

Original Article - Year 2017 - Volume 32 -
Primary treatment of lip and nasal deformity in unilateral cleft lip or cleft lip and palate
Tratamento primário da deformidade labial e nasal nas fissuras labiais e labiopalatinas unilaterais
ABSTRACT
INTRODUCTION: Cleft lip and palate, the most frequent congenital craniofacial deformity, mainly affects the upper lip, nose, and palate. One possible treatment is single-stage lip repair with primary rhinoplasty. Here we assessed the correlations among cleft severity, surgical age, and aesthetic results.
METHODS: A total of 26 patients with unilateral cleft lip or cleft lip and palate aged 3-12 months underwent surgical lip repair associated with the Göteborg/McComb rhinoplasty technique. Steps before and after surgery were separately evaluated by five plastic surgeons using pictures and the data were analyzed.
RESULTS: The average patient age at surgery was 6.5 ± 3.15 months, and only seven patients (26.9%) underwent surgery at 3 months of age as recommended by the protocol. Cleft severity and results quality were associated, whereas surgical age and aesthetic results were not correlated. Results in all cases were considered optimal or satisfactory.
CONCLUSIONS: The lip repair technique, which presents good reproducibility and aesthetic results and can be used with other primary treatment techniques for the nose, should be adopted by treatment centers managing cleft lip and palate. Cleft severity is an important factor in results quality; the greater the severity, the worse the results. In the present study, surgical age was not correlated with results quality.
Keywords: Cleft lip; Lip/surgery; Mouth abnormalities; Nose/abnormalities; Nose/surgery.
RESUMO
INTRODUÇÃO: A fissura labiopalatina é a deformidade congênita mais frequente dentre as malformações craniofaciais, afetando principalmente o lábio superior, nariz e palato. A realização da queiloplastia associada à rinoplastia primária em tempo único é uma tendência. Avaliamos a correlação entre a gravidade da fissura, a idade cirúrgica e a qualidade estética do resultado pós-operatório.
MÉTODOS: Foram avaliados 26 pacientes com fissuras labiais ou labiopalatinas unilaterais, com idades entre 3 e 12 meses, operados pela técnica de queilorrinoplastia de Göteborg/McComb. Foi feita uma avaliação fotográfica do pré e pós-operatório por cinco cirurgiões plásticos separadamente e os dados analisados.
RESULTADOS: A idade média de realização do procedimento foi de 6,5 ± 3,15 meses, sendo que somente sete pacientes (26,9%) foram operados na idade de 3 meses preconizada pelo protocolo. Foi encontrada correlação entre a gravidade da fissura e a qualidade dos resultados, ao mesmo tempo em que não foi encontrada associação entre a idade da cirurgia e os resultados. Todos os casos do estudo foram considerados ótimos ou satisfatórios.
CONCLUSÕES: A utilização de uma técnica de queiloplastia que seja de fácil reprodutibilidade, com bons resultados estéticos, e que possa ser utilizada em conjunto com outras técnicas de tratamento primário do nariz é uma boa opção a ser adotada por centros de tratamentos deste tipo de paciente. A gravidade da fissura é um fator importante na qualidade dos resultados. Quanto mais grave a fissura os resultados tendem ser piores. A idade da cirurgia, neste estudo, não teve correlação com a qualidade nos resultados.
Palavras-chave: Fenda labial; Lábio/cirurgia; Anormalidades da boca; Nariz/anormalidades; Nariz/cirurgia.
Cleft lip and palate, the most frequent congenital craniofacial deformity with extremely varied presentations, mainly affects the upper lip, nose, and palate. Accordingly, adequate full treatment is required, and multidisciplinary teams comprising plastic surgeons, dentists, and speech therapists, among other professionals, are currently recommended1.
In Brazil, few studies have assessed the incidence of this malformation in the general population. In such studies, the incidence was reportedly 0.88:1000 live births2 to 1:1000 live births3,4.
In Rio Grande do Norte, the Professor Heriberto Bezerra Pediatric Hospital (HOSPED), which belongs to the Universidade Federal do Rio Grande do Norte (UFRN), ran a craniofacial abnormalities program until 2013 and was a State reference for treating patients with cleft lip and palate.
The program was based on a group of three types of professionals required for cleft treatment: plastic surgeons, speech therapists, and orthodontists (focusing on maxillary functional orthopedics) in addition to using the UFRN and other professionals supporting therapy (social workers, nurses, pediatricians, otolaryngologists, neuropediatric specialists, geneticists, and others).
In the treatment of patients with cleft lip and palate, multidisciplinary efforts are required and surgical techniques and tactics are increasingly sought to obtain better aesthetic and functional results considering that each case presents distinct anatomical alterations with individualized requirements5. HOSPED used the Göteborg6 technique described by Buzzo in 2010 as a protocol for lip correction. This technique was developed via a scientific and cultural agreement between the University of Gothenburg, Sweden, and the Brazilian Society of Research and Assistance to Craniofacial Rehabilitation (SOBRAPAR), Campinas, São Paulo, in 1995 and coordinated by Dr. Cássio M. Raposo do Amaral, Dr. Bengt Johanson, and Dr. Jan Ljla6,7.
To briefly summarize the development of lip repair treatments throughout history, it should be mentioned that the first attempts to fix cleft lips were reported in 390 B.C. in China8. Then, in the 16th century, in 1564, Ambroise Paré described a technique using needles to approach the sides of cleft lips in a straight line with subsequent anchoring of the sides with threads around the needles in a figure-eight shape9.
Mirault (1844) and Giraldes (1866) described a lip repair technique based on triangular flaps. In 1892, Hagedorn was already concerned with re-constructing the Cupid bow. William Rose (1891) and James Thompson (1912) described techniques with angulated scars that generated an elongated lip and decreased the formation of red patches, which was common at that time9.
Since then, there has been concern about the use of angulated or straight scars to minimize scar retraction, which is common in the latter. In 1949, Le Mesurier described a technique using square flaps based on a technique by Hagedorn10. In 1954, Charles Tennison emphasized the importance of repositioning the orbicularis muscle of the mouth, maintaining the Cupid bow, and using triangular flaps11. This technique was modified by Randall in 1959 to improve flap position12,13. In 1968, Spina recommended z-plasty of flaps on the medial side of the lip; at the same time, Perseu Lemos recommended a similar technique as demonstrated by Anger in 200514.
Ralph Millard Jr became the most important figure in lip repair after publishing his technique in 19579, which is now probably the most used technique, and he and other authors such as Mohler15 have modified it.
Nasal deformity, which is one of the greatest challenges for surgeons performing this surgery time, also requires consideration. The positions of the nasal wings and "soft triangle" as well as symmetry are difficult to achieve satisfactorily.
According to Harold McComb (1985 & 1986) and Keneth Salyer (1986), primary rhinoplasty performed in the same stage of surgery as lip repair, did not result in alterations of nasal cartilage growth and development9,16,17, which encourages the majority of surgeons today to perform the primary surgery involving the lip and nose in a single stage.
OBJECTIVE
We aimed to correlate cleft severity, patient age at time of surgery, and aesthetic results employing the same surgeon and surgical technique in each procedure.
METHODS
A total of 26 patients aged 3-12 months were included in this retrospective study conducted from July 2008 to October 2013. Among them, 17 were male and nine were female, and all underwent lip repair using the Göteborg technique and McComb rhinoplasty. The surgical procedures were performed by the same surgeon in the HOSPED/UFRN, under inhalation general anesthesia, orotracheal intubation, spontaneous breathing, and adequate monitoring.
This research project followed the legal guidelines described in Resolution 196/96 from the National Health Council regarding research involving humans and according to the principles of the Declaration of Helsinki.
All patients without adequate photographic documentation, with an associated syndrome, with a rare cleft condition, who underwent surgery after 1 year of age, or who underwent a lip repair treatment other than the Göteborg technique were excluded from this study.
The protocol used specifies that the ideal age to perform primary lip repair is 3 months and follows the "10 rule" (10 weeks of life - approximately 3 months; 10 mg/dL of hemoglobin; 10 pounds of weight - approximately 4.5 kg).
After anesthetic induction, the patient was positioned in the horizontal dorsal decubitus position with slight cervical hyperextension using a small cushion in the shoulders and cloth in the occipital region to stabilize the head. A marking was then performed as recommended by the Göteborg technique and described by Buzzo in 2010 using methylene blue for both complete and incomplete clefts (Figures 1 and 2). Tattooing the key points was a challenging maneuver using an insulin needle and methylene blue since during surgery, due to tissue manipulation, markings are otherwise frequently lost.

Figure 1. Incomplete cleft lip and palate - Göteborg marking.
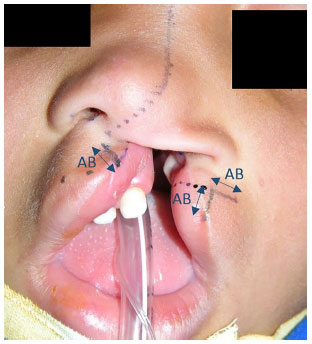
Figure 2. Complete cleft lip and palate with detail of Göteborg marking using the AB measure.
After the marking was made, blocking of the infraorbital branches of the trigeminal nerve was performed with 2% xylocaine solution using a vasoconstrictor at a concentration of 1:200,000 (maximum dose, 5 mg/kg) and 7.5 mg/dL ropivacaine (maximum dose, 3 mg/kg) with minimum infiltration in the upper lip and nose to avoid anatomical distortion that could have affected the surgeon evaluation.
The surgery was initiated by preparing the lip on the cleft side, incising the skin with a cold steel scalpel no. 11 in total plane, making angulated skin flaps, and following the incision in the portion of the labial gingival sulcus nearly 2 mm above the sulcus to facilitate closure. This incision can be extended as much as required so the lateral flap reaches the medial non-cleft portion.
Following this moment, a dissection of the cleft portion of the lip was performed with the aid of a Freer or Aesculap elevator, moving it from the maxilla to the matching piriform fossa and fully releasing the base of the nasal wing. The orbicularis muscle of the mouth was isolated by releasing only the amount required to suturing this contralateral muscle. Care should be taken to never excessively release this muscle on the cleft portion in particular; otherwise, a visible recess may be created as a result in the lip after closure (Figure 3).

Figure 3. Prepared lip flap of the cleft side.
After this step, the non-cleft portion was worked upon, incising again the skin in total plan using a cold steel scalpel no. 11, making skin flaps, and releasing the labial gingival sulcus, including the labial frenulum (maneuver that allows a good movement on the non-cleft lip side when connecting it to the cleft portion), and isolating the orbicularis muscle of the mouth in this side to elevate it approximately 2-3 mm.
From this point, we initiated the alar cartilage elevation on the cleft side in both the vestibular and external portions using an iris scissors. This subcutaneous elevation was widely extended through the nasal dorsum on the cleft side according to the guidelines by McComb (Figure 4).
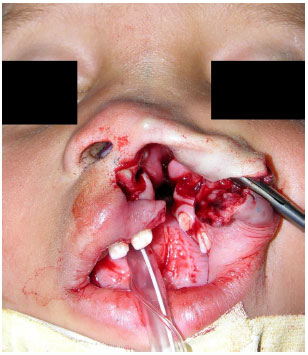
Figure 4. Nasal dissection details.
The labial mucosa on the cleft side was then closed using PDS or Vicryl 4-0 sutures to carry the medial lip until the last point of this side, and this point was fixed in the maxilla on the non-cleft portion. The medial flap suture was finished, correcting the labial frenulum and following the sulcus to the lateral flap, which was already fixed in the maxilla.
Synthesis of the orbicularis muscle of the mouth was then performed using non-absorbable thread (nylon 4-0) with three to five stitches depending on muscular volume. The skin flaps were finally rotated, advanced, and sutured with nylon 6-0 thread. The excess red mucosa was dissected extremely carefully in the alignment of the transition between the skin and lip mucosa, and the redness was sutured with PDS or Vicryl 4-0 sutures.
According to the protocol used here, the McComb technique was performed for the primary rhinoplasty, suturing from the point that joins the domal region of the alar cartilage in the cleft side until a point above the ipsilateral triangular cartilage, and this point was sutured with a 40/12 needle and fixed outside the skin using a bolster to protect the skin made from sterile nasogastric or serum tube. Following the same principle, the sutures surrounding the nasal wing on the cleft side were added and used three to five stiches depending on each case.
Patients remained hospitalized for a mean 24 h. The sutures performed with bolster and 6-0 nylon on the skin were removed in the first return at 7 days after surgery. Feeding comprised mashed or liquid-form foods for 1 week until the first return, progressing to light and unrestricted until the end of the first month after surgery. Pacifiers and feeding bottles were avoided until 2 weeks after surgery. The returns occurred at 7, 14, and 30 days and 3-6 months after surgery. Speech therapy was released after 15 days and orthodontics 30 days after surgery.
The analysis of the results was performed according to photographic documentation in the frontal and basal position. The pictures were evaluated separately by five plastic surgeons. Two moments were evaluated: one before surgery, to classify the clefts as mild, moderate, or severe; and one after surgery to assess the aesthetic appearance of the surgical results and classify it as poor, satisfactory, or optimal.
In the post-operative aspect, the surgeons were asked to observe lip scar quality and position, leveling degree of the skin-mucosa line, and symmetry between the nostrils and columella position.
Statistical analysis
The quantitative data are described as mean and standard deviation, while categorical data are shown as counts and percentages.
To assess the association between quantitative variables among themselves (cleft severity score before surgery, aesthetic results, and surgical age), the Pearson correlation coefficient was used and significance was determined using Student's t-test.
To compare means between aesthetic results and preoperative cleft severity categories, analysis of variance was used followed by Tukey's post-hoc test.
The significance used in the study was alpha = 0.05.
The data were analyzed using SPSS version 22.0.
RESULTS
Among the 26 patients included in the study, 17 were male (65.4%) and nine were female (34.6%); 11 (42.3%) presented with cleft lip and 15 (57.7%) had cleft lip and palate; 19 (73.1%) occurred on the left side and seven (26.9%) occurred on the right side.
The average patient age at the time of surgery was 6.5 ± 3.15 months; only seven patients (26.9%) underwent surgery at the recommended 3 months of age.
For the statistical analysis, two questions were addressed: Was there any correlation between preoperative cleft severity and aesthetic results; and was there a correlation between surgical age and aesthetical results.
Comparison of the two groups revealed a correlation between cleft severity and results quality, and the greater the cleft severity, the worse the results (p = 0.025).
Regarding the cleft severity categories (mild, moderate, and severe), a statistically significant correlation was observed between mild and severe only. Between these two groups, there was a tendency to obtain worse results for severe clefts and better results for mild clefts (p = 0.005 and r = 0.53) (Figure 5).
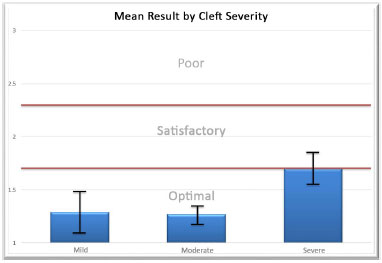
Figure 5. Mean result is optimal/satisfactory regardless of cleft severity (p = 0.005 and r = 0.53).
Regarding our second question, the correlation between surgical age and aesthetic results, the analysis demonstrated no statistically significant association. We then assessed the correlation between surgical age and cleft severity to discard the possibility of a "contamination" from surgical age group due to a specific concentration of severity level since all cases in our service arrived via self-referral (e.g., all patients of a certain age showing the same severity level). There was no statistical significant correlation observed, which corroborated with the first test performed. Thus, we concluded that there was no statistically significant correlation between surgical age and aesthetic results.
The mean result in terms of severity category grade was good, with mean mild and moderate category scores within the optimal level and mean severe category score at the optimal/satisfactory border.
There was only one recorded complication, representing a complication index of 3.8%. The patient presented with a moderate-grade facial hematoma for which conservative treatment was provided that resulted in good progression.
DISCUSSION
Cleft severity and age at primary surgery contributed extensively to the aesthetic results. As demonstrated by Buzzo6,7 and Raposo-do-Amaral18, the probability of treating cleft patients with surgery at the right age and with a good nutritional condition is low because our service is performed via public assistance through the national health system, in which the absolute majority of patients have low socioeconomic status.
Lack of information about the disease, delays in being directed to the reference center, difficulty traveling to the treatment center (sometimes comprising long inter-municipal dislocations), low local socioeconomic status, nutritional deficiencies, and anemia are the main reasons for treatment delays in most patients19.
This issue remains very challenging since it involves several socioeconomic, cultural, and ethnic variables in addition to diverse cleft-related factors. Thus, the search for the best treatment that best suits each situation and achieves the best aesthetic and functional results must persist.
In fact, during the study period (July 2008 to October 2013), 66 patients underwent unilateral lip repair with rhinoplasty following the Göteborg/McComb technique; unfortunately, most cases were not included in this study since they did not meet the technique's surgical age criterion of 3 months.
Considering the high number of patients who underwent surgery at an older age, it will be interesting to conduct another study that compares the results obtained in patients treated at 3 months according to the protocol and those in patients treated at older ages. Such a study would enable the analysis of the real damage or sequelae that may occur in lip repair/primary rhinoplasty conducted at an older age.
Only 26.9% of patients in this study could be treated at the age recommended by the protocol; the remaining were unable mainly due to anemia caused by malnutrition and a poor diet. It should be considered that this service is offered in the poor state of Rio Grande do Norte, where the socioeconomic status of most of the population is very low6,7,18,19. According to the protocol, the patient must have a hemoglobin level ≥ 10 mg/dL to undergo the procedure; otherwise, the surgery must be postponed until this measure is achieved.
Another important constraint was the lack of transport accessible to these patients for treatment compliance since speech therapy and orthodontic services were provided weekly and required their attendance.
Similar to what was described in the literature20,21, 57.7% of our cases involved cleft lip and palate and 73.1% were located on the left side20,21.
The Göteborg technique used in this study was easily performed and presented good reproducibility (did not present variable distances or angulations). The markings were made using standard measures, the distance between the most prominent portion of the non-cleft side (A) to the projection of the philtral crest in the skin-mucosa line (B) (Figure 2).
Using this measure (AB), we performed the remaining markings on both labial sides. Among the positive aspects of this technique, we emphasize that the redness was of adequate size, the philtral crest of the cleft side was a good length (due to the flaps that simulate z-plasty), and the orbicularis muscle of the mouth was anatomically repositioned, and the labial gingival sulcus was of a good depth.
Brown and McDowell, Millard (1982), Salyer (1986), Bardach (1987), and McComb (1984) demonstrated that there were no restrictions to nasal growth after single-stage lip and nasal surgery, which suggests that the primary surgery should involve the lip and nose20,22.
The nose is one of the greatest stigma of cleft patients (and a surgical challenge), mainly due to the collapse of the nasal wing on the cleft side; in addition, deviations and asymmetries vary from case to case. By approaching the lip and nose jointly in the primary surgery, many of these alterations are reduced and future interventions on the cleft nose are minimized, resulting in a more peaceful childhood with less stigma and prejudice.
The McComb technique may be perfectly adapted to the Göteborg approach, which generates a good presentation of structures for a wide nasal elevation as recommended. It also increases the total surgery time by 15 minutes (elevation at the end of elaborating lip flaps and points where the bolster was applied at the end of the surgery with the lip already sutured). These two techniques are synergetic and required to obtain a good result (Figures 6 and 9).

Figure 6. Case 1 - Left cleft lip.

Figure 7. Case 2 - Left cleft lip.

Figure 8. Case 3 - Left cleft lip and palate.

Figure 9. Case 4 - Right cleft lip and palate.
The analysis revealed a correlation between cleft severity and aesthetic results; specifically, the greater the severity, the worse the result.
Despite the tendency to obtain a worse result in cases of severe cleft, optimal and satisfactory aesthetic results were obtained in all cases and there were no cases of a poor result (Figure 10 and Figure 5).
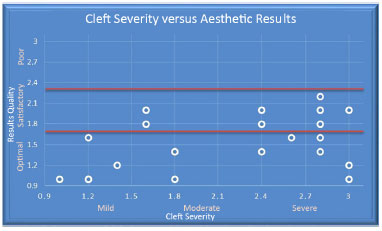
Figure 10. Increasing cleft severity tends to worsen the results (p = 0.025).
We found no correlation between surgical age and aesthetic results (Figure 11), which we did not expect to observe. On the other hand, it was reassuring to observe good results regardless of surgical age since a delay in surgical age is frequently seen in Northeastern Brazil due to the above mentioned issues. These results may because the cohort was small due to the maximum allowable surgical age of 1 year, which decreased greatly the number of cases included; and the follow-up of patients not being extensive, as the pictures analyzed were collected from 6 months to 2 years after surgery.
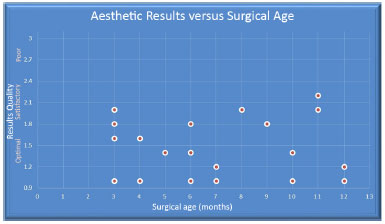
Figure 11. Surgical age was not correlated with aesthetic results (p > 0.05).
CONCLUSIONS
In the treatment of patients with unilateral cleft lip and cleft lip and palate, the use of a lip repair technique with good reproducibility and aesthetic results that can be used together with other techniques in the primary treatment of the nose is undoubtedly a good option for treatment centers.
The aesthetic results of all cases in this study were classified as optimal or satisfactory.
Cleft severity is an important factor contributing to aesthetic results; the greater the severity, the worse the results.
Surgical age in this study was not correlated with aesthetic results.
COLLABORATIONS
LSBS Data analysis and/or interpretation; final manuscript approval; study planning and design; surgery and/or experiments; manuscript elaboration and critical content review.
CLB Final manuscript approval; study design and elaboration.
REFERENCES
1. Franco D, Eyler AD. Cirurgia de fissurados: detalhes que facilitam. Rev Bras Cir Plást. 2003;18(1):55-69.
2. Cândido TT. Epidemiologia das fendas de lábio e/ou palato: estudo de recém-nascidos em dois hospitais de Porto Alegre, no período de 1970 a 1974 [Tese de doutorado]. Porto Alegre: Universidade Federal do Rio Grande do Sul; 1978.
3. Nagem Filho H, Moraes N, Rocha RGF. Contribuição para o estudo da prevalência das más formações congênitas lábio-palatais na população escolar de Bauru. Rev Fac Odontol. (São Paulo). 1968;6(2):111-28.
4. Souza JMP, Buchalla CM, Laurenti R. Estudo da morbidade e da mortalidade perinatal em maternidades. III - Anomalias congênitas em nascidos vivos. Rev Saúde Pública. 1987;21(1):5-12. DOI: http://dx.doi.org/10.1590/S0034-89101987000100002
5. Anger J, Sertorio CB. Avaliação das medidas do alongamento do lábio nas queiloplastias com plástica em Z no tratamento das fissuras labiopalatinas unilaterais. Rev Bras Cir Plást. 2006;21(3):133-9.
6. Buzzo CL. Tratamento cirúrgico da fissura labial pela técnica de Göteborg: seguimento de 7 anos. Rev Bras Cir Plást. 2010;25(2):251-9.
7. Buzzo CL, Franco D, Nóbrega ESS, Silva-Freitas R, Amaral CAAR, Carone DR. Avaliação do uso do modelador nasal em pacientes portadores de fissura labial unilateral operados pela técnica de Göteborg. Rev Bras Cir Plást. 2010;25(4):541-7.
8. Boo-Chai K. An ancient Chinese text on a cleft lip. Plast Reconstr Surg. 1966;38(2):89-91. PMID: 5330449 DOI: http://dx.doi.org/10.1097/00006534-196608000-00001
9. Millard DR. Cleft Craft. The evolution of its surgery. Vol. I. The unilateral deformity. Philadelphia: Lippincott Williams & Wilkins; 1976.
10. LeMesurier AB. A method of cutting and suturing lip in the treatment of complete unilateral clefts. Plast Reconstr Surg (1946). 1949;4(1):1-12.
11. Tennison CW. The repair of the unilateral cleft lip by the stencil method. Plast Reconstr Surg. 1952;9(2):115-20. DOI: http://dx.doi.org/10.1097/00006534-195202000-00005
12. Randall P. A triangular flap operation for the primary repair of unilateral clefts of the lip. Plast Reconstr Surg. 1959;23(4):331-47. DOI: http://dx.doi.org/10.1097/00006534-195904000-00003
13. Saunders DE, Malek A, Karandy E. Growth of the cleft lip following a triangular flap repair. Plast Reconstr Surg. 1986;77(2):227-38. PMID: 3945686 DOI: http://dx.doi.org/10.1097/00006534-198602000-00009
14. Anger J. Prof. Perseu Castro de Lemos e Prof. Victor Spina: A História da Plástica em Z na Queiloplastia Para a Correção das Fissuras Lábio-Palatinas Unilaterais. Rev Bras Cir Plást. 2005;20(4):245-7.
15. Mohler LR. Unilateral cleft lip repair. Plast Reconst Surg. 1987;80(4):511-7. DOI: http://dx.doi.org/10.1097/00006534-198710000-00005
16. Bonato Jr A. Fissura labiopalatal unilateral. In: Mélega JM, ed. Cirurgia plástica fundamentos e arte - cirurgia reparadora de cabeça e pescoço. Rio de Janeiro: Medsi; 2002. p.126-39.
17. McComb H. Primary correction of unilateral cleft lip nasal deformity: a 10-year review. Plast Reconstr Surg. 1985;75(6):791-9. PMID: 4001197 DOI: http://dx.doi.org/10.1097/00006534-198506000-00003
18. Raposo-do-Amaral CE. Avaliação do percentual de assimetria labial e nasal em pacientes com fissura lábio-palatina submetidos a queiloplastia primária. Rev Bras Cir Plást. 2010;25(1):38-48.
19. Luna ICG, Coutinho AL, Pereira R, Salgado I, Cardozo K, Albuquerque RW. Deiscência em cirurgia de fissura labiopalatina: perfil clínico-epidemiológico. Rev Bras Cir Plást. 2012;27(3supl):41.
20. McCarthy GJ, Cutting CB, Hogan VM. Introduction to facial clefts. In: McCarthy JG, ed. Plastic surgery: cleft lip & palate and craniofacial anomalies. Philadelphia: W.B. Saunders; 1990. p.2437-50.
21. Ronche-Ferreira JC, Minami E. Introdução ao estudo das fissuras labiopalatais. In: Mélega JM, ed. Cirurgia Plástica Fundamentos e Arte - cirurgia reparadora de cabeça e pescoço. Rio de Janeiro: Medsi; 2002. p. 3-7.
22. Figueiredo JCA, Freitas AG. Fissuras labiais. In: Mélega JM, ed. Cirurgia plástica fundamentos e arte - cirurgia reparadora de cabeça e pescoço. Rio de Janeiro: Medsi; 2002. p. 89-109.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Associação Brasileira de Cirurgia Crânio-Maxilo-Facial, São Paulo, SP, Brazil
3. Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS, Brazil
4. Hospital SOBRAPAR - Crânio e Face, Campinas, SP, Brazil
Institution: Hospital Pediátrico Professor Heriberto Bezerra, Universidade Federal do Rio Grande do Norte, Brazil.
Corresponding author:
Leonardo Santos de Barros Spencer
Av. Borges de Medeiros, 3160, Apto 401 - Praia de Belas
Porto Alegre, RS, Brazil Zip Code 90110-150
E-mail: contato@drleonardospencer.med.br
Article received: August 6, 2015.
Article accepted: November 11, 2015.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter