in the short and medium term8. According to Bono14, it is important to correct the ligament structures (Giraldés and Cooper ligament), these being responsible for the fixation, support and immobilization of the whole breast15.
Persistent postoperative breast ptosis, both in mastopexy, introduction of breast implants or both associated techniques, remains one of the most important and frequent complaints in the outcomes15, which highlights the need for a continuous study in search of the most appropriate treatment for each case.
The degeneration of the cutaneous elastic fibers appears as a silent factor, leading to the unpredictability of their properties such as elasticity, distensibility, and resilience. Based on the work of Fachinelli et al.3, it was possible to verify that the degeneration of the elastic fibers could have influence on the surgical outcome of breast implants.
Although Fachinelli et al.3 did not find differences in density and distribution of elastic fibers in patients with inguinal hernia, in this study these properties are altered. In a study by Bonta et al.5, the alterations of elastic fibers, skin thinning, histological alterations of collagen and the vascularization of the skin were related to natural aging.
Within the results found in relation to the elastic fibers, we can raise the hypothesis that the various degrees of degeneration of the elastic fibers found in the sample created a chain of postoperative responses in which edema, skin tension, and traction can evolve in an altered physiological way, leading to the consequent alteration of the outcome.
Both the alterations in cutaneous elastic fibers and the degree of breast ptosis, when severe and correlated, point to the indication of a second surgical intervention, which must be properly explained and analyzed by the surgeon and the patient. In this study, these changes could only be understood by evaluating the laboratory results after the surgery; thus, if this information could be classified in the preoperative tests as a relevant factor, possibly, attempts to circumvent and effectively resolve these breast alterations would be more predictable, leading to the optimization of results.
Some limitations can be observed in this study. As it is a retrospective experimental, observational study, one cannot establish a causal link between the variables studied. This limitation is inherent to the type of design chosen for this initial evaluation of the variables of interest.
Moreover, there are several classifications of breast ptosis. For this work, the classification proposed by Daniel12 was chosen because it was considered the most didactic. However, there are still other classifications widely used, such as, for example, the proposal of Regnault16.
The setting for the use of the classification of ptosis by the criteria of Daniel12 had as references the same anatomic units for all degrees (nipple areola complex - NAC - and inframammary crease). In contrast, the criteria of Regnault16 vary depending on the height of the areola, the contour of the gland and skin hypoplasia (complete or true ptosis, divided into grades I - III; partial ptosis and pseudoptosis).
CONCLUSIONS
The study of the elements of breast ptosis and cutaneous elastic fibers enabled the evaluation of their varied degrees of presentation and influence in the surgical result. Due to the pre-operative unpredictability, this study suggests a better analysis of the degrees of alteration of the cutaneous elastic fibers through the proposition of a prospective study with the objective of contributing in a unique way to the best analysis of criteria and indication of suitable surgical techniques for breasts.
COLLABORATIONS
JEBM Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
REFERENCES
1. Sociedade de Cirurgia Plástica. De acordo com a ISAPS Brasil lidera ranking de cirurgia plástica no mundo. [acesso 2015 Maio 25]. Disponível em: http://www2.cirurgiaplastica.org.br/de-acordo-com-a-isaps-brasil-lidera-ranking-de-cirurgias-plasticas-no-mundo/
2. Pitanguy I, Amorim NFG, Ferreira AV, Berger R. Análise das trocas de implantes mamários nos últimos cinco anos na Clínica Ivo Pitanguy. Rev Bras Cir Plást. 2010;25(4):668-74. DOI: http://dx.doi.org/10.1590/S1983-51752010000400019
3. Fachinelli A, Trindade MR, Fachinelli FA. Elastic fibers in the anterior abdominal wall. Hernia. 2011;15(4):409-15. DOI: http://dx.doi.org/10.1007/s10029-011-0804-2
4. Souza SC. Graduações de ptose mamária. Arq Catarin Med. 2008;37(3):66-71.
5. Bonta M, Daina L, Muţiu G. The process of ageing reflected by histological changes in the skin. Rom J Morphol Embryol. 2013;54(3 Suppl):797-804.
6. Hendricks H. Complete submuscular breast augmentation: 650 cases managed using an alternative surgical technique. Aesthetic Plast Surg. 2007;31(2):147-53. DOI: http://dx.doi.org/10.1007/s00266-006-0128-2
7. Graf RM, Bernardes A, Rippel R, Araujo LR, Damasio RC, Auersvald A. Subfascial breast implant: a new procedure. Plast Reconstr Surg. 2003;111(2):904-8. PMID: 12560720 DOI: http://dx.doi.org/10.1097/01.PRS.0000041601.59651.15
8. Daher JC, Amaral JDLG, Pedroso DB, Cintra Júnior R, Borgatto MS. Mastopexia associada a implante de silicone submuscular ou subglandular: sistematização das escolhas e dificuldades. Rev Bras Cir Plást. 2012;27(2):294-300. DOI: http://dx.doi.org/10.1590/S1983-51752012000200021
9. Spear S. Augmentation/Mastopexy: "Surgeon, Beware". Plast Reconstr Surg. 2003;112(3):905-6. PMID: 12960875 DOI: http://dx.doi.org/10.1097/01.PRS.0000072257.66189.3E
10. Spear SL, Carter ME, Ganz JC. The correction of capsular contracture by conversion to "dual-plane" positioning: technique and outcomes. Plast Reconstr Surg. 2003;112(2):456-66. PMID: 12900603 DOI: http://dx.doi.org/10.1097/01.PRS.0000070987.15303.1A
11. Spear SL, Pelletiere CV, Menon N. One-stage augmentation combined with mastopexy: aesthetic results and patient satisfaction. Aesthetic Plast Surg. 2004;28(5):259-67. DOI: http://dx.doi.org/10.1007/s00266-004-0032-6
12. Daniel MJB. Inclusão de prótese de mama em duplo espaço. Rev Bras Cir Plást. 2005;20(2):82-7.
13. Sanchéz J, Carvalho AC, Erazo P. Mastopexia com prótese: técnica em "D" espelhado. Rev Bras Cir Plást. 2008;23(3):200-6.
14. Bono JEP. Mamoplastia ligamentar. Rev Bras Cir Plást. 2008;23(3):192-9.
15. Gomes RS. Mastopexia com retalho de pedículo superior e implante de silicone. Rev Bras Cir Plást. 2008;23(4):241-7.
16. Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976;3(2):193-203.
Hospital Mãe de Deus Center, Porto Alegre, RS, Brazil
Institution: Hospital Mãe de Deus Center, Porto Alegre, RS, Brazil.
Corresponding author:
Javier Enrique Brod Méndez
Rua São Francisco da Califórnia, 133 - Higienópolis
Porto Alegre, RS, Brazil Zip Code 90550-080
E-mail: jmendez0603@hotmail.com
Article received: July 29, 2015.
Article accepted: November 11, 2015.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter