

Original Article - Year 2016 - Volume 31 -
Evaluation of cases of mammoplasty with the areolar inferior pedicle technique
Avaliação dos casos de mamoplastia pela técnica do pedículo inferior areolado
ABSTRACT
INTRODUCTION: Mammoplasty is one of the most common plastic surgeries in Brazil. Among the surgical techniques described in the literature, the areolar inferior pedicle technique is the most significant because of its versatility, safety, and satisfactory aesthetic results. This study avaluated cases of mammoplasty with the areolar inferior pedicle technique performed by the author, and to propose a small change in the attachment of the pedicle to the pectoralis major muscle.
METHODS: A total of 74 patients underwent the surgery from June 2007 to December 2014.
RESULTS: The average patient age was 35.63 years; the mean body mass index was 25.8; and the mean follow-up duration was 28 months. Complications occurred in 33.76% of the cases, and the average amount of resected tissue was 585 g. The degree of satisfaction was excellent or good in 93% of the cases. The sensitivity of the areolar-papillary complex (APC) was maintained in 72% of left-breast reconstructions and 77% of right-breast reconstructions. Moreover, there was a complete loss of sensitivity in 3% of left-breast cases.
CONCLUSION: The use of mammoplasty with the areolar inferior pedicle was versatile and safe, and produced favorable outcomes. In addition, the sensitivity of the APC was adequately maintained. Further studies might confirm the importance of the change in fixation of the pedicle suggested in this study.
Keywords: Mammoplasty; Plastic surgery; Breast; Cosmetic techniques; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A mamoplastia é uma das cirurgias plásticas mais realizadas no Brasil. Dentro do universo de técnicas descritas, destaca-se o pedículo inferior areolado por sua versatilidade, segurança e bons resultados estéticos. O estudo avalia os casos de mamoplastia pela técnica do pedículo inferior areolado realizados pelo autor e apresentar uma pequena modificação na forma de fixação do pedículo ao músculo peitoral maior.
MÉTODOS: Foram avaliadas 74 pacientes operadas no período de junho de 2007 a dezembro de 2014.
RESULTADOS: A idade média das pacientes foi de 35,63 anos, o índice de massa corporal médio foi 25,8 e o tempo médio de seguimento, de 28 meses. Complicações ocorreram em 33,76% dos casos, a quantidade média de tecido ressecado foi 585 gramas. O grau de satisfação foi ótimo ou bom em 93% dos casos. Houve manutenção da sensibilidade do complexo areolopapilar (CAP) em 72% das mamas à esquerda e 77% à direita. Em 3% das mamas à esquerda houve perda completa da sensibilidade.
CONCLUSÃO: A mamoplastia pelo pedículo areolado inferior mostrou-se neste estudo versátil, segura e com bons resultados. Além disso, houve boa manutenção da sensibilidade do CAP. Estudos posteriores poderão ratificar a importância da modificação na fixação do pedículo sugerida neste trabalho.
Palavras-chave: Mamoplastia; Cirurgia plástica; Mama; Técnicas cosméticas; Procedimentos cirúrgicos reconstrutivos.
Excess breast tissue is usually associated with physical and psychological discomfort. In addition to the complaints of back pain, neck pain, and dermatitis, patients with macromastia present limitations in physical activity and experience major social impairments because of the excessive breast volume1. Previous studies have reported that bilateral reduction mammoplasty is highly effective in relieving these symptoms2.
Reduction mammoplasty is one of the most common plastic surgery procedures. The choice of the best technique, which combines safety and satisfactory aesthetic and functional results, represents a challenge for plastic surgeons3.
Reduction mammoplasty with the inferior pedicle, including the areolar-papillary complex (APC), continues to be widely employed in North America; however, it is rarely performed in Brazil1,4.
Several studies have demonstrated the safety of this technique, as well as the reproducibility of results, absence of major complications (even in larger resections), preservation of the sensitivity of the APC, and the possibility of use in cases of severe ptosis and breast amputation with free graft of the areola5,6.
Plastic surgeons endeavor to achieve the best aesthetic results through the combination of several parameters, including shape and volume readjustments, stability, reproducible results, and low complication rates. Among the available surgical techniques and strategies, each surgeon will have a preference for a particular technique and may sometimes make modifications to obtain optimal results.
OBJECTIVES
This study aimed to analyze cases of mammoplasty with the areolar inferior pedicle technique performed by the author, and to propose a change in the method of attachment of the pedicle to the pectoralis major muscle.
METHODS
This retrospective study evaluated cases of mammoplasty conducted by using the areolar inferior pedicle technique between June 2007 and December 2014 in Criciúma, state of Santa Catarina, Brazil. Cases of mammoplasty performed with other techniques, secondary surgeries, and cases with missing data were excluded from the study.
Data were collected by reviewing medical records, surgical descriptions, photographic records, and telephone contacts. The variables evaluated were patients' age, body weight, body mass index, comorbidities, smoking, complication rate, need for reintervention, degree of sensitivity of the APC, and aesthetic satisfaction. This study complied with the principles of the Declaration of Helsinki.
The degree of sensitivity of the APC was evaluated subjectively by patients and classified into the following categories: unchanged, minor decrease, major decrease, or complete loss of sensitivity. The degree of aesthetic satisfaction was evaluated subjectively and classified into the following categories: excellent, good, fair, and poor.
In the preoperative period, all patients were subjected to laboratory tests, electrocardiography, chest radiography, and mammography and ultrasound of the breasts, as well as preanesthetic consultation. All patients signed an informed consent form.
The surgeries were performed at the hospital, and the resected material was sent to the pathology laboratory. The patients used surgical bras for 60 days.
Marking
With the patient standing, the following reference points were demarcated: furculum, chest midline, inframammary crease, and breast meridians. Point A corresponds to the projection above the areola at the midpoint of the inframammary crease; the arms of flaps AB and AC make a 90º angle to each other, extending to a distance of 9-10 cm, according to the evaluation conducted with bi-digital clamping. The pedicle was demarcated with a base of 8 cm.
Surgical technique
The surgeries were performed under general anesthesia, and the breasts were infiltrated with a saline solution containing adrenaline at a dilution of 1:250,000. The preoperative markings were incised, and the areolas were demarcated with a 4.5-cm areolotome. The pedicle was de-epithelized and excess breast tissue was resected, preserving the fascia of the pectoral muscle, which is an important area for pedicle clamping.
Modified fixation of the pedicle
The body of the pedicle was fixated with simple stitches by using nylon 2-0 zigzag sutures instead of the classical fixation with symmetrical stitches, to prevent the strap effect and impairment of APC vascularization (Figures 1 and 2). In the upper portion, two attachment points were used for better stabilization, with care not to limit the lift of the APC (Figures 3 and 4).
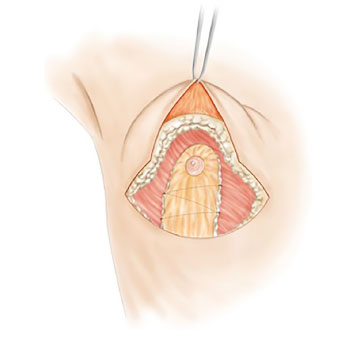
Figure 1. Fixation of the pedicle in zigzag form.
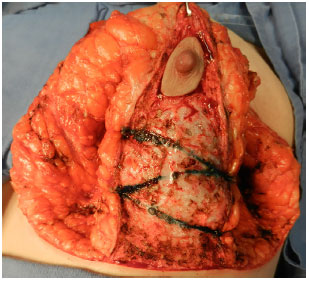
Figure 2. Intraoperative image of the fixation of the pedicle in zigzag form.
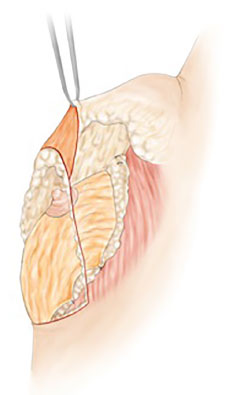
Figure 3. Superior fixation points.
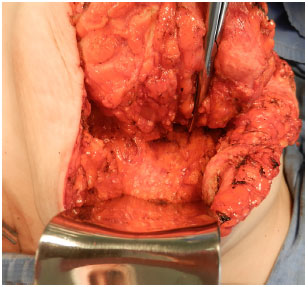
Figure 4. Intraoperative image of the superior fixation of the pedicle.
The breast was sutured in two layers (subdermal and intradermal) with Monocryl 4-0 absorbable suture. A suction drain was used for 3-4 days.
Liposuction was conducted in the lateral regions of the breast for aesthetic refinement when indicated.
RESULTS
Between June 2007 and December 2014, 96 surgeries were conducted with the areolar inferior pedicle technique (Figures 5 and 6). A total of 22 patients were excluded from the study because of failure of follow-up or loss of telephone contact. The follow-up period ranged from 6 to 90 months, with an average of 28 months. The patients' age ranged between 15 and 78 years, with an average of 35.67 years. The average body mass index was 25.8. The amount of resected tissue ranged between 60 and 2800 g, with an average of 585 g. There were no malignant findings in the samples sent for pathology.
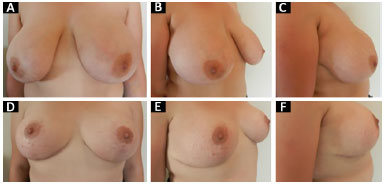
Figure 5. Mammoplasty with the areolar inferior pedicle technique. A, B and C: Before surgery; D, E and F: 6 months after surgery.
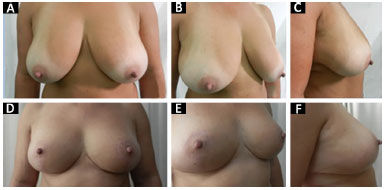
Figure 6. Mammoplasty with the areolar inferior pedicle technique. A, B and C: Before surgery; D, E and F: 1 year after surgery.
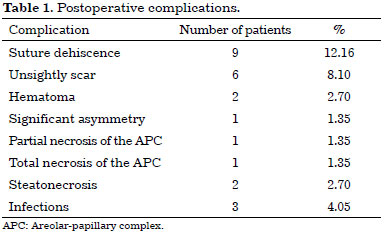
Complications occurred in 25 (33.76%) patients, and the most frequent cases were scar dehiscence, which occurred primarily at the junction between the vertical and the horizontal scar. Major reoperations were required in three cases: two for removal of nodules (steatonecrosis) at the end of the pedicle and one case for correction of significant asymmetry. Minor corrections were performed in 12 patients under local anesthesia. Three cases of infections occurred in wounds and were treated with oral antibiotics. No systemic complications were observed (Table 1).
With regard to the degree of satisfaction with the surgery, the percentage of patients that considered the results optimal, good, regular, and poor was 81%, 12%, 6%, and 1%, respectively (Figure 7).
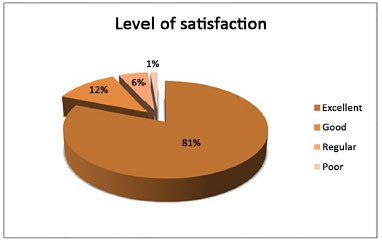
Figure 7. Evaluation of patient satisfaction.
The sensitivity of the APC was evaluated separately in the right and left breasts. Total loss of sensitivity was observed in 3% of left-breast reconstructions (Figure 8) and in none of the rightbreast reconstructions (Figure 9).
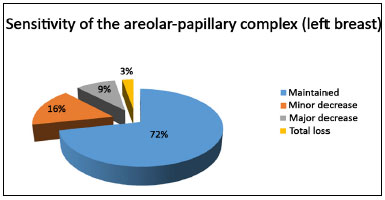
Figure 8. Sensitivity of the areolar-papillary complex (left breast).
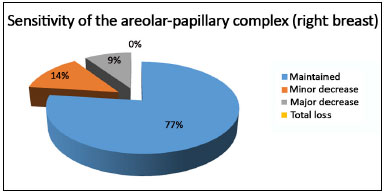
Figure 9. Sensitivity of the areolar-papillary complex (right breast).
Seven percent of the patients were smokers at the time of surgery.
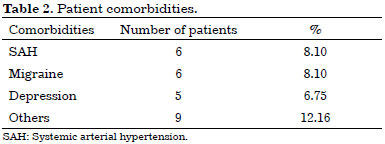
Comorbidities were found in 26 (35.11%) patients, with the most common complications being hypertension (8.1%), migraine (8.1%), and depression (6.75%) (Table 2).
DISCUSSION
The goal of the plastic surgeons in mammoplasty is to achieve optimal aesthetic results with lower complication rates. Several techniques have been described in the literature, and it is the responsibility of surgeons to master most of those techniques in order to increase their skills and better face daily challenges in the clinic.
The areolar inferior pedicle technique was first described by Ribeiro and Backer 1977. In 2002, they reported their experience with this technique in 2000 patients during a period of 30 years and described five types of flaps6-9.
This technique is easily reproducible, does not significantly increase the duration of surgery, can be used in breasts of varying shapes and sizes, has a low complication rate, maintains nipple sensitivity and erection, and has an adequate level of patient satisfaction10-12.
Rohrich, in 2004, found that this was the most commonly used technique by 44.1% of the surgeons who participated in their study in the United States1.
In mammoplasty executed by using the inferior pedicle, complications occurred in 22.1% to 59.0% of cases, depending on the criteria of each study13,14. In our study, the complication rate was 33.78%, and the most frequent cases were minor complications, including scar dehiscence and unsightly scars, concurring with the results reported in previous studies3,13.
Necrosis of the APC occurred in two cases (2.7%): one involving partial necrosis and one involving total necrosis. The incidence of total necrosis of the APC is low in cases in which the areolar inferior pedicle technique was used5,13,15. There were two cases of steatonecrosis at the distal portion of the pedicle because the base of the pedicle was too narrow; however, there was no APC impairment. None of the study patients with necrosis of the APC or steatonecrosis were smokers.
The loss of sensitivity of the APC is a cause for concern for surgeons and patients. In this respect, the techniques that use the superior pedicle, with the need for tissue resection of the base of the breast, have higher rates of permanent reduction in the sensitivity of the APC16.
Several studies have shown that the use of the inferior pedicle results in rapid recovery of the sensitivity of the APC, and this recovery can reach the preoperative levels16,17. In our study, the sensitivity of the APC was unchanged in 72% of left-breast reconstructions and in 77% of right-breast reconstructions. There was a complete loss of sensitivity in 3% of left-breast cases, whereas no such loss was observed in right-breast cases.
With regard to the satisfaction with the outcomes, the level was excellent or good in 93% of the cases. The techniques that use the inferior pedicle evolve with a significant increase in the vertical component of the scar18-20.
We made a small change in the technique for pedicle fixation to decrease excessive ptosis. In addition to making the attachment in zigzag form, as described above, we attached the distal part of the pedicle with two sutures, one medial and one lateral, with care to prevent excessive fixation of the pedicle and avoid difficulties in opening the APC and flattening of the breast. We noted that long-term results were obtained by stabilizing the pedicle with this fixation procedure and that the position of the APC was maintained (in the apex of the breast cone).
CONCLUSION
Mammoplasty by using the areolar inferior pedicle was safe, achieved satisfactory cosmetic results, and preserved the sensitivity of the APC. Further studies might confirm the importance of the change in fixation of the pedicle suggested in this study.
COLLABORATIONS
EF Aprovação final do manuscrito; concepção e desenho do estudo; realização das operações e/ou experimentos; redação do manuscrito ou revisão crítica de seu conteúdo.
GJSA Realização das operações e/ou experimentos.
IAYK Análise e/ou interpretação dos dados; análise estatística; redação do manuscrito ou revisão crítica de seu conteúdo.
FYK Redação do manuscrito ou revisão crítica de seu conteúdo.
REFERENCES
1. Rohrich RJ, Gosman AA, Brown SA, Tonadapu P, Foster B. Current preferences for breast reduction techniques: a survey of board-certified plastic surgeons 2002. Plast Reconstr Surg. 2004;114(7):1724-33.
2. Georgiade GS, Riefkohl RE, Georgiade NG. The inferior dermalpyramidal type breast reduction: long-term evaluation. Ann Plast Surg. 1989;23(3):203-11.
3. Cammarota MC, Camara Filho JPP, Daher JC, Benedik Neto A, Faria CADC, Borgatto MS, et al. Aplicação estética e reconstrutora da mamoplastia com pedículo areolado. Rev Bras Cir Plást. 2014;29(2):237-42.
4. Adorno Filho ET, Almeida KG, Arruda AM, Kracik AS, Oliveira GSM, Costa GR, et al. Breast reduction with the lower pedicle technique: an observational study. Rev Bras Cir Plást. 2014;29(4):525-30.
5. Gerzenshtein J, Oswald T, McCluskey P, Caplan J, Angel MF. Avoiding free nipple grafting with the inferior pedicle technique. Ann Plast Surg. 2005;55(3):245-9.
6. Lacerna M, Spears J, Mitra A, Medina C, McCampbell E, Kiran R, et al. Avoiding free nipple grafts during reduction mammaplasty in patients with gigantomastia. Ann Plast Surg. 2005;55(1):21-4.
7. Ribeiro L, Backer E. Mastoplastia com pedículo de seguridad. Rev Esp Cir Plast. 1973;16:223-34.
8. Jurado J. Plásticas mamárias de redução baseadas em retalho dérmico vertical monopediculado. In: Anais XII - Congresso Brasileiro de Cirurgia Plástica; 1976. p. 29.
9. Ribeiro L, Accorsi A Jr, Buss A, Marcal-Pessoa M. Creation and evolution of 30 years of the inferior pedicle in reduction mammaplasties. Plast Reconstr Surg. 2002;110(3):960-70.
10. Scott GR, Carson CL, Borah GL. Maximizing outcomes in breast reduction surgery: a review of 518 consecutive patients. Plast Reconstr Surg. 2005;116(6):1633-9.
11. Bezerra FJF, Moura RMG, Silva Júnior VV. Mamoplastia redutora e simetrização de mama aposta em reconstrução mamária utilizando a técnica de pedículo inferior. Rev Bras Cir Plást. 2007;22(1):52-9.
12. Ribeiro L. Pedículos em mamoplastia: atlas e texto. Rio de Janeiro: Guanabara Koogan; 2005.
13. Zambacos GJ, Mandrekas AD. Complication rates in inferior pedicle reduction mammoplasty. Plast Reconstr Surg. 2006;118(1):274-5.
14. Thorek M. Possibilities in the reconstruction of the human form. N Y Med J. 1922;116:572.
15. O'Grady KF, Thoma A, Dal Cin A. A Comparison of complication rates in large and small inferior pedicle reduction mammaplasty. Plast Reconstr Surg. 2005;115(3):736-42.
16. Schlenz I, Rigel S, Schemper M, Kuzbari R. Alteration of nipple and areola sensitivity by reduction mammaplasty: a prospective comparison of five techniques. Plast Reconstr Surg. 2005;115(3):743-51.
17. Mofid MM, Dellon AL, Elias JJ, Nahabedian MY. Quantitation of breast sensibility following reduction mammaplasty: a comparison of inferior and medial pedicle techniques. Plast Reconstr Surg. 2002;109(7):2283-8.
18. Boechat HRBL, Rodrigues FHOC, Miranda ES, Castro VM, Souza VEM, Leão CEG. Evolução da posição do complexo aréolomamilar e da extensão das cicatrizes após mamoplastia redutora com retalho de pedículo inferior areolado. Rev Bras Cir Plást. 2008;23(3):167-72.
19. André FS, Chocial AC. Tratamento das gigantomastias. Rev Bras Cir Plást. 2010;25(4):657-62.
20. Strombeck JO. Macromastia in women and its surgical treatment. A clinical study based on 1,042 cases. Acta Chir Scand Suppl. 1964;341:Suppl 341:1.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Universidade do Extremo Sul Catarinense, Criciúma, SC, Brazil
3. Clínica Belvivere de Cirurgia Plástica e Laser, Criciúma, SC, Brazil
Institution: Clínica Belvivere de Cirurgia Plástica e Laser, Criciúma, SC, Brazil.
Corresponding author:
Eduardo Favarin
Rua Coronel Pedro Benedet, 505, Salas 10/11 - Centro
Criciúma, SC, Brazil Zip Code 88801-250
E-mail: efavarin@yahoo.com.br
Article received: July 28, 2015.
Article accepted: September 29, 2015.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter