

Original Article - Year 2016 - Volume 31 -
Versatility of the medial gastrocnemius muscle flap in reconstructing lower limb soft tissue lesions
Versatilidade do uso do retalho do músculo gastrocnêmio medial na reconstrução de lesões de partes moles de membros inferiores
ABSTRACT
INTRODUCTION: Covering complex lower limb wounds is a major challenge. The medial gastrocnemius muscle flap is usually indicated for reconstruction of loss of substance of the knee and proximal third of the leg. The objective of this study was to evaluate the results using gastrocnemius muscle flaps in lower limb wounds.
METHODS: A total of 28 patients with loss of substance in the lower limbs were treated with medial gastrocnemius muscle flaps. Data were obtained from clinical records of patients who underwent surgery from 2003 to 2012.
RESULTS: In 28 patients who underwent surgery, the age range was 4 to 57 years, with a mean of 30.6 years. The etiology of the lesions was a motorcycle accident in 16 cases (57.1%), being run over in 8 cases (28.6%), car crash in 2 cases (7.2%), meningococcemia in 1 case (3.6%), and snake bite in 1 case (3.6%). After an average follow-up of 15 months (range: 6 to 26 months), all patients had stable coverage. The mean number of preoperative debridements was 2.4 (range: 1 to 8). In 22 patients, the flaps were made without the release of the muscle origin and in 6 patients the muscle flaps were separated from their origin in the femur.
CONCLUSIONS: Transfer of a gastrocnemius muscle flap is a simple and safe procedure in the treatment of lower limb injuries. The application of the medial gastrocnemius muscle flap was demonstrated in different situations, with satisfactory results and easy reproducibility.
Keywords: Surgical flaps; Skeletal muscle; Legs; Leg injuries; Wounds and injuries; Traumatic amputation
RESUMO
INTRODUÇÃO: A cobertura de feridas complexas de membros inferiores é um grande desafio. O retalho muscular do gastrocnêmio medial é comumente indicado para reconstrução de perdas de substância do joelho e terço proximal da perna. O objetivo desse trabalho é avaliar os resultados da utilização do retalho muscular do gastrocnêmio nos casos de ferida em membros inferiores.
MÉTODOS: Um total de 28 pacientes com perda de substância de membros inferiores foi tratado com retalho muscular do gastrocnêmio medial. Os dados foram obtidos em registros clínicos dos pacientes operados no período de 2003 a 2012.
RESULTADOS: Vinte e oito pacientes foram operados, com idades variando de 4 a 57 anos, e média de 30,6 anos. A etiologia das lesões foi acidente por motocicleta em 16 casos (57,1%), atropelamentos em oito casos (28,6%), acidente automobilístico em dois casos (7,2%), meningococcemia em um caso (3,6%) e acidente ofídico em um caso (3,6%). Depois de um seguimento médio de 15 meses (variação de 6 a 26 meses), todos pacientes mostraram cobertura estável. O número médio de desbridamentos pré-operatórios foi 2,4 (variação de 1 a 8). Em 22 pacientes, os retalhos foram confeccionados sem a liberação da origem muscular e em seis pacientes os retalhos musculares foram separados de sua origem no fêmur.
CONCLUSÕES: A transferência do retalho muscular do gastrocnêmio é um procedimento simples e seguro no tratamento de lesões de membros inferiores. Foi demonstrada a aplicação do retalho muscular do gastrocnêmio medial em diferentes situações, com resultados satisfatórios e fácil reprodução.
Palavras-chave: Retalhos cirúrgicos; Músculo esquelético; Pernas; Traumatismos da perna; Ferimentos e lesões; Amputação traumática.
Lower limb wounds have a range of presentations and are usually caused by high-energy trauma, with extensive cutaneous loss and impaired tissue viability, amputations of limbs or fingers, lacerations, and crushing and exposure of tissues. Over the last 30 years, advances in reconstructive surgery, such as the development and use of pedicled fasciocutaneous/muscle flaps and the introduction of microsurgery, have broadened the therapeutic arsenal of the plastic surgeon and evolved in the treatment of traumatic lesions1,2.
The evaluation, follow-up, and surgical treatment of these complex lesions are performed by a multidisciplinary team, with essential involvement of the plastic surgeon. Functional recovery should always be sought, regardless of the proposed treatment, reconstruction, or amputation1,2.
The reconstruction of lower limbs remains a challenge for plastic surgeons. The anatomical features, such as lack of soft tissue and thin skin, lead to great difficulty in treating soft tissue injuries in this location3.
The medial gastrocnemius muscle flap is well known for its reliability in lower limb reconstruction, especially in bone and prosthesis exposures in the knee, as well as in the upper third of the leg4,5. However, this pedicle-elevated muscle flap has proven very versatile and can be used in the reconstruction of other regions of the lower limbs.
OBJECTIVE
The objective of this study was to present the experience of the Plastic Surgery Service of the Regional Hospital of Asa Norte (Brasília, DF) in the treatment of lower limb injuries using the gastrocnemius muscle flap, from 2003 to 2012.
METHODS
This was a retrospective study of all patients admitted to the Plastic Surgery Service of the Regional Hospital of Asa Norte who underwent reconstruction of the lower limbs in the period from 2003 to 2012 due to loss of cutaneous cover, by using a flap from the medial head of the gastrocnemius muscle.
These patients were admitted electively after clinical/surgical management of their wounds by other specialties, such as orthopedics and general surgery. The following variables were evaluated: gender, age, trauma etiology, presence and location of a fracture, characteristics of the loss of substance, and presence of bone exposure.
The study included patients who were treated at the Plastic Surgery Service of the Regional Hospital of Asa Norte for lower limb wounds during the study period, and who underwent reconstruction with flaps from the medial head of the gastrocnemius muscle.
Exclusion criteria were hemodynamic instability, tibial nerve lesions, or lesions in the donor area.
Debridements of the lower limb lesions were performed using one or more methods, in order to obtain a clean wound without secretions or areas of macroscopic necrosis, with less fibrotic tissue.
Participants were exempted from providing informed consent since this was a retrospective study. The study was approved by the Research Ethics Committee of the State Department of Health of the Federal District (CAAE number: 47391715.6.0000.5553, opinion number: 1.167.841).
Surgical technique
The elevation of the flap of the medial head of the gastrocnemius begins with a longitudinal incision in the posterior region of the leg between the 2 bellies of the muscle. Care is taken to identify the sural nerve and the small saphenous vein as lateral borders of the medial head of the gastrocnemius muscle. Distally, the aponeurosis is separated from the medial head of the gastrocnemius by the Achilles tendon. The belly of the medial head is released in the midline. Laterally, the lateral head of the gastrocnemius is found, followed by the soleus.
The posterior and lateral dissection of the medial head of the gastrocnemius is uncomplicated. The tendon origin of the medial head of the gastrocnemius in the femur can be sectioned with preservation of the artery and medial sural vein, increasing the arc of rotation of this muscle flap. Muscle denervation is performed with the dissection of the sural nerve at the medial head of the gastrocnemius.
RESULTS
The study sample consisted of 28 patients with complex lower limb wounds treated with a muscle flap of the medial head of the gastrocnemius. The mean age of the patients at the time of initial treatment was 30.6 years, ranging from 4 to 57 years. Males accounted for 71.4% of the sample (Table 1). The mean number of preoperative surgical debridements was 2.4 (range: 1 to 8).
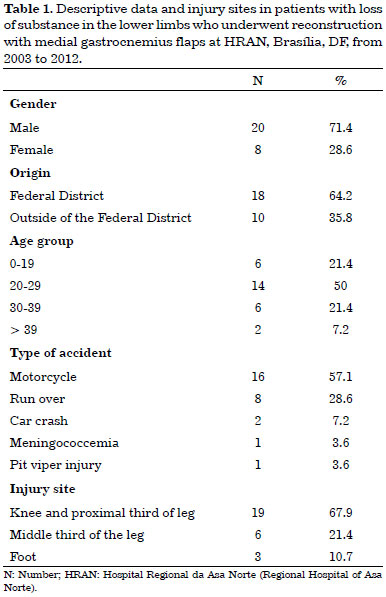
The etiology of loss of lower limb substance included motorcycle accidents (57.1%), being run over (7.2%), car crash (7.2%), meningococcemia (3.6%), and pit viper injury (3.6%) (Table 1). The loss of substance was most common in the upper third of the leg and knee (67.9%), the middle third of the leg (21.4%), the dorsum of the foot (7.2%), and the plantar region (3.6%) (Figures 1 to 3). No fracture was present in 71.4%, while 28.6% had a tibial or metatarsal fracture. All patients had bone and/or tendon exposure (Figure 4).
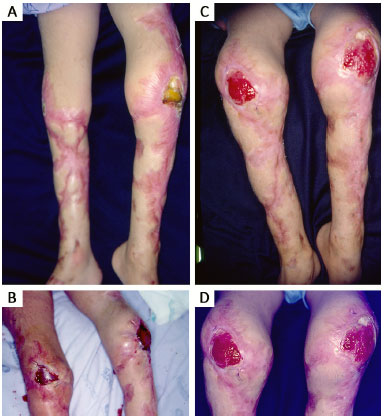
Figure 1. A: A 6-year-old child with bilateral patellar exposure, mainly om the left, due to meningococcemia; B: Use of the medial gastrocnemius muscle flap bilaterally, at 2 postoperative days; C: 40 postoperative days; D: Detail of coverage of the bilateral patellar region with medial gastrocnemius muscle flaps.

Figure 2. A: An 8-year-old child who was run over, with metatarsal exposure on the dorsum of the foot; B: Coverage of bone exposure of the dorsum of the foot with medial gastrocnemius muscle flap from the contralateral leg (cross-leg).
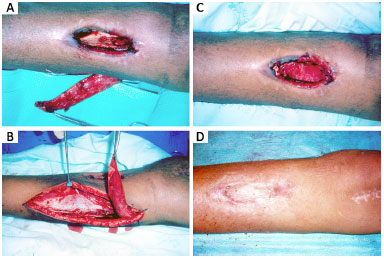
Figure 3. A: A 17-year-old victim of a motorcycle accident with bone exposure of the tibia, with release of a segment of the medial gastrocnemius to cover the lesion; B: The segment of the medial head of the gastrocnemius muscle will pass under the skin tunnel to the patient's exposed bone; C: Placement of the flap over the bone exposure area; D: Skin graft on the muscle flap at 95 postoperative days.

Figure 4. A: A 24-year-old victim of a pit viper injury with loss of substance in the plantar region, and with bone exposure and retraction when flexing the hallux; B: Detail of elevation of the medial gastrocnemius muscle flap; C: Immobilization of the legs with plaster to allow the integration of the muscle flap in cross-leg position; D: Coverage of loss of substance with medial gastrocnemius muscle flap after release of cross-leg position. Correction of hallux retraction by release of the flexor of this toe; E: Skin graft on the muscle flap at 35 postoperative days.
The surgical complications included partial loss of the flap in 2 (7.1%) cases. It was necessary to associate the muscle flap of the medial head of the gastrocnemius with other flaps in 6 cases (21.5%). In the other cases, the flap was adequate to cover the lesion, enabling a good esthetic and functional result.
DISCUSSION
The medial gastrocnemius muscle flap has been used in a more standardized way since the 1970s for lower limb reconstruction4,5. It is one of the most commonly used flaps to cover losses of substance of the knee, proximal third of the leg, and distal third of the thigh. The advantages of the flap are the presence of a constant, safe, and reliable vascular pedicle, with satisfactory width and length of the muscle. In addition, the optimal arc of rotation of the muscle and its plasticity allows closure without tension, and the coverage of injuries in most cases6,7.
The medial gastrocnemius muscle is characterized by being biarticular, comprising part of the structure of the triceps surae, along with the soleus and the lateral head of the gastrocnemius. Its function is to perform plantar flexion of the ankle, besides contributing to the circulation of the posterior cutaneous territory of the leg through at least 2 perforating vessels8. The resection of only one belly of the gastrocnemius does not impair plantar flexion and does not cause major deformity9. The easy dissection has a rapid learning curve.
The medial head of the gastrocnemius muscle has an average length of 20 cm (range: 19 to 23 cm) and a width of 6.5 cm (range: 4.5 to 9 cm), which allows a wide arc of rotation and good coverage of exposed bone of the leg and knee. The vascular pedicle has an average length of 4.5 cm, and the average area of a medial gastrocnemius flap is 32.5 cm2 (range: 22.3 to 47.5 cm2)7,8.
The main indications for use of the gastrocnemius flap are coverage of lesions in the knee and in the upper third of the leg. Indications also include tibial plateau fractures with bone exposure, prosthesis coverage in knee arthroplasty, and coverage of exposed bone and metal in the knee and upper third of the leg after amputation or treatment of tumors10,11. In the present study, we encountered other indications for the pedicled gastrocnemius muscle flap, such as coverage of patellar exposure after meningococcemia (Figure 1).
In addition, the pedicled gastrocnemius muscle flap may be used in association with a fasciocutaneous flap to cover bone exposure in the middle third of the leg. In cases of loss of substance on the dorsum of the foot, the flap can be used crosswise (cross-leg) (Figure 2).
The use of the medial gastrocnemius as a cross flap (cross-leg) to cover loss of substance on the dorsum of the foot and plantar region is not the first choice, as we usually have other good options1-3,12, but the crossleg flap may be the only viable pedicled flap in special cases (Figure 5).

Figure 5. Detail of release of the origin of the medial gastrocnemius at the medial condyle of the femur.
Most patients in the present study were young adults with a mean age of 31 years, since the main etiology of the lesions treated in this study was trauma caused by a motorcycle accident (Table 1). Another study reported a mean age of 49 years in patients treated with the medial gastrocnemius flap, but 57.8% of the cases were for resection of tumors, mainly sarcomas13.
The anatomy of the medial gastrocnemius muscle has been extensively studied and the muscle is not only used as a local flap in the lower limbs. The skin that covers this muscle can be used as a skin flap, based on the perforators of the medial gastrocnemius muscle8. In addition, the use of free flaps of the medial gastrocnemius as motor units for the upper limb has been reported9,14.
Anatomical studies have demonstrated a constant intramuscular vascular pattern in the gastrocnemius. This pattern consists of a sural artery for each head, which usually divides into the proximal portion of the belly as 2 longitudinal terminal branches. These findings allow the longitudinal separation of the 2 distal thirds of each muscle belly into 2 equal segments without compromising blood flow (Figure 3).
This technique of segmentation of the gastrocnemius muscle head can be used in specific situations, for example, in the presence of a deep bone defect after a gunshot injury or in a patient with chronic osteomyelitis. In these cases, it is possible to fill the cavity with one of the muscle segments and cover the area with the other segment, so that the first segment increases the blood supply to the injury site, and the other segment serves as the basis for the skin graft15.
To access the gastrocnemius muscle, we prefer a posterior incision in the midline of the leg between the two heads of the muscle, rather than a medial incision in the leg, since this allows better visualization of the pedicle (Figure 5). In this way, a wider muscle elevation and release can be achieved, especially in the region of the pes anserinus.
This observation was confirmed by a study of fresh cadavers. The posterior incision between the two heads of the gastrocnemius in the midline allows a 2.02-cm greater advancement of the flap than that made by a medial incision (on the medial side of the leg, 2 cm posterior to the medial border of the tibia), resulting in a larger coverage area for the gastrocnemius flap6,16.
In 6 patients, it was necessary to release the femoral origin of the muscle to increase the arc of rotation of the muscle flap (Figure 5). In a recent anatomical study, Veber et al.7 observed that the release of the gastrocnemius from its origin in the femur and the dissection of the pes anserinus increase the arc of rotation of the medial gastrocnemius flap in 30 to 50%. The pes anserinus (tendon of the sartorius, gracilis, and semitendinosus muscles) may limit the rotation of the medial head of the gastrocnemius. Therefore, sectioning the origin of the medial head of the gastrocnemius at the medial condyle of the femur and/or the tendons of the pes anserinus is a way to increase the arc of rotation of this flap6,7.
In the present study, the flap was not made with the lateral head of the gastrocnemius muscle. This flap has a risk of peroneal nerve compression. In order to avoid nerve compression, the muscle must be transposed under the peroneal nerve. The retractors should be positioned carefully and excessive pressure should be avoided. The incidence of peroneal nerve palsy in the gastrocnemius lateral head flaps is 7.7 to 12.5%6,13,17.
As advocated by other authors13,17, we recommend and perform denervation of the medial gastrocnemius flap. This procedure allows good contour of atrophied muscle over time, reduces the risk of early wound dehiscence, and reduces pain associated with muscle contraction. In addition, contraction of the medial gastrocnemius flap may lead to intermittent occlusion of the popliteal vein, as observed by Cho18 in 2 cases.
The complication rate in the present study was 7.1%, compatible with that in other studies6,13,17. The risk of necrosis of the flap is usually associated with undiagnosed vascular insufficiency (sural artery), and may be caused by trauma or inadequate postoperative care, especially regarding the patient's placement in bed.
With regard to morbidity in the donor area of the gastrocnemius flap, a self-evaluation questionnaire involving 82 patients found that 20% had pain when walking up to 50 m, 40% had pain when they walked more than 200 m, and 70% had pain and feeling of weakness in the operated leg when they ran13.
In the same study, a physical evaluation of 40 patients found that those who had a wound covered with a gastrocnemius flap had a 10 to 11% deficiency in ankle flexion and extension, as well as a 27% deficiency in knee flexion and 14% in knee extension.
In addition, in dynamometry testing of 34 patients, the maximum plantar flexion strength at the ankle was 76% in the operated leg, leading to a 24% reduction in resistance strength, compared to that in the non-operated leg. However, the observed deficiencies could be attributed to previous treatment (resection of tumors or placement of prostheses) and not to the flap. Even so, such morbidities were well tolerated13.
There are numerous alternatives to reconstruction of complex lesions, but it is essential to perform adequate surgical planning based on age, sex, profession, size of the loss, and location and magnitude of the trauma caused by a high-energy impact. Concern about the donor area and the quality of results in the recipient area is ongoing.
Along with free perforating flaps, the medial gastrocnemius flap has proven to be versatile and easy to perform, with wide applicability in the reconstruction of the lower limbs and a low rate of complications. In addition, the arc of rotation of the flap can be widened with the release of the muscular origin at the femoral condyle.
CONCLUSION
A flap using the medial head of the gastrocnemius has proven to be an option for coverage of areas of bone exposure in the knee, leg, and dorsal foot. The flap is versatile, easy to use, and has a low rate of complications.
COLLABORATIONS
JLSM Data analysis and/or interpretation; final approval of the manuscript; study conception and design.
SCR Data analysis and/or interpretation.
AAS Performed operations and/or experiments.
AVRFN Performed operations and/or experiments; manuscript writing or critical review of content.
PHSR Data analysis and/or interpretation; manuscript writing or critical review of content.
CS Data analysis and/or interpretation; manuscript writing or critical review of content.
REFERENCES
1. Al-Qattan MM. The reverse sural fasciomusculocutaneous "mega-high" flap: a study of 20 consecutive flaps for lower-limb reconstruction. Ann Plast Surg. 2007;58(5):513-6.
2. Franco D, D'Avila F, Arnaut Junior M, D'Avila B, Franco T. Tratamento das áreas cruentas de perna com retalhos locais. Rev Bras Cir Plást. 2015;30(2):264-72.
3. Garcia AMC. Retalho sural reverso para reconstrução distal da perna, tornozelo, calcanhar e do pé. Rev Bras Cir Plást. 2009;24(1):96-103.
4. McCraw JB, Fishman JH, Sharzer LA. The versatile gastrocnemius myocutaneous flap. Plast Reconstr Surg. 1978;62(1):15-23.
5. Feldman JJ, Cohen BE, May JW Jr. The medial gastrocnemius myocutaneous flap. Plast Reconstr Surg. 1978;61(4):531-9.
6. Arnold PG, Mixter RC. Making the most of the gastrocnemius muscles. Plast Reconstr Surg. 1983;72(1):38-48.
7. Veber M, Vaz G, Braye F, Carret JP, Saint-Cyr M, Rohrich RJ, et al. Anatomical study of the medial gastrocnemius muscle flap: a quantitative assessment of the arc of rotation. Plast Reconstr Surg. 2011;128(1):181-7.
8. Torres LR, Teixeira WGJ, Setani EO, Wei TH, Zumiotti AV. Retalho cutâneo das artérias perfurantes do músculo gastrocnêmio medial: estudo anatômico. Acta Ortop Bras. 2007;15(1):40-2.
9. Moraes FB, Paranahyba RM, Oliveira E, Kuwae MY, Rocha VL. Estudo anatômico do músculo gastrocnêmio medial visando transferência muscular livre functional. Rev Bras Ortop. 2007;42(8):261-5.
10. Pozzobon LR, Helito CP, Guimarães TM, Gobbi RG, Pécora JR, Camanho GL. Retalho de rotação para cobertura após artroplastia total do joelho. Acta Ortop Bras. 2013;21(4):219-22.
11. Souza FI, Zumiotti AV, Mattar Júnior R, Wei TH, Resende MR, Torres LR. Emprego do músculo gastrocnêmio no tratamento das lesões infectadas do joelho. Acta Ortop Bras. 2009;17(4):239-41.
12. Martins GB, Moreira AA, Viana FO. Reconstrução de lesões de partes moles do calcanhar com uso de retalhos fasciocutâneos. Rev Bras Cir Plást. 2009;24(1):104-9.
13. Daigeler A, Drücke D, Tatar K, Homann HH, Goertz O, Tilkorn D, et al. The pedicled gastrocnemius muscle flap: a review of 218 cases. Plast Reconstr Surg. 2009;123(1):250-7.
14. Liu XY, Ge BF, Win YM, Jing H. Free medial gastrocnemius myocutaneous flap transfer with neurovascular anastomosis to treat Volkmann's contracture of the forearm. Br J Plast Surg. 1992;45(1):6-8.
15. Moscona RA, Fodor L, Har-Shai Y. The segmental gastrocnemius muscle flap: anatomical study and clinical applications. Plast Reconstr Surg. 2006;118(5):1178-82.
16. Lamaris GA, Carlisle MP, Durand P, Couto RA, Hendrickson MF. Maximizing the Reach of the Pedicled Gastrocnemius Muscle Flap: A Comparison of 2 Surgical Approaches. Ann Plast Surg. 2016 May 23. [Epub ahead of print]
17. Pico R, Lüscher NJ, Rometsch M, de Roche R. Why the denervated gastrocnemius muscle flap should be encouraged. Ann Plast Surg. 1991;26(4):312-24.
18. Cho KO. Intermittent occlusion of the popliteal vein by a gastrocnemius rotational muscle flap. A report of two cases. J Bone Joint Surg Am. 2002;84-A(9):1659-63.
1. Faculdade de Medicina da Universidade de Brasília, Brasília, DF, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
3. Hospital Regional da Asa Norte, Brasília, DF, Brazil
Institution: Hospital Regional da Asa Norte, Brasília, DF, Brazil.
Corresponding author:
Jefferson Lessa Soares de Macedo
Quadra SQS 213, Bloco H, Apto 104 - Asa Sul
Brasília, DF, Brazil Zip Code 70292-080
E-mail: jlsmacedo@yahoo.com.br
Article received: January 12, 2016.
Article accepted: October 3, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter