

Articles - Year 2003 - Volume 18 - Issue 3
Microsurgical replantation of avulsed scalp - 7 years of experience
Reimplante Microcirúrgico das Avulsões de Couro Cabeludo - Experiência de 7 anos
ABSTRACT
Scalp avulsion is a devastating physical, fururional, and psychological injury to patients. The emergence of surgery and the first replantation by Miller; in 1976, was a major break through in the management of scalp avulsion that became the treatment of choice, whe never possible. This study aims to present the 7 last years of experience of the Discipline of Plastic Surgery of the Medical School of the University of São Paulo and to compare it with the literature, so as to standardize the carefor the cases here in addressed and thus achieve the bestpossible results. The cases presented consist of 6 female patients with scalp avulsion, their ages ranging between 9 and 29 years. Warm ischemia time ranged between 9 and 25 hours (average 14 hours). Four cases were totally successful, one case was partially successful (40%), and the remaining cases lost the replantation. The current techniques and the structure available in specialized facilities enable the appropriate management of avulsed scalps through microsurgical replantation, thus leading to satisfactoty results that are superior to the previously available options.
Keywords: Surgery; avulsion; replantation; scalp; cranioencephalic trauma
RESUMO
A avulsão de couro cabeludo apresenta-se como lesão devastadora aos pacientes acometidos, tanto na esfera orgânica e funcional quanto na psicológica. O advento da microcirurgia e a realização do primeiro reimplante por Miller, em 1976, revolucionaram o manejo da avulsão de couro cabeludo, tornando-se o tratamento de escolha sempre que possível.
Este estudo visa a apresentação da experiência dos últimos 7 anos da Disciplina de Cirurgia Plástica da Faculdade de Medicina da Universidade de São Paulo e a comparação com os dados da literatura, a fim de padronizar um atendimento para os casos em questão e obter o melhor resultado possível.
A casuística apresentada perfaz 6 pacientes do sexo feminino com avulsão do couro cabeludo e idade variando entre 9 e 29 anos. O tempo de isquemia quente oscilou entre 9 e 25 horas (média de 14 horas). O sucesso foi total em 4 casos, parcial (40%) em 1 caso e ocorreu perda do reimplante no caso restante.
Com as técnicas atuais e a estrutura disponível nos centros especializados, faz-se possível o adequado manejo das avulsões de couro cabeludo através do reimplante microcirúrgico, obtendo-se resultados adequados e superiores às opções oferecidas previamente.
Palavras-chave: Microcirurgia; avulsão; reimplante; couro cabeludo; trauma cranioencefálico
Scalp avulsion is a rare event, albeit with serious consequences due both to the injury mechanism and to its psychological and social consequences.
From the physiopathological standpoint, scalp avulsion is the result of the prehension and oblique traction of hair by rotating or traction machinety, while perpendicular traction of the scalp results only in hair being pulled out. It occurs most frequently in work environments, as a consequence of the non-utilization of appropriate protection, and in women, because they have long hair more often.
The forces involved cause tissues to be torn out, affecting only the scalp or also involving other regions, like the forehead, eyebrows, ears and lower portions of the face, making reconstruction procedures even more difficult.
Regarding the depth of the avulsion, the most common is tearing at the subgaleal level. However in cases of greater traction strength, subperiosteal avulsion may occur, even affecting parts of the cranial vault, and irs association with cranioencephalic traumas is not uncommon(1).
Permanent treatment has undergone major changes after the improvement and standardization of microsurgical replantation techniques. Until the 1970's, usual treatment consisted in covering with skin grafts, which caused permanent alopecia and greater risk of ulceration. In 1976, Miller et al.(2) reported the first successful case of microsurgical replantation, thus encouraging the utilization of the technique, which then became the first choice treatment. Other treatment options were reserved for unsuccessful cases or as ancillary procedures.
Until recently, the world experience with scalp microsurgical replantations was limited to isolated case reports, not more than thirty or forty, or to small study groups; and for that reason it was not possible to standardize the treatment sequence and success rates.
Success depends on factors such as ischemia time, quality of the avulsed portion, experience of the surgeon, and others. The likelihood of failure confronts surgeons with a difficult situation to solve, as there is often no remaining scalp, but rather a large exposed area of the cranial vault to be covered.
In face of this highly complex situation and in view of the need to conduct a general analysis of the results so far obtained by several study groups, the objective of this paper was to analyze the results obtained in recent years by the several groups that have carried out replantations and, combined with the experience of the authors, define success rates and standardize the practice in our setting.
METHODS
The study was conducted retrospectively and comprises a number of consecutive clinical cases of patients with scalp avulsion seen by or referred to the Discipline of Plastic Surgery of the Medical School Hospital of the University of São Paulo,over 7 years, between 1994 and 2001.
The sample presented includes 6 female patients, with ages ranging between 9 and 29 years. Avulsed portions ranged between 70 and 100%. Patients were evaluated in the emergency room, following the ATLS protocol (Advanced Trauma Life Support) in order to identify and treat associated injuries and reach stabilization for surgery.
Avulsed scalps were washed with large amounts of saline solution, stored in sterile plastic bags with Ringer's Lactate and kept in shredded ice.
Procedures were performed by two surgical teams concomitantly, one preparing the receptor area-debridement and identification of vessels - and another preparing the scalp and performing vascular grafts.
As to the surgical replantation technique, initially, enough temporal vessels should be identified to maintain the replantation, and, if necessary, occipital vessels and any other vessels presem in the surgical field.

Fig. 1 - Case # 1. Complete scalp, avulsion.
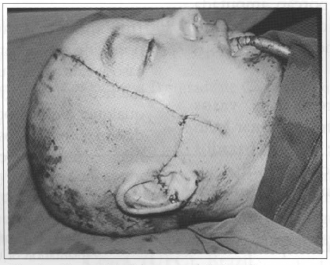
Fig. 2 - Case # 1. Immediate postoperative.
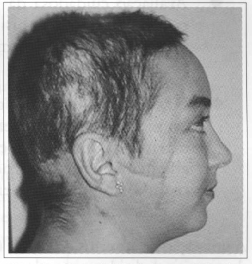
Fig. 3 - Case # 1. Two months postoperative.
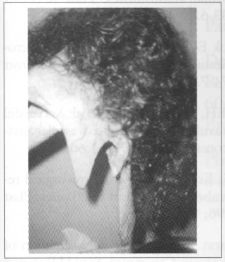
Fig. 4 - Case # 2. Complerely avulsed scalp.
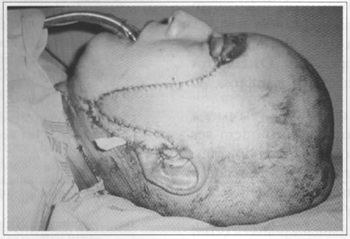
Fig.5 - Case # 2. Immediate postoperative.
Fig. 6 - Case # 2. Four months postoperative.
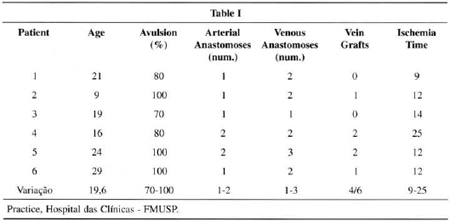
The number of arterial anastomoses varied between one and two, while the number of venous anastomoses varied between one and three, all of them performed with surgical microscope and mononylon 10-0. In four cases, vein grafts were used, varying between zero and two grafts. Warm ischemia time ranged from 9 to 25 hours (average 14 hours) (Table I).
In the postoperative period, patients rested with their heads slightly raised in relation to the trunk, with broad-spectrum int:ravenous antibiotics, for approximately seven days. Seromas and hematomas were promptly emptied, thus avoiding the compression of vascular pedicles. Neither anticoagulants nor vasodilators were used in any of the cases.
RESULTS
Success rates were 100% in four cases, 40% in one case, and total loss of the replantation in one case. In one of the totally successful cases, the patient died due to associated cranioencephalic trauma. Lost areas were treated with partial thickness skin grafts after debridament, leading to alopecia as a seguela.
Then the use of tissue expanders under the re-implanted areas permitted the correction of bald areas by replacing previously grafted areas with pre-expanded flaps.
DISCUSSION
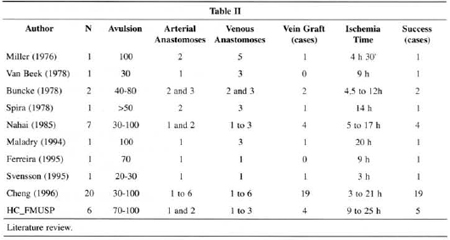
The results obtained with the use of the microsurgical technigue are compatible with those of the international literature (Table II), thus confirming it is the best therapeutic choice to manage scalp avulsion, provided certain principies are observed.
Among the factors that contribute towards a favorable prognosis, the following ones are worth mentioning:
• Adeguate preoperative preparation, with correction of hemorrhagic shock and treatment of life-threatening associated injuries.
• Thorough evaluation of the severed portions, as to the suitability of the tissue (shearing) and of the vessels for replantation.
• Generous debridement of avulsed vessels; they may present extensive injury to the intima and, unless appropriately prepared, the process may lead to thrombosis, even in technically precise anastomoses.
The utilization of vein grafts is important in order to allow the adeguate débridement of the vessels and tension-free anastomosis, in addition to enabling two teams to work simultaneously. Cheng et al.(5) described the use of vein grafts concomitantly in two surgical sites (donor and receptor areas), thus reducing surgical time significantly. Grafts may be removed locally or from limbs.
In special situations, when there are no veins for anastomosis and draining the flap, arterio-venous shunts may be used (from a scalp artery to a vein in the receptor area), and the supraorbital and supratrochlear regions are freguently used for that end. In case number 6, with loss of 60% of the replantation, exactly the opposite was done, with anastomosis of the right temporal artery in a scalp vein with interposed venous graft, as no arterial stump was identified in the avulsed portion, which would be otherwise left without blood supply.
Replantation is potentially indicated in every case due to the benefits it can provide. However, there are a few situations in which its use is counter-indicated, such as in:
1. warm ischemia time above 30 hours;
2. extensive loss of vessels in the flap;
3. excessive laceration or crushing of avulsed tis sues , and
4. inadequate preservation of the latter.
In cases of partial or total loss of the replantation, other surgical procedures are reguired to cover and protect the cranial vault(3,4). One of those options is partial thickness skin grafts (used in two cases of loss in the present study), tissue expansion, and local and distant flaps.
CONCLUSION
Initially based on published literature and, then, with the observation of the results of the treated cases that presented functional, esthetical, and psychological gains undoubtedly superior to any other therapeutic option, major efforts should be made so as to be successful in the microsurgical replantation of avulsed scalps.
REFERENCES
1. Nahai F, Hester TR, Jurkiewicz MJ. Microsurgical replantation of the scalp. J Trauma. 1985; 25:897-902.
2. Miller GD, Austee EJ, Shell JA. Successful of an avulsed scalp by microvascular anastomoses. Plast Reconstr Surg. 1976; 58:133-6.
3. Van Beek AL, Zook EG. Scalp replantation by microsurgical revascularization: Case report. Plast Reconstr Surg. 1978; 61:774-7.
4. Buncke HJ, Rose EH, Brownstein MJ et al. Suecessful replantation of two avulsed scalps by microvascular anastomoses. Plast Reconstr Surg. 1978; 61:666-72.
5. Cheng K, Zhou S, Kecheng J et al. Microsurgical replantation of the avulsed scalp: report of 20 cases. Plast Reconstr Surg. 1996; 97:1099-106.
6. Svensson H, Njalsson T. Microsurgical replantation of partial avulsion of the scalp. Case report. Scand J Reconstr Surg Hand Surg. 1995; 29:177-80.
I - Plastic Surgery Resident of the Discipline of Plastic Surgery of Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo.
II - Consultant of the Discipline of Plastic Surgery of Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo.
III - Full Professor of the Discipline of Plastic Surgery of Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo.
Plastic Surgery Discipline of Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo
Address for correspondence:
Dimas André Milcheski, MD
R. Oscar Freire, 2121 apto. 504
05409-011 - São Paulo - SP Brazil
e-mail: dimasam@brturbo.com


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter