

Original Article - Year 2016 - Volume 31 -
Surgical treatment of hidradenitis suppurativa with anterior and posterior lateral thoracic fasciocutaneous flaps
Tratamento cirúrgico de hidradenite supurativa com retalho fasciocutâneo torácico lateral anterior e posterior
ABSTRACT
INTRODUCTION: Hidradenitis suppurativa (HS) is a chronic, multifactorial, and often recurrent bacterial infection, affecting the skin and subcutaneous tissues. However, complete HS resolution can be achieved through surgical treatment. A series of patients with HS complications is described herein, along with their evolution and complications after complete axillary surgical resection and lateral thoracic fasciocutaneous flap rotation. The evaluation of associated affected areas is also reported.
METHODS: Between 2009 and 2014, 6 patients with an average age of 25.5 years (range: 15 to 35 years) underwent surgery for the treatment of HS. All patients had long-standing, chronic axillary lesions that were refractory to non-surgical treatment.
RESULTS: Six patients with HS (2 males and 4 females) underwent surgery. The average follow-up period was 16 months (range: 4 months to 5 years). Complete resolution was achieved and no HS recurrence was observed. Bilateral resection was performed in 4 cases, and unilateral resection in 2. Five patients also had inguinal involvement, and 3 had surgery concurrent with the axilla. Five patients had partial dehiscence and serosanguinous discharge, followed by complete scar formation by second intention healing.
CONCLUSION: Surgery is often the most appropriate and definitive treatment for HS. The lateral thoracic fasciocutaneous flap technique is associated with high success rates in this patient population.
Keywords: Hidradenitis suppurativa; Surgical flaps; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A hidradenite supurativa (HS) é uma infecção bacteriana crônica, multifatorial e frequentemente recorrente na pele e nos tecidos subcutâneos. No entanto, a resolução completa pode ser conseguida por meio de cirurgia. É descrita uma série de pacientes com complicações de HS, sua evolução, as complicações após a ressecção cirúrgica completa axilar e a rotação de retalho fasciocutâneo torácico lateral, além da análise das áreas acometidas associadas.
MÉTODOS: Entre 2009 e 2014, seis pacientes com idade entre 25,5 anos em média (intervalo: 15-35) foram submetidos à cirurgia para HS. Todos os pacientes apresentaram lesões de longa data axilares crônicas refratárias ao tratamento clínico.
RESULTADOS: Seis pacientes com HS (dois homens e quatro mulheres) foram submetidos à cirurgia. O período de acompanhamento foi de 16 meses, em média (intervalo: 4 meses - 5 anos). A resolução completa foi alcançada e nenhuma recorrência foi observada. A ressecção foi bilateral em quatro casos e unilateral em dois. Cinco pacientes apresentaram lesão inguinal, das quais três foram operadas no mesmo tempo cirúrgico. Cinco pacientes apresentaram deiscência parcial e descarga serossanguinolenta, seguida de cura completa após cicatrização por segunda intenção.
CONCLUSÃO: A cirurgia é frequentemente o tratamento definitivo mais adequado para a HS. A técnica de retalho fasciocutâneo torácico lateral está associada a altas taxas de sucesso nesta população de doentes.
Palavras-chave: Hidradenite supurativa; Retalhos cirúrgicos; Procedimentos cirúrgicos reconstrutivos.
Hidradenitis suppurativa (HS) is a chronic bacterial infection of the skin and subcutaneous tissue that affects the apocrine glands, and is often difficult to treat and recurrent1-4.
HS was described in 1864 by Verneuil, who associated its occurrence with the infection of sweat glands. In 1922, Shiefferdecker observed that this disease was specifically related to the apocrine glands, and named the pathology as HS3-6.
The etiology is not fully understood1,2, although its occurrence is related to diabetes, smoking, obesity, and immunosuppression. HS starts with obstruction of the hair follicle sheath and is caused by a keratin plug that subsequently leads to infection. The axillary, inguinal, gluteal, mammary, inframammary, umbilical, perianal, perineal, pubic, thoracic, scalp, retroauricular, and eyelid regions are affected, as they are associated with a large number of these glands1,4,7,8.
Non-surgical treatment should initially be attempted, while surgery is indicated for recurrent cases that do not respond to a conservative approach. Non-surgical treatment is based on the use of topical and/or systemic drugs, such as antibiotic therapy and corticosteroids. The lack of specific tests hinders the early diagnosis and subsequent treatment.
Surgical intervention may be the only option for cure, and the approaches vary from acute abscess drainage to local excision or extensive removal of all affected tissue3,9. The surgical technique considered most appropriate takes into account the need to open all sinus tracts. Experience has shown that a better outcome is obtained with wide-excision surgery, which results in lower recurrence rates3,4,9,10.
OBJECTIVES
This report describes a series of HS cases that were treated by performing surgical resection of the affected axillary area, with subsequent coverage using a local fasciocutaneous flap. The indications, evolution, postoperative complications, and concurrent treatment of associated lesions were evaluated.
METHODS
From 2009 to 2014, 6 HS patients (2 males and 4 females) underwent surgery. The procedures were performed at a public hospital in Fortaleza, CE, by the same surgeon. Patients who responded to non-surgical treatment were excluded. The study was conducted according to the principles of the Declaration of Helsinki. The age of the patients ranged from 15 to 35 years and the average age was 25.5 years.
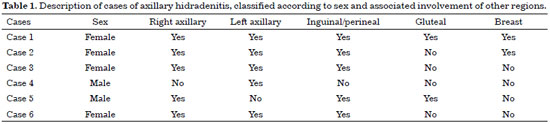
All patients had long-standing, chronic axillary lesions that were refractory to non-surgical treatment (Figure 1). In 2 cases, the lesions affected only one axilla. In 5 cases, there was associated inguinal involvement, but only 3 underwent resection concurrent with the axilla. In 2 cases, there was associated gluteal involvement. Breast and sternal lesions were present in 2 cases (Table 1). These were painful, cystic and pustular lesions, causing great psychological and social distress due to their strong smell, and adversely affected the patient's social life. In both cases, the patients were smokers.

Figure 1. Long-standing, chronic axillary hidradenitis suppurativa, refractory to non-surgical treatment and presenting with cutaneous fistulas, fibrosis, and active lesions.
In all cases, the proposed treatment was based on the concurrent surgical management of all affected areas, with lateral thoracic fasciocutaneous flap rotation in the axilla and primary closure in the inguinal, gluteal, and mammary region.
The fasciocutaneous flap prepared for the axillary region was designed according to the size of the resected area. An incision was performed on the skin, crossing the demarcated border, and was carried down to the fascia. The flap was prepared, rotated to cover the defect, and sutured on the edges in the deepest region, in order to reduce the dead space of the defect below the flap. Continuous suction drains were placed.
In 4 female cases, anterior lateral thoracic fasciocutaneous flap rotation with complete closure of the lesions was performed, to avoid deforming the breast region (Figure 2). In males (2 cases), a posterior lateral thoracic fasciocutaneous flap was used (Figure 3).

Figure 2. Design of the anterior lateral thoracic fasciocutaneous flap for coverage of the resected axillary region.

Figure 3. Design of the posterior lateral thoracic fasciocutaneous flap for coverage of the resected axillary region.
RESULTS
Six patients (2 males and 4 females) underwent surgery between 2009 and 2014. Complete resolution was observed in all cases, without any relapse in the treated area. The patients were followed up for a period ranging from 4 months to 5 years, on average 16 months.
Bilateral axillary resection was performed in 4 cases. In 2 cases, the lesion affected only one axilla. In 5 cases, there was associated inguinal involvement, but only 3 underwent resection concurrent with the axilla. In 2 cases, there was associated gluteal involvement. Concurrent breast and sternal lesions were present in 2 cases (Table 1). Two patients were smokers. One case underwent resection with a unilateral flap, while only resection of small lesions with primary suturing was performed on the opposite side. There was no limitation on arm abduction in any of the cases.
DISCUSSION
HS affects the sweat glands and is characterized by a recurrent inflammatory and infectious process. It can affect several regions, including the axillary, inguinal, perineal, and gluteal areas. In addition, it may be associated with smoking2,4,7. More recent studies suggest that HS can be replaced by the term acne inversa, justifying this change with the notion that hidradenitis is not an inflammation of the apocrine sweat glands, but an occlusion of the hair follicles, as in acne vulgaris11.
Surgical treatment for HS has long been performed, and has been shown to be effective when used appropriately, despite significant recurrence rates, especially with larger lesions. The first surgically treated cases date back to the late 1950s, and reviews of these procedures have been described since then9.
The most appropriate technique depends on the extent and location of the lesions, and always takes into account the complete resection of all affected areas, with sufficient safety margin and depth to reach healthy tissues and remove all areas of hair growth to avoid recurrence.
In the simplest cases, resection is limited to small areas, with few sequelae. However, in advanced cases, with cysts, long-standing recurrent infection, scars, and tunneled areas, wide resection should be performed; however, this does not allow primary closure. All cases presented herein had advanced disease. This may be due to neglect or difficulty accessing the public health system, thus enabling the disease to evolve.
In cases in which the removal of the entire affected area creates large defects, skin grafts are widely used. These are commonly and successfully employed to reconstruct large affected areas. However, there may be areas of retraction that limit arm elevation, in addition to providing very thin coverage4,9,10,12-15.
A flap is a widely used and appropriate alternative in most cases. These are basic procedures, employed to correct loss of dermal substance due to lesion resection. In addition, they provide a satisfactory functional result3,9,10,13.
The most appropriate procedure is defined according to the region affected by the disease. In axillary lesions, the reconstruction is complex and must take into account the type of skin, shape, and contour5,6,9,15,16. Local V-Y advancement fasciocutaneous flaps have long been used for the closure of large surgical wounds that result from extensive resection for HS.
In axillary lesions, an alternative is the doubleopposing V-Y flap. In cases of recurrence, the use of lateral thoracic island, fasciocutaneous flaps has been reported to provide satisfactory outcomes6,8,9,13,15-17. This is considered to be a good option in females, due to the proximity of the lesion and scar to the lateral contour of the breast, thus suggesting that moving too much breast tissue is not necessary16,18. In men, the thoracodorsal fasciocutaneous flap was chosen because of the small anterior lateral thoracic donor area and the possibility of moving the nipple-areolar complex3,19.
Although musculocutaneous flaps are widely used in reconstructive surgeries and have recognized advantages, such as good vascularization and thickness, they present some disadvantages when compared to cutaneous flaps, since the latter preserve the muscles. In addition, functional deficits and postoperative pain are reduced2.
Planning the reconstruction of the affected areas is critical for the success of surgical treatment. The most suitable method should be chosen by taking into account factors such as the location and size of lesions, and the incisions that will be necessary. These factors are significantly correlated with the length of hospital stay and the patient's recovery, which has a subsequent impact on treatment costs9,10,13.
Resection of the associated inguinal region was performed in the first 3 cases. However, a longer and more painful postoperative period was observed. In the 2 subsequent cases, the recovery was faster, with fewer complaints by the patients.
HS treatment is complex and difficult. However, despite the lack of clinical response in some cases, the surgical approach can provide complete resolution of chronic infectious and inflammatory conditions. The local fasciocutaneous flap proved to be very efficient in axillary reconstruction, since it did not cause any loss of substance or functional sequelae.
COLLABORATIONS
VVSJ Analyzed and/or interpreted the data; performed statistical analyses; approved the final version of the manuscript; developed and designed the study; performed surgeries and/ or experiments; wrote the manuscript and/or critically reviewed its content.
NGSO Approved the final version of the manuscript; developed and designed the study; performed surgeries and/or experiments.
FRSS Analyzed and/or interpreted the data; wrote the manuscript and/or critically reviewed its content.
REFERENCES
1. Schmitt JV, Bombonatto G, Martin M, Miot HA. Risk factors for hidradenitis suppurativa: a pilot study. An Bras Dermatol. 2012;87(6):936-8.
2. Andrade MMA, Constantino JRM, Gomes DMBM, Faria FF, Oliveira RG, Ferreira RMRS, et al. Hidradenitis suppurativa: literature review and case report. J Coloproctol (Rio J.). 2012;32(2):196-201.
3. Teixeira JCEO, Ribeiro Filho AS, Castro OC. Thoracodorsal fascioc utaneous flap in the treatment of hidradenitis suppurativa: a case report and literature review. Rev Bras Cir Plást. 2012;27(1):170-3.
4. Charúa-Guindic L, Maldonado-Barrón R, Avendaño-Espinosa O, Navarrete-Cruces T, Osorio-Hernández RM, Jiménez-Bobadilla B. Hidradenitis suppurativa. Cir Cir. 2005;74(4):249-55.
5. Rehman N, Kannan RY, Hassan S, Hart NB. Thoracodorsal artery perforator (TAP) type I V-Y advancement flap in axillary hidradenitis suppurativa. Br J Plast Surg. 2005;58(4):441-4.
6. Geh JL, Niranjan NS. Perforator-based fasciocutaneous island flaps for the reconstruction of axillary defects following excision of hidradenitis suppurativa. Br J Plast Surg. 2002;55(2):124-8.
7. Fernandes NC, Franco CP, Lima CM. Hidradenitis suppurativa: retrospective study of 20 cases. An Bras Dermatol. 2013;88(3):480-1.
8. Soldin MG, Tulley P, Kaplan H, Hudson DA, Grobbelaar AO. Chronic axillary hidradenitis-the efficacy of wide excision and flap coverage. Br J Plast Surg. 2000;53(5):434-6.
9. Alharbi Z, Kauczok J, Pallua N. A review of wide surgical excision of hidradenitis suppurativa. BMC Dermatol. 2012;12:9.
10. Ellis LZ. Hidradenitis suppurativa: surgical and other management techniques. Dermatol Surg. 2012;38(4):517-36.
11. Sellheyer K, Krahl D. "Hidradenitis suppurativa" is acne inversa! An appeal to (finally) abandon a misnomer. Int J Dermatol. 2005;44(7):535-40.
12. Wiseman MC. Hidradenitis suppurativa: a review. Dermatol Ther. 2004;17(1):50-4.
13. Lirón-Ruiz R, Torralba-Martinez JA, Pellicer-Franco E, Morales-Cuenca G, Martín-Lorenzo JG, Miguel-Perelló J, et al. Treatment of long-standing extensive perianal hidradenitis suppurativa using double rotation plasty, V-Y plasty and free grafts. Int J Colorectal Dis. 2004;19(1):73-8.
14. van Rappard DC, Mooij JE, Mekkes JR. Mild to moderate hidradenitis suppurativa treated with local excision and primary closure. J Eur Acad Dermatol Venereol. 2012;26(7):898-902.
15. Hynes PJ, Earley MJ, Lawlor D. Split-thickness skin grafts and negative-pressure dressings in the treatment of axillary hidradenitis suppurativa. Br J Plast Surg. 2002;55(6):507-9.
16. Schwabegger AH, Herczeg E, Piza H. The lateral thoracic fasciocutaneous island flap for treatment of recurrent hidradenitis axillaris suppurativa and other axillary skin defects. Br J Plast Surg. 2000;53(8):676-8.
17. Busnardo FF, Coltro PS, Olivan MV, Busnardo AP, Ferreira MC. The thoracodorsal artery perforator flap in the treatment of axillary hidradenitis suppurativa: effect on preservation of arm abduction Plast Reconstr Surg. 2011;128(4):949-53.
18. Mello DF, Helene Junior A. Retalho fasciocutâneo torácico lateral para reconstrução de defeitos axilares após ressecção de hidradenite supurativa: série de 10 casos. Rev Bras Cir Plást. 2016;31(2):186-91.
19. Menderes A, Sunay O, Vayvada H, Yilmaz M. Surgical management of hidradenitis suppurativa. Int J Med Sci. 2010;7(4):240-7.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Geral Dr. César Cals, Fortaleza, CE, Brazil
3. Universidade de Fortaleza, Fortaleza, CE, Brazil
Institution: Hospital Geral Dr. César Cals, Fortaleza, Ceará, Brazil.
Corresponding author:
Valderi Vieira da Silva Júnior
Rua Barão de Aracati, 1304 - Aldeota
Fortaleza, CE, Brazil Zip Code 60115-081
E-mail: valderijr@hotmail.com
Article received: July 10, 2015.
Article accepted: October 30, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter