

Original Article - Year 2016 - Volume 31 -
Labiaplasty and its current status
Plástica de pequenos lábios e suas possibilidades atuais
ABSTRACT
INTRODUCTION: Nymphoplasty or labiaplasty consists of a surgical approach to hypertrophy of the labia minora, and is aimed at correcting asymmetry and removing redundant tissue of the vulva. Hypertrophy of the labia minora is characterized by tissue that exceeds the limits of the labia majora under normal conditions. Surgery is an option in patients who complain of unpleasant odor, urinary infection, interference with sexual activity, and/or personal dissatisfaction; in the latter case, the surgical indication has an aesthetic purpose. The aim of this article was to report our experience with wedge resection of the labia minora in patients with hypertrophy.
METHODS: We retrospectively analyzed 53 cases of labiaplasty performed with the wedge resection technique from 2010 to 2015. The results were evaluated for postoperative anatomical appearance, the degree of patient satisfaction, and the effect on sexual activity.
RESULTS: Patients were satisfied with the postoperative aesthetic appearance. There was improvement in sexual satisfaction, ability to perform physical activities, and hygiene. No complications were observed, such as suture dehiscence, infection, or tissue necrosis. One patient required reoperation in the postoperative period due to asymmetry of the labia minora. Another patient complained of excessive exposure of the clitoris, but she had preexisting clitoral hypertrophy.
CONCLUSION: Labiaplasty using the wedge resection technique relieved personal discomfort and provided functional and aesthetic improvement. Due to the lack of validation and standardization of labiaplasty techniques, further clinical research should be performed.
Keywords: Vulva/abnormalities; Hypertrophy; Surgical reconstructive procedures.
RESUMO
INTRODUÇÃO: A ninfoplastia consiste na abordagem cirúrgica da hipertrofia dos pequenos lábios, que visa ao aperfeiçoamento da assimetria destes e do tecido redundante da vulva. A hipertrofia de pequenos lábios caracteriza-se por aqueles que, em posição e condições normais, sobressaem-se aos grandes lábios. A cirurgia tem sido proposta na presença de transtornos, como odor desagradável, infecção urinária, comprometimento da atividade sexual e/ou insatisfação pessoal, cuja indicação cirúrgica possui fins estéticos. O objetivo deste artigo é relatar nossa experiência com a ressecção em cunha dos pequenos lábios nas pacientes que apresentam tal hipertrofia.
MÉTODOS: Foram analisados retrospectivamente 53 casos de ninfoplastia pela técnica de ressecção em cunha, no período de 2010 a 2015. Os resultados foram analisados quanto ao aspecto anatômico no pós-operatório, o grau de satisfação das pacientes e a interferência na atividade sexual.
RESULTADOS: As pacientes se mostraram satisfeitas com o aspecto estético pós-cirúrgico. Houve melhora no desempenho sexual, na prática de atividades físicas e condições de higiene. Não foram verificadas complicações, como deiscência de sutura, infecção ou necrose tecidual. Uma paciente precisou ser reoperada devido à assimetria de pequenos lábios no pós-operatório. Outra paciente queixou-se da excessiva exposição do clitóris, porém o mesmo já apresentava discreta hipertrofia prévia.
CONCLUSÃO: A ninfoplastia pela técnica de ressecção em cunha apresentou benefícios em relação ao desconforto pessoal, melhora funcional e estética. Devido à ausência de validação e padronização nas técnicas de ninfoplastia atuais, novos estudos clínicos devem ser realizados.
Palavras-chave: Vulva/anormalidades; Hipertrofia; Procedimentos Cirúrgicos Reconstrutivos.
Nymphoplasty or labiaplasty consists of the surgical correction of hypertrophy of the labia minora (Figure 1). This surgery aims to correct asymmetry of the labia minora and to remove redundant tissue of the vulva, in order to enhance function and aesthetics1,2. There is no consensus on the definition of hypertrophy of the labia minora; however, there has been an attempt at classification when the labia minora exceed the limits of the labia majora under normal conditions3.
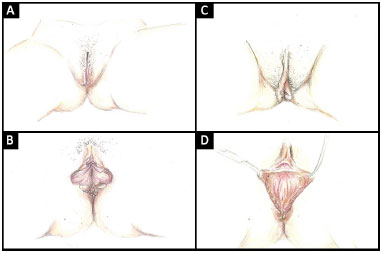
Figure 1. Schematic drawings; A: Vulva showing anatomical relationship of labia majora and labia minora; B: Hypertrophy of labia minora with accentuated protrusion; C: Hypertrophy of labia minora with moderate protrusion; D: Perioperative appearance for correction of hypertrophy of labia minora.
Some authors define hypertrophy when the maximum width between the midline and the free lateral border of the labia minora exceeds 4-5 cm4,5. More recently, other authors have proposed reducing this distance to 3-4 cm4,6.
The hypertrophy can cause various disorders. These include: inflammation, compromised genital hygiene, interference with sexual activity because of dyspareunia, low self-esteem, emotional distress, and even the need for intermittent self-catheterization in women with myelodysplasia7. Such a problem should therefore be approached with seriousness, care, and psychological support for the patient, since it is an area of significant emotional impact8, particularly in the adolescent population9.
In most cases, hypertrophy of the labia minora has no specific etiology. However, Barrett and Carlson10 proposed a specific mechanism to explain the appearance of hypertrophy. These authors attribute hypertrophy to lymphangiectasia, which includes a group of disorders characterized by dilation of lymphatic channels and insufficient lymphatic drainage11.
Lymphangiectasia may be congenital, with late or acquired manifestations12. Acquired lymphangiectasia may be secondary to Crohn's disease, fibroepithelial polyps, external trauma in the vulvar region, exaggerated weight gain, chronic irritation, or endogenous or exogenous androgen hormone action6,13,14. This theory is supported by recurrence after surgery15.
Although there are no standard diagnostic criteria for hypertrophy of the labia minora, surgery has been proposed in the presence of chronic symptoms. These include unpleasant odor, urinary infection, and interference with sexual activity14,15.
In the absence of these symptoms, personal dissatisfaction is a surgical indication for aesthetic purposes. However, anatomical differences are common, and hypertrophy of the clitoral hood is often associated with an increase in the labia minora. These changes, if not managed properly, limit the results, producing negative aesthetic and functional sequelae1.
Since the introduction of labiaplasty, a range of surgical techniques has been reported in the literature. These include deepithelialization, direct excision, W-shaped resection, wedge resection, Z-plasty, and laser labiaplasty. The essential objectives of these procedures include the reduction of hypertrophied labial volume, with maintenance of the neurovascular bundles, color, and texture, as well as preservation of the introitus and labial contours16.
The deepithelization technique consists of the removal of a small portion of tissue, as long as the labial contour is preserved. This technique is more suitable for patients with minimal hypertrophy of the labia minora. The direct excision technique produces a poor aesthetic result, since the natural color, contour, and texture of the tissue is lost; this technique uses a simple approach, aiming only to reduce volume.
W-shaped resection and Z-plasty are a type of tissue reconstruction using rotational flaps, and guarantees a good aesthetic outcome. The wedge resection technique is comparable to direct excision with regard to volume reduction; however, the labial contour is preserved17. It is of great importance to emphasize that the choice of technique depends on several factors such as: the objective of the surgery, what the patient's anatomy allows, and the experience and comfort of the surgeon in performing each technique16.
OBJECTIVE
In this study, we present our experience with the resection of labia minora using the wedge resection technique, in patients in whom the labia minora exceed the limits of the labia majora when examined in orthostatic position with the thighs abducted.
METHODS
This article is based on a retrospective study of 53 cases of female genital plastic surgery performed from January 2010 to December 2015 at the University Hospital of the Federal University of Juiz de For a, and in the Plastic Center - Plastic Surgery Clinic, a private clinic located in the city of Juiz de Fora, Minas Gerais.
The age of the patients ranged from 14 to 45 years, with a mean age of 25 years. Oral contraceptives were used by 88% of the women, and the body mass index (BMI) ranged from 22 to 32. Patients with local wounds or active infection were excluded. The same surgical technique was used to correct hypertrophy of the labia minora, and consisted of wedge resection of excess tissue, without loss of the patient's natural labial contour.
The patients were placed in the lithotomy position. Surgical marking of the excess to be removed in wedge form was performed with indelible ink, malachite green, or methylene blue, each case being individualized.
Surgery commences after placement of suture wires or hemostatic clamps on the front and back of the labia minora. An incision is made with a number 15 blade, followed by removal of excess skin with a Metzenbaum curved scissors; then, continuous over and over suture is performed, approaching the edges; 4-0 catgut or 3-0 polyglactin 910 is used for closure.
In all patients, regardless of the anesthesia, local infiltration was used, with lidocaine 2%, bupivacaine 0.25%, and adrenaline at a concentration of 1:200,000, always with moderate infiltration, because the tissue of the region is flaccid and easily deformable. Hemostasis was performed with a high frequency scalpel with strict control.
The patients were kept in the hospital for 6 to 12 hours, depending on the type of anesthesia, the association with other surgeries or hospitalization, and the distance from their residence.
In isolated labia minora surgery, sedation with local anesthesia was used, with general anesthesia being reserved only for associated surgeries. The most frequent associated surgeries were reduction mammoplasty, silicone breast implantation, and liposuction.
In the postoperative period, rest, cold packs for the first 24 hours, and topical antiseptic and gynecological ointments were prescribed. The following antibiotic regimen was used: a single intravenous dose of cefazolin 1 g at anesthetic induction, repeated every 8 hours for two doses, or cefadroxil 500 mg orally every 12 hours for four days. Supplementary nonsteroidal anti-inflammatory medication was prescribed, and sexual abstinence was recommended for four weeks.
The patients were followed up at 7 days, 14 days, 2 months and 6 months, in the absence of new interventions or complications. The results were analyzed objectively, based on the postoperative anatomical appearance, and subjectively, by means of a questionnaire. The two questions inquired about the degree of satisfaction and the effect on intercourse.
RESULTS
All patients were satisfied with the aesthetic appearance of the labia minora. They reported better hygiene and improvement in performance of physical activities. None reported any negative effects on intercourse, but in fact reported improvement in sexual activity. One patient required reoperation in the postoperative period due to asymmetry of the labia minora. Another complained of excessive exposure of the clitoris; however, this patient had slight clitoral hypertrophy even before the surgical procedure. The clitoral hood was not approached in the surgery; however, there were no complaints of hypersensitivity.
The anatomical appearance was considered good, and there was no visible evidence of surgery (Figure 2), documented with routine pre and postoperative pictures. Moreover, there were no complications related to the procedures, such as suture dehiscence, infection, or tissue necrosis.
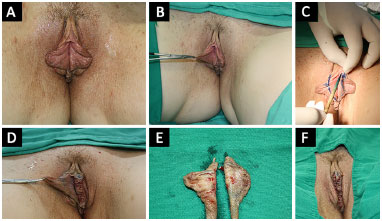
Figure 2. Corrective surgery for hypertrophy of labia minora; A: Preoperative appearance of hypertrophy of the labia minora; B: Preoperative appearance of hypertrophy of the labia minora; C: Preoperative marking with methylene blue; D: Perioperative appearance of surgery for hypertrophy of the labia minora; E: Surgical specimen; F: Immediate postoperative appearance.
DISCUSSION
There are few reports on the surgical treatment of hypertrophy of the labia minora, which makes it difficult to compare the results obtained by other practitioners. The number of these reports will increase as the demand for the procedure increases. This leads us to question whether this small number of reports is due to low demand, or the lack of plastic surgeons who perform the surgery.
It is important to emphasize that hypertrophy of the labia minora can be congenital or acquired as a result of chronic irritation, exaggerated weight gain, or endogenous or exogenous hormonal (androgenic) action. For any one of these, there are several surgical techniques applicable for correction of hypertrophy8.
Triana states that despite the numerous techniques described, wedge resection of excess tissue provides satisfactory results for the vast majority of patients2,18. However, new techniques have been developed, with functional and aesthetic results similar to those of currently used methods. In the future, new techniques must be constantly developed, in order to reduce the stigma related to hypertrophy of the labia minora.
Zwang19 believes that the requests for reconstruction will cease only when women become sufficiently informed about the appearance of the external genitalia, and understand that there is no uniform external appearance. On the other hand, Fitzpatrick20 states that if women are not satisfied with the appearance of their genitalia, they can request surgical intervention, which is why labiaplasty procedures have increased by 20% annually in the past few years.
With the increased exposure of female genitalia in magazines, films, novels, the arts, the internet, and other media, women may observe natural differences in external genital anatomy, make comparisons, and identify a more aesthetically pleasing appearance. The cult of the body associated with the improvement of female self-esteem is an important factor in obtaining personal satisfaction when patients seek the assistance of plastic surgery to improve body contour8.
The request for surgical treatment of the labia minora when a surgical indication is not present is also common in plastic surgery outpatient clinics. Patients may be motivated by the desire to tell friends or relatives about their intimate surgery.
Many of these candidates for surgery do not have asymmetry of the labia minora, or symptoms that indicate or justify a surgical procedure. These patients should be referred for psychological support. According to Zwang21, the physician's role is to apply professional ethical standards by declining to perform surgery prompted by body dysmorphic disorder.
CONCLUSION
Wedge resection labiaplasty is a simple and safe procedure, with low complication rates. It is an easily reproducible procedure with optimal results and a high degree of patient satisfaction. The present study documented relief of personal and social distress, as well as functional and aesthetic improvement.
Nevertheless, labiaplasty should be approached with discretion and care, and surgeons should use a technique with which they have greater experience and comfort, despite the many techniques described. The increase in this surgical procedure is mainly due to the increased exposure of the female genitalia in the media.
Caution is advised when suggesting surgery in cases of slight hypertrophy or asymmetry of the labia minora without a medical indication, due to the risks inherent in any surgical procedure, and possible complications.
New procedures and surgical refinements are emerging, with results similar to those already proposed, but no significant differences in postoperative or final outcome. However, it should be emphasized that there is no standardization of current surgical practice. Therefore, new clinical studies should be performed to validate the available techniques and define the best management of patients who undergo labiaplasty.
ACKNOWLEDGEMENTS
The authors thank Andiara Barbosa Neder, graduate in Art and Design at the Federal University of Juiz de Fora (UFJF), for the illustrations included in this article.
COLLABORATIONS
MTD Analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
MPDC Analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
ALRM Analysis and/or interpretation of data; final approval of the manuscript; drafting the manuscript or critical review of its contents.
MBC Analysis and/or interpretation of data; final approval of the manuscript; drafting the manuscript or critical review of its contents.
ALN Analysis and/or interpretation of data; final approval of the manuscript; drafting the manuscript or critical review of its contents.
LDC Analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; drafting the manuscript or critical review of its contents.
GVD Analysis and/or interpretation of data; statistical analysis; drafting the manuscript or critical review of its contents.
LVD Analysis and/or interpretation of data; final approval of the manuscript; drafting the manuscript or critical review of its contents.
REFERENCES
1. Daher M, Muñiz AR, Daher AC, Vanzan K, Monteiro G, Maciel J, et al. Star nymphoplasty: a surgical technique for labia minora hypertrophy. Rev Bras Cir Plást. 2015;30(1):44-50.
2. Triana L, Robledo AM. Refreshing labioplasty techniques for plastic surgeons. Aesthetic Plast Surg. 2012;36(5):1078-86.
3. Farahani F, Gentry A, Lara-Torre E, McCuin E. Self-attempted labioplasty with elastic bands resulting in severe necrosis. J Low Genit Tract Dis. 2015;19(2):e35-7.
4. Rouzier R, Louis-Sylvestre C, Paniel BJ, Haddad B. Hypertrophy of labia minora: experience with 163 reductions. Am J Obstet Gynecol. 2000;182(1 Pt 1):35-40.
5. Radman HM. Hypertrophy of the labia minora. Obstet Gynecol. 1976;48(1 Suppl):78S-79S.
6. Munhoz AM, Filassi JR, Ricci MD, Aldrighi C, Correia LD, Aldrighi JM, et al. Aesthetic labia minora reduction with inferior wedge resection and superior pedicle flap reconstruction. Plast Reconstr Surg. 2006;118(5):1237-47.
7. Choi HY, Kim KT. A new method for aesthetic reduction of labia minora (the deepithelialized reduction of labioplasty). Plast Reconstr Surg. 2000;105(1):419-22.
8. Cunha FI, Silva LM, Costa LA, Vasconcelos FRP, Amaral GT. Ninfoplastia: classificação e refinamentos técnicos. Rev Bras Cir Plást. 2011;26(3):507-11.
9. Reddy J, Laufer MR. Hypertrophic labia minora. J Pediatr Adolesc Gynecol. 2010;23(1):3-6.
10. Barrett MM, Carlson JA. A clinicopathologic study of labia minora hypertrophy: signs of localized lymphedema were universal. J Low Genit Tract Dis. 2014;18(1):13-20.
11. Proujansky R. Pediatric Gastrointestinal Disease. 3rd ed. Ontario: BCDecker; 2000. p. 194-202.
12. Heller DS, Kuye OO. Recurrent hypertrophy of the labia minora: a hormonally related lesion possibly related to fibroepithelial stromal polyps of the vulva. J Low Genit Tract Dis. 2011;15(1):69-70.
13. Filassi JR, Munhoz AM, Ricci MD, Melo NR. Aplicação do retalho labial superior para a correção cirúrgica da hipertrofia de pequenos lábios. Rev Bras Ginecol Obstet. 2004;26(9):735-9.
14. Vieira-Baptista P, Lima-Silva J, Beires J. Intimate surgery: what is done and under which scientific bases? Acta Obstet Ginecol Port. 2015;9(5):393-9.
15. Wu JA, Braschi EJ, Gulminelli PL, Comiter CV. Labioplasty for hypertrophic labia minora contributing to recurrent urinary tract infections. Female Pelvic Med Reconstr Surg. 2013;19(2):121-3.
16. Miklos JR, Moore RD. Labiaplasty of the labia minora: patients' indications for pursuing surgery. J Sex Med. 2008;5(6):1492-5.
17. Motakef S, Rodriguez-Feliz J, Chung MT, Ingargiola MJ, Wong VW, Patel A. Vaginal labiaplasty: current practices and a simplified classification system for labial protrusion. Plast Reconstr Surg. 2015;135(3):774-88.
18. Laufer MR, Galvin WJ. Labia hypertrophy: a new surgical approach. Adolesc Pediatr Gynecol. 1995;8(1):39-41.
19. Zwang G. Atlas du sexe de la femme. Paris: La Musardine; 2001.
20. Fitzpatrick L. Plastic surgery below the belt. Time Magazine; 2008 Nov 19. Citado 2016 Nov 10]. Disponível em: http://content.time.com/time/health/article/0,8599,1859937,00.html
21. Zwang G. Vulvar reconstruction. The exploitation of an ignorance. Sexologies. 2011;20(2):81-7.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Faculdade de Medicina, Universidade Federal de Juiz de Fora, Juiz de Fora, MG, Brazil
3. Hospital Universitário, Universidade Federal de Juiz de Fora, Juiz de Fora, MG, Brazil
4. Faculdade Ciências Médicas e da Saúde de Juiz de Fora, MG, Brazil
Institution: Hospital Universitário, Universidade Federal de Juiz de Fora, Juiz de Fora, MG, Brazil.
Corresponding author:
Marilho Tadeu Dornelas
Avenida Eugênio do Nascimento s/nº - Dom Bosco
Juiz de Fora, MG, Brazil Zip Code 36038-330
E-mail: marilho.dornelas@ufjf.edu.br
Article received: August 25, 2013.
Article accepted: October 30, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter