

Original Article - Year 2016 - Volume 31 -
Lower eyelid and malar/palpebral groove reconstructions with a V-Y skin flap after skin tumor removal
Reconstrução de pálpebra inferior e junção malar/palpebral com retalho cutâneo em V-Y após ressecção de tumores de pele
ABSTRACT
INTRODUCTION: The most commonly used flaps for the reconstruction of the lower eyelid and malar/palpebral groove are cervicofacial flaps owing to their horizontal traction, which results in a lower risk of ectropion and canthal dystopias. V-Y skin flap is not often used for the fear of the vertical traction being transferred to the lower eyelid, which would lead to the occurrence of ectropion and dystopias. Our aim is to demonstrate that, if well executed, this flap may be a good option for reconstructions of this region.
METHODS: Sixty-eight eyelid reconstructions have been performed at the ACCamargo Cancer Center between December 2012 and May 2015. Of these, 29 patients underwent reconstruction of the lower eyelid or malar/palpebral groove using a V-Y skin flap after skin tumor removal.
RESULTS: Among the palpebral reconstructions, the most commonly used was the V-Y flap (29 cases, 42.6%). Two cases (6.9%) developed ectropion. No case of seroma, hematoma, infection, or partial loss of the flap has been observed.
CONCLUSION: The V-Y flap is a good option for eyelid reconstruction when well indicated, designed, and executed, since it presents low complication rates and the possibility to be performed under local anesthesia. Therefore, this flap is a good choice for patients without the clinical conditions necessary to undergo surgery under general anesthesia.
Keywords: Eyelids; Reconstructive surgical procedures; Skin neoplasms; Ectropion.
RESUMO
INTRODUÇÃO: Os retalhos mais comumente utilizados para reconstruções de pálpebra inferior e junção malar/palpebral são os cervicofaciais, pois a sua tração horizontal levaria a menor risco de ectrópio e distopias cantais. O retalho cutâneo em V-Y frequentemente não é utilizado pelo receio de que a tração vertical seja transferida à pálpebra inferior, gerando ectrópio e distopias. Nosso objetivo é demonstrar que, se bem executado, este retalho pode ser uma boa opção para reconstruções nesta região.
MÉTODOS: Foram realizadas 68 reconstruções palpebrais no ACCamargo Cancer Center, entre dezembro de 2012 e maio de 2015. Dentre estes pacientes, 29 foram submetidos à reconstrução de pálpebra inferior ou junção malar/palpebral, após ressecção de tumores cutâneos, com retalhos cutâneos em V-Y.
RESULTADOS: Dentre as reconstruções palpebrais, o retalho V-Y foi o mais utilizado (29 casos, 42,6%). Dois casos (6,9%) evoluíram com ectrópio. Não houve nenhum caso de seroma, hematoma, infecção ou perda parcial do retalho.
CONCLUSÃO: O retalho V-Y é uma boa opção para reconstruções palpebrais quando bem indicado, desenhado e executado, pois apresenta baixos índices de complicações e também por poder ser realizado sob anestesia local, sendo uma boa escolha para pacientes sem condições clínicas de serem submetidos à anestesia geral.
Palavras-chave: Pálpebras; Procedimentos cirúrgicos reconstrutivos; Neoplasias cutâneas; Ectrópio.
Reconstruction with V-Y skin flaps can be performed in several areas of the face. When this technique is employed to reconstruct the lower eyelid and malar/palpebral groove, the risk of developing ectropion and dystopias of the canthal region makes it particularly challenging1.
Cervicofacial flaps of horizontal tractions (Mustardé) are the most commonly used flaps in the reconstruction of the lower eyelid region, since their horizontal traction reduces the risk of ectropion2. The V-Y flap is not often used in the reconstruction of these regions owing to the fear of the vertical traction being transmitted to the palpebral margin, thus leading to the development of ectropion and dystopias2.
OBJECTIVE
The aim of this study is to demonstrate that, when well indicated and performed, the V-Y skin flap is a good option to reconstruct the lower eyelid and malar/palpebral groove. This is because of the fact that it presents low rates of postoperative complications and the possibility to be performed under local anesthesia in patients with advanced age and without the clinical conditions necessary to undergo surgery under general anesthesia.
METHODS
A retrospective study was carried out by the author (M.C.), analyzing 68 patients undergoing immediate eyelid reconstruction after skin tumor removal between December 2012 and May 2015 at the ACCamargo Cancer Center, in São Paulo, SP. A particular emphasis was given to those patients submitted to a reconstructive procedure with V-Y skin flaps.
All patients submitted to eyelid reconstructions with V-Y skin flaps used for the lower eyelid and malar/ palpebral groove were analyzed within the period indicated. In total, 29 cases have been evaluated (no patient was excluded).
The reconstructions were performed after complete removal of the tumors and tumor-free margins (in all cases, an intraoperative anatomopathological examination was performed by freezing the specimen, except for the case of melanoma, in which the surgical margins were extended, according to the Breslow's thickness and standardizations of the National Comprehensive Cancer Network - NCCN)3.
The information of the patients, such as type of tumor, location, complications, and need for surgical correction among others have been obtained from the medical records.
Ectropion was defined as the appearance of eyelid eversion, loss of contact between the bulbar and eyelid conjunctiva, or a difference >1 mm between the operated and contralateral eyelid persisting 6 months after surgery. Symptoms, such as xerophthalmia, epiphora, and foreign body sensation in the eye were also taken into account to establish the diagnosis and conduct.
Surgical Technique
The "V" shape was made for the medial incision being parallel or in the nasogenian sulcus. This would ensure the width and length of the upper flap to be equal to the dimensions of the surgical defect. The flap was incised into the subcutaneous tissue (SCT), and its upper and lower portions were detached to make it thin in these regions.
In the pedicle site, divulsion was performed with curved hemostatic surgical instruments at an angle of inclination of 30º between the flap and the skin plane, thus extending its base to the SCT. After a satisfactory advancement of the flap, the donor area was closed, forming a "Y" shape, and the sutures were carried out in an "in step" pattern, i.e., alternating the sides of the flap to suture the upper margin without any tension. These "in step" sutures were performed taking a lower region of the flap and an upper region of the malar or palpebral tissue and distributing the tension along the flap2 (Figure 1).
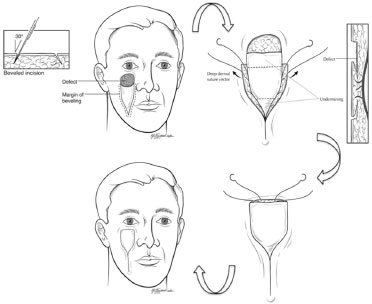
Source: Taken from Sugg et al.2
Figure 1. Design of the V-Y flap with the medial line in the right nasogenian sulcus. Divulsion in the region of the pedicle to 30º. detachment of the flap in its cranial and caudal portions, and points performed in an "in step" pattern.
When the medial incision exceeded the transition between the nasal wing and the malar region, transfixing sutures were carried out in full thickness using a 4-0 Nylon thread (transfixing sutures in the nasal mucosa) for the proper reconstruction of the nasal wing loop.
In some cases, one or more fixation points were carried out in the upper portion of the flap, anchored to the periosteum with a 4-0 PDS or 4-0 Mononylon thread. For the reconstruction of the inner corner of the eyes, anchoring sutures to the periosteum or canthal ligament were performed with a 3-0 Monocryl thread.
RESULTS
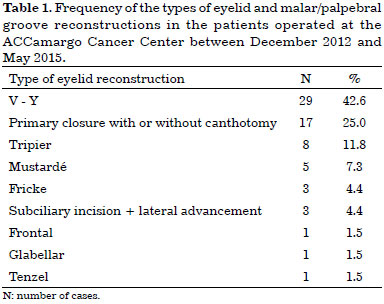
Sixty-eight reconstructions of the eyelid and malar/palpebral groove have been carried out between December 2012 and May 2015 at the ACCamargo Cancer Center. The V-Y flap was the flap most commonly used (29 cases, corresponding to 42.6%), followed by primary closure with or without canthotomy (17 cases, 25%) and Tripier flap (8 cases, 11.8%) (Table 1).
Among the cases that underwent reconstructions with the V-Y flap, 15 patients were women and 14 were men. The average age was 69.6 years (31 to 95 years). Regarding the primary lesions, 24 cases had basal cell carcinomas (82.8%), four had squamous cell carcinomas (13.8%), and one had melanoma (3.4%). In relation to the topography of the lesion, 22 and four cases had an affected inner corner of the eye (75.8%) and malar/palpebral groove region (13.8%), respectively; three cases presented extensive lesions, which involved the inner corner, lower eyelid, and malar region (10.4%).
No necrosis of the distal portion, hematoma, seroma formation, or infection was observed in all 29 cases reconstructed with the V-Y flap.
Two cases developed ectropion (6.9%) (Figures 2 and 3), which did not resolve six months after surgery (one medial and one lateral ectropion). Four cases (13.8%) underwent a new surgical correction of the flap under local anesthesia six months after surgery, which was aimed at an aesthetic improvement (Figures 2 to 7).

Figure 2. An 81-year-old patient submitted to a V-Y flap reconstruction upon the removal of an extended basal cell carcinoma. A: Generated defect and design of the flap presenting errors in width and length; B: IPO reconstruction; C: 6 months PO with medial ectropion (we opted to monitor the patient). PO: Postoperative; IPO: Immediate postoperative.

Figure 3. A 75-year-old patient submitted to a V-Y flap reconstruction upon the removal of an extended basal cell carcinoma. A: Generated defect and design of the flap; B: IPO reconstruction with transfixing points on the nasal mucosa and anchoring points from the flap to the periosteum; C: 6 months PO with lateral ectropion (we opted to correct it using a "tarsal strip"). PO: Postoperative; IPO: Immediate postoperative.

Figure 4. A 31-year-old patient submitted to a V-Y flap reconstruction upon the removal of a basal cell carcinoma. A: Generated defect and design of the flap; B: IPO reconstruction; C: 11 months PO. No requirement for surgical correction. PO: Postoperative; IPO: Immediate postoperative.
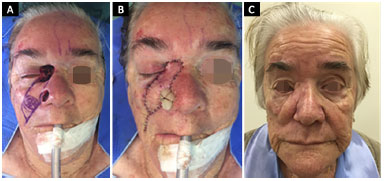
Figure 5. An 86-year-old patient submitted to a V-Y flap reconstruction upon the removal of a basal cell carcinoma. A: Generated defect and design of the flap; B: IPO reconstruction with transfixing points on the nasal mucosa; C: 4 months PO with mild apparent sclera and residual edema of the flap. PO: Postoperative; IPO: Immediate postoperative.

Figure 6. An 87-year-old patient submitted to a V-Y flap reconstruction upon the removal of a basal cell carcinoma under local anesthesia and sedation. A: Generated defect and design of the flap; B: IPO reconstruction with transfixing points on the nasal mucosa. IPO: Immediate postoperative.
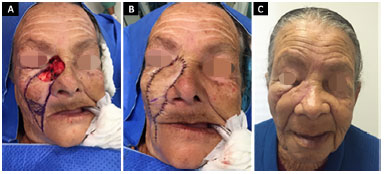
Figure 7. A 77-year-old patient submitted to a V-Y flap reconstruction upon the removal of an extended basal cell carcinoma. A: Generated defect and design of the flap; B: IPO reconstruction with anchoring points from the flap to the periosteum and transfixing points on the nasal mucosa; C: 1 month and 15 days PO showing edema, although in the absence of apparent sclera. PO: Postoperative; IPO: Immediate postoperative.
DISCUSSION
In the reconstructions of the lower eyelid and malar/palpebral groove, cervicofacial flaps (Mustardé) represent the first-choice procedure. This is because of their horizontal traction, which decreases the possibility of developing ectropion and canthal dystopia in the postoperative period1. The cervicofacial flap was firstly described by Esser in 19184 and then popularized by Mustardé in 19705. This flap minimizes the tension in the lower eyelid, recruiting tissue laterally to, but not below, the defect2. However, this type of flap requires an extensive detachment, which increases the risk of seroma and necrosis of the distal portion of the flap2,6.
The risk of developing a postoperative ectropion correlates to a pre-existing eyelid sagging, type of skin of the patient, position of the maxilla in relation to the orbit, size, and location of the defect, type of reconstruction performed, and with or without the use of adjuvant measures, such as anchoring points in the periosteum and/or canthopexies2.
Eyelid reconstruction using grafts should be avoided, since primary and secondary contractions might lead to ectropion. A study carried out by Rubin et al.7 found that 14.2% of the patients developed ectropion when eyelid reconstruction was performed using grafts.
The V-Y flap could represent an alternative to cervicofacial flaps used in the eyelid and malar/palpebral groove reconstructions. This flap requires less detachment and creates less dead space, thus reducing the risk of necrosis or seroma. In addition, it provides a similar tissue in relation to color, thickness, and eyelid texture and can be performed under local anesthesia (with or without sedation)2,6,8.
However, the vertical traction of this flap remains the greatest concern to the point that some authors, such as Lize et al.9 suggest the horizontal advancement of the V-Y flap towards the lower eyelid to avoid the vertical tension on the free margin of the eyelid. Other authors, such as Kesiktas et al.10 and Matsuda et al.11, suggest the combination of two flaps to reconstruct the inner corner of the eyes (nasolabial V-Y and glabellar flaps), since a single nasolabial flap (V-Y) could generate an excessive vertical traction and even a "tent" effect in the concavity of the medial canthal region. However, when performed properly, the V-Y skin flap does not increase the risk of postoperative ectropion but adequately reconstructs the region of the inner corner of the eye2.
Sugg et al.2 conducted a study with 34 patients. Of these, 11 underwent eyelid reconstruction with cervicofacial flaps and 23 with V-Y flaps. Of the patients reconstructed with cervicofacial flaps, 82% developed some type of complication, and among those reconstructed with V-Y flaps, 13% developed complications (p = 0.0002).
No statistically significant difference was observed in relation to the development of ectropion in both groups (two cases were detected in the cervicofacial flap group [18%] and one case in the V-Y flap group [4%]; p = 0.24). However, in the cervicofacial flap group, it was necessary to re-operate three patients due to hematoma, while no cases were re-operated in the V-Y flap group (p = 0.03).
Another study carried out by Austen et al.12 found 16% incidence rate of ectropion in a group of 32 patients reconstructed with cervicofacial flaps. Other authors, such as Doermann et al.13 and Li et al.14, detected 9% and 3% incidence rates of ectropion, respectively, after eyelid reconstruction with the V-Y flap.
Yildirim et al.15 conducted a study on 22 patients who underwent reconstruction of the middle third of the face (infraorbital regions, side of the nose, and inner corner of the eyes) and found one case of mild ectropion and a small necrosis at the distal end of the flap. The authors suggest carrying out a de-epithelialization of the flap's ends to anchor them with a 4-0 Nylon thread to the medial and lateral canthal ligaments to prevent ectropion.
According to Harris & Perez1, anchoring points to the periosteum in flaps carried out in the eyelid and malar region re-form the natural osteocutaneous connections, while minimizing palpebral and canthal dystopias. According to the authors, absorbable threads can be used in patients presenting a moderate risk of distortions as these will protect the eyelid until the tension of the flap will disappear. However, in high-risk patients, unabsorbable threads should be used.
In our series of 29 cases of eyelid or malar/palpebral groove reconstructions, two developed postoperative ectropion (6.9%), which showed no improvement six months after surgery. Cases of ectropion occurred in the patients presenting large defects (affecting the inner corner of the eye as well as the palpebral and malar regions). Both patients were elderly (75 and 81 years old) and presented previous eyelid sagging.
In the first case (Figure 2), the design of the flap was inappropriate. It was wider than necessary and shorter, thus not allowing for a good cranial and medial advancement, which eventually generated medial ectropion. This patient continued to present ectropion six months after surgery, but as he was asymptomatic, he showed a good eyelid occlusion. Thus, because of the advanced age (81 years old), we opted to monitor the patient.
On the other hand, the defect generated in the second case (Figure 3) was the largest of the group and affected the nasal region, inner corner of the eye, lower eyelid, and malar region. Therefore, a long and wide flap, generating a great vertical traction in the lower eyelid and resulting in lateral ectropion, was necessary to cover the defect. Six months after surgery, the patient still presented palpebral malocclusion but was symptomatic. We then opted to correct the ectropion with a tarsal strip under local anesthesia.
We believe that, for patients who are at high-risk of developing ectropion (large defects and previous tarsoligamentary sagging), it is possible to choose canthopexy or canthoplasty for the reconstruction.
Some patients developed mild sclera in the postoperative period, which resolved with the aid of conservative measures. Some patients have not yet completed the six months of postoperative period and are therefore still being monitored.
Four cases required surgical correction of the distal portion or pedicle area, which was still elevated six months after surgery. In these cases, the aim was an aesthetic improvement of the reconstruction (13.8%). These procedures were performed under local anesthesia in the outpatient clinic.
Transfixing points on the nasal mucosa showed to be of great value to better define the nasal wing loop in the postoperative period. These have been performed in all patients, whose incision exceeded this region. Correcting the aesthetic transition between the nasal wing and the malar region was not required in these patients. No patient developed infections during the postoperative period.
On the other hand, the points performed in an "in step" pattern and carried out in all patients showed to be important in aiding the advancement of the flap cranially and in decreasing the tension on its upper margin, thus reducing vertical traction.
In our series, 75.8% of the cases reconstructed with the V-Y skin flap had a tumor in the inner corner of the eyes. We believe that, in this region, the flap seems to do less vertical traction and may be anchored to the periosteum and/or the medial canthal ligament. This minimizes traction and reforms the natural concavity of the region, without the necessity of a second flap.
We did not observe any case of hematoma, seroma, necrosis of the distal portion of the flap, or infection.
Patients' follow-up proved to be the greatest challenge of this study. Some patients after the first postoperative months did not return for outpatient monitoring and others died (for reasons not related to surgery), which is expected due to their age group. Of this group, six patients were followed up for less than six months, thus creating biases in this cohort, since these patients may later develop ectropion or require surgical flap correction.
CONCLUSION
When well indicated, designed, and executed, the V-Y skin flap can provide satisfactory results for the reconstructions of the lower eyelid and malar/palpebral groove. It also appears as a good option for those patients who do not have the clinical conditions necessary to undergo surgery under general anesthesia, since this flap can be rapidly implemented, with small detachment, low rates of complications, and can be performed under local anesthesia, with or without sedation.
ACKNOWLEDGMENTS
To Dr. João Duprat, Dr. Eduard Rene Brechtbul, Dr. Eduardo Bertolli, Dr. Fernando Henrique Sgarbi Parro, and Dr. Luis Philipe Molina Vana
COLLABORATIONS
MC Analyzed and/or interpreted the data; elaborated and designed the study; carried out the surgeries; wrote the manuscript.
REFERENCES
1. Harris GJ, Perez N. Anchored flaps in post-Mohs reconstruction of the lower eyelid, cheek, and lateral canthus: avoiding eyelid distortion. Ophthal Plast Reconstr Surg. 2003;19(1):5-13.
2. Sugg KB, Cederna PS, Brown DL. The V-Y advancement flap is equivalent to the Mustardé flap for ectropion prevention in the reconstruction of moderate-size lid-cheek junction defects. Plast Reconstr Surg. 2013;131(1):28e-36e.
3. National Comprehensive Cancer Network (NCCN). [citado 2015 Jun 6]. Disponível em: https://www.nccn.org/patients/guidelines/melanoma/files/assets/common/downloads/files/melanoma.pdf
4. Esser JFS. Die Rotation der Wange und allgemeine Bemerkungen der chirurgischen Gesichtsplastik. Paris: Vogel; 1918.
5. Mustardé JC. The use of flaps in the orbital region. Plast Reconstr Surg. 1970;45(2):146-50.
6. El Kollali R. Lower eyelid and cheek reconstruction by a temporally extended V-Y cheek flap. J Craniofac Surg. 2013;24(1):e57-9.
7. Rubin P, Mykula R, Griffiths RW. Ectropion following excision of lower eyelid tumours and full thickness skin graft repair. Br J Plast Surg. 2005;58(3):353-60.
8. Kwon KH, Lee DG, Koo SH, Jo MS, Shin H, Seul JH. Usefulness of v-y advancement flap for defects after skin tumor excision. Arch Plast Surg. 2012;39(6):619-25.
9. Lize F, Leyder P, Quilichini J. Le Lambeau d´advancement horizontal en V-Y dans les reconstructions des pertes de substances non transfixiantes de la paupière inférieure chez le sujet jeune. J Fr Ophtalmol. 2015;38(1):7-12.
10. Kesiktas E, Eser C, Gencel E, Aslaner EE. A useful flap combination in wide and complex defect reconstruction of the medial canthal region: Glabellar rotation and nasolabial V-Y advancement flaps. Plast Surg (Oakv). 2015;23(2):113-5.
11. Matsuda H, Takahashi Y, Ichinose A, Miyazaki H, Kakizaki H. Combination of nasolabial v-y advancement flap and glabellar subcutaneous pedicled flap for reconstruction of medial canthal defect. Case Rep Ophthalmol. 2014;5(1):50-3.
12. Austen WG Jr, Parrett BM, Taghinia A, Wolfort SF, Upton J. The subcutaneous cervicofacial flap revisited. Ann Plast Surg. 2009;62(2):149-53.
13. Doermann A, Hauter D, Zook EG, Russell RC. V-Y advancement flaps for tumor excision defects of the eyelids. Ann Plast Surg. 1989;22(5):429-35.
14. Li JH, Xing X, Liu HY, Li P, Xu J. Subcutaneous island pedicle flap: variations and versatility for facial reconstruction. Ann Plast Surg. 2006;57(3):255-9.
15. Yildirim S, Aköz T, Akan Md, Avci G. Nasolabial V-Y advancement for closure of the midface defects. Dermatol Surg. 2001;27(7):656-8.
ACCamargo Cancer Center, São Paulo, SP, Brazil
Institution: ACCamargo Cancer Center, São Paulo, SP, Brazil.
Corresponding author:
Mariane Campagnari
Rua Deputado Laercio Corte, 951, Ap. 61 Bloco Copaibas - Panamby
São Paulo, SP, Brazil Zip Code 05706-290
E-mail: maricampa@hotmail.com / marianecampa@gmail.com
Article received: July 17, 2015.
Article accepted: September 29, 2015.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter