

Special Article - Year 2016 - Volume 31 -
Prophylaxis of fat embolism syndrome: a current analysis
Profilaxia da síndrome de embolia gordurosa: uma análise atual
ABSTRACT
INTRODUCTION: To analyze data from the internet on deaths from fat embolism, time of onset, and other information that could determine current reality in Brazil regarding fat embolism syndrome incidence and any ,media repercussions, and also to review methods of prevention and what are the best methods available to treat this disease.
METHODS: A Google search was conducted from January 2000 to January 2014 using the keywords "plastic surgery" and "death." We included and reviewed articles containing the words "embolism", "fat embolism" and "complications in (or of) plastic surgery".
RESULTS: We included 235 relevant news stories over the 14 included years. There were 45 cases of death related with plastic surgery that offered few data for individualization. Of these patients, 44 were women. Possible causes mentioned were pulmonary embolism (five cases), perforation of viscera (four cases), malignant hyperthermia (three cases), anesthesia (two cases), anaphylactic shock (two cases), fat embolism (one confirmed case), and "other" (five cases).
CONCLUSION: Guidelines to prevent fat embolism in plastic surgery are needed, however, there is also the need of more evidence based studies to understand more clearly what methods are best.
Keywords: Anaphylaxis; Embolism fat; Malignant hyperthermia; Pulmonary embolism; Surgery plastic/mortality; Viscera.
RESUMO
INTRODUÇÃO: Analisar dados da internet relacionados a mortes por embolia gordurosa, inicio da doença, e outras informações podem determinar a realidade atual no Brasil relacionada à incidência da síndrome de embolia gordurosa e qualquer repercussão na mídia, e também revisar as metodologias de prevenção e quais são os melhores métodos disponíveis para tratar a doença.
MÉTODOS: Uma pesquisa no google foi conduzida de Janeiro de 2000 a Janeiro de 2014 utilizando os descritores "cirurgia plástica" e "morte". Foram incluídos e revisados artigos contendo as palavras "embolia", "embolia gordurosa" e "complicações em (ou de) cirurgia plástica".
RESULTADOS: Incluiu-se 235 matérias novas relevantes ao longo dos 14 anos. Houve 45 casos de óbito relacionados com cirurgia plástica que ofereceu poucos dados para individualização. Desses pacientes, 44 eram mulheres. As causas possíveis mencionadas foram embolia pulmonar (cinco casos), perfuração das vísceras (cinco casos), hipertermia maligna (três casos), anestesia (dois casos), choque anafilático (dois casos), embolia gordurosa (um caso confirmado), e "outros" (cinco casos).
CONCLUSÃO: Diretrizes de prevenção para embolia gordurosa em cirurgia plástica são requeridas, porém, há também necessidade de mais estudos baseados em evidência para entender mais claramente quais são os melhores métodos.
Palavras-chave: Anafilaxia; Embolia gordurosa; Hipertermia maligna; Embolia pulmonar; Cirurgia plástica/mortalidade; Visceras.
The word "embolism" derives from the Greek and it means "something throw in". It constitutes a frequent intraoperative and postoperative risk. Fat embolism occurs due to a mechanical blockage of the vascular lumen by circulating fat droplets, mainly as a result of orthopedic fractures in long bones and polytrauma secondary to cosmetic procedures involving lipectomy and fat grafting. Other associated risk factors are burns, soft tissue injury, sepsis, intravenous infusion of lipids, acute pancreatitis, alcoholism and corticosteroid therapy1-3.
The main symptoms involve the respiratory system and the central nervous system being the classic triad: progressive respiratory failure, altered level of consciousness and petechiae (12-72h after the initial event.)2,3.
There are two major theories that explain the pathophysiological evolution of signs and symptoms of fat embolism, but they do not change the treatment plan: a mechanical hypothesis and a biochemical hypothesis. The most accepted theory is the combination of the two theories, with mechanical factor responsible for the genesis of the syndrome.
The mechanical hypothesis holds that intravascular projection of microdroplets of fat through the venous sinusoids as a result of increased intramedullary pressure following fractures and cosmetic procedures. Upon reaching the small pulmonary vessels, primarily, and the systemic vessels, as a result of the patency of the foramen ovale, of pulmonary arteriovenous microfistulas and of the deformation of microdroplets of fat running through the pulmonary capillaries, vascular obstruction occurs with the onset of symptoms.
The biochemical hypothesis is based on the action of an enzyme called lipoprotein lipase, which degrades micro droplets of fat into free fatty acids, increasing the serum content of their toxic byproducts which cause endothelial injury and type II pneumocytes (responsible for producing surfactant). There is, as well, an increased level of chemical mediators such as platelet activating factor, phospholipase A2, cyclic guanosine monophosphate, serotonin, and nitric oxide - among others - responsible for the evolution of the clinical presentation4,5.
Fat embolism (FE) occurs in most patients with long bone fractures and pelvic fractures. The incidence varies, depending on the series, from 67-95% of trauma patients1,2. Still, fat embolism syndrome (FES) occurs in only 1-10% of patients of those who exhibit pulmonary, neurological, cardiac, hematologic, eye and skin signs and symptoms2,3.
The first case of post traumatic FE was reported by Zenker in 1862, but only in 1873 that Bergmann conducted the first clinical diagnosis of a FE case following hip fracture. In 1970, Gurd characterized the clinical findings and defined FES2. Since then, a number of studies have been conducted in orthopedics and plastic surgery area to improve definition and treatment in cases of FES.
Fat grafting procedure is commonly performed after lipectomy, both for aesthetic and reconstructions purposes. However, few reports exist in the literature on FES. During lipectomy and fat grafting, there are ruptured venules and damage to adipocytes, yielding lipid microfragments which reach the venous circulation and, consequently, FE that can also reach the circulation system. A study of lipectomy in an animal model found circulating microparticles of fat and pulmonary lipid deposits in 100% of the sample1.
By presenting a very severe clinical picture, some preventive strategies for FES were described. Regarding plastic surgery, especially lipectomy, initial care should be given to diligent patient selection for proposed procedures. Reduction in surgical time decreases the risk for development of FES, as well as risks for other adverse events, such as thromboembolism. The limited number of procedures in a single area of the body lessens injury to blood vessels, decrease the possibility of lipidmicrofragments to penetrate vessels. Preventive strategies also include administration of intravenous fluids for up to 24 hours after surgery to maintain adequate blood volume and prevent hemoconcentration1,2.
Although lipectomy is widely used, there are few reports in literature on the FES following its procedures. We analyzed data from an internet search related to deaths from FE, time of onset, and other relevant information to determine current reality in Brazil regarding FES incidence and any media repercussions.
METHOD
A Google search was conducted from January 2000 to January 2014 using the keywords "plastic surgery" and "death." Articles including the words "embolism","fat embolism" and "complications in (or of) plastic surgery" were reviewed. We included only manuscripts written in Portuguese and from Brazilian publications. All data reported in the lay reports were collected, such as associated surgeries and date of complications.
RESULTS
The search resulted in 235 relevant news stories over the 14 included years. Among those news stories, there were 45 cases of death related to plastic surgery, but they had minimal data for individualization. Of these patients, 44 were women. Deaths occurred during the surgery and up to three months after surgery. Causes of death varied and were imprecise.
Possible causes mentioned were pulmonary embolism (five cases), perforation of viscera (four cases), malignant hyperthermia (three cases), anesthesia (two cases), anaphylactic shock (two cases), fat embolism (one confirmed case), and "other" (five cases). The term "embolism" was used generically in 24 cases.
Therefore, among the 24 cases of "embolism," which were determined as fat embolism, patients' mean age was 38.1 years, all individuals were female. Symptoms were highly variable, and most frequent causes of death were: dyspnea, chest pain, respiratory failure and cardiac arrest.
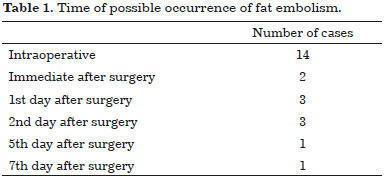
In 13 patients (58.3%) symptoms occurred during surgery. Two patients died immediate in the postoperative period, three in the first postoperative day and other three in the second day after surgery. One patient developed lethal condition on the fifth postoperative day (after a coma during surgery) and another patient on the seventh day - with a clinical presentation of dyspnea and cough on the first day after surgery (Table 1).
Among these 24 cases of death, in only two cases (1 abdominoplasty and 1 breast implant) no lipectomy was performed. In the remaining 24 cases, lipectomy was part of the surgical procedure: in four cases, lipectomy alone; three cases of liposculpture (liposculpture followed by lipo-injection; and in 15 cases, lipectomy combined with other cosmetic procedures.
We observed little consistent data regarding the cases (Table 2), most of them did not have updates in news after the first two weeks following the event.
DISCUSSION
Patients suffering orthopedic trauma comprised the majority of FES cases, and most of studies were done in this area. Post-orthopedic trauma patients, with or without fracture of long bones4 must be followed-up for early diagnosis.
Lipectomy is the second most commonly surgery performed by plastic surgeons in Brazil and in the USA, and currently, the number of lipofilling procedures is also on rise. The combination of lipectomy and lipofilling increases the incidence of fat embolism, and consequently, the risk of FES3.
The onset of symptoms generally occurs within 12-72 hours of the trauma5. In our analysis, approximately 60% of embolisms occured during surgery. Logically there is bias in relation to the patient series used, since many similar cases may not have been reported in press, or had a confirmed diagnoses.
On the other hand, clinical diagnosis is essential (Chart 1 and Table 3), no gold standard exam exist for confirmation of FES. One third of patients present this clinical triad: acute respiratory distress, neurological alterations and petechiae4. FES is generally self-limiting3, and it requires only ventilation support.


Present mortality rate of FES is 7-15%, it tends to fall with the increase of advanced technologies in the ICU2. It is important to be aware that FES occurs in up to 23% of femoral fractures. However, it is often not diagnosed because of the associated traumas (especially chest trauma) which might masquerades respiratory symptoms of FES5.
In order to avoid FES, early stabilization and reduction of fracture of the long bones is essential6. Additionally, the pre-hospitalization use of oxygen therapy has been seen to be effective in reducing the symptoms of FES4. An experimental study with rats has shown that general anesthesia is superior to spinal anesthesia (reduced mortality in the presence of FES), possibly suggesting that general anesthesia should be used in patients with greater risk for FES7.
In an analysis of 30 rats in which the technique of superwet lipectomy was used, and in which animals were divided into three groups - one with anesthesia alone (control), one with lipectomy alone, and one with lipectomy plus fat grafting - there was a 30% higher incidence in deposits of fat cells in the pulmonary capillaries in the liposuctioned group than in the control group, and 60%higher incidence in the group with fat grafting. Although there is no information on how significant this risk is, and if this risk occurs in humans undergoing this type of procedure. That study did not prove that lipectomy can cause embolisms, or show emboli that may or may not cause problems, even when associated with graft fat, in which most cases of fat emboli in the lungs were seen2.
Other analysis assessed the effect of FE in several organs such as lung and liver of 20 New Zealand rabbits submitted to intramuscular autologous fat grafting in the right thigh following lipectomy. The lung and liver tissue were examined post-euthanasia to identify any late injury secondary to a previous FE event in the tissues. The only change observed was the macroscopic sample stains of the liver tissue. There were no microscopic signs consistent with embolic effect. There were no symptoms compatible with repercussions of an embolic process microscopically4.
In a retrospective study of 14 years' experience injecting fat in the gluteal region for aesthetic purposes, in which there was variation in the quantity of fat and region filled over the years, they concluded that when a large quantity of fat is injected in a small area in an attempt to obtain better results, there are more frequent complications. Two patients (0.2%) had FES. In both cases, the quantities of aspirated material and of injected fat were very small, but both had significant dehydration after the surgery8.
Similar cases were described, in which dehydration was present in FES. Dehydration can cause blood concentration, including concentration of fat that was not completely eliminated from the circulatory system following lipectomy and/or lipofilling. Significant fluid ingestion is recommended after surgery. Complications were fewer if the fat was distributed in a more extensive area and in different layers, allowing for better revascularization3.
The extensive mobilization of fat during lipectomy can cause mechanical damage to the adipocytes and neighboring blood vessels, permitting the lipids to reach the bloodstream, and there is an increase in fat embolism associated with lipofilling2.
In an experimental study comparing lipectomy techniques, the dry technique presented an especial high risk for embolism immediate after surgery. The option to perform fat injections using a less traumatic surgical technique (following wet or tumescent lipectomy, and with a reduced number of lipectomy sites) can be considered preventive measures against embolic events3.
In case reports on lipectomy followed by FES there are descriptions, such as: "the surgery took place without intercurrences, with 600 ml of fat removed. General anesthesia lasted two hours, with no significant loss of blood"4. Again, note that even without the stated "risk factors," the risk exists. When combined with other procedures, as evidenced in our analysis, the risk increases, with the increased length of the surgery, and with greater mobilization of complicating factors8-12.
Despite the many professionals affirm that intramuscular lipofilling may cause more injures to vessels, therefore causing a higher incidence of FES, no articles were found comparing subcutaneous and intramuscular lipofilling, or affirming the superiority of one technique over the other. This is an area needing further research7-13.
There is no specific treatment for FES, but there is supportive treatment: ventilation support, hemodynamic support, and the controversial use of corticoids (methylprednisolone)3. Early diagnosis, surgical or nonsurgical recovery of the fracture, and adequate supportive treatment are essential factors for management of FES with low mortality rates10-14.
The use of corticosteroids is described in orthopedic articles on fractures of long bone as an important means of prophylaxis for fat embolism15. Corticoids increase the stability of the cellular/alveolar membrane, reducing the pulmonary inflammatory process, and offer a reduction in the rate of fat embolism events up to 24%. Despite good evidence and recommendations for the use of corticoids, their use still not accepted or routinely adopted in orthopedic services5-16.
CONCLUSION
In summary, the methods for preventing fat embolism in plastic surgery are:
- Superwet or tumescent technique,
- Maintain adequate hydration intra and post-operative,
- Reduce surgical time,
- Avoid multiple procedures at a single time,
- Perform more conservative lipectomy with fewer treated areas,
- Understand that lipofilling increases the risk of FES, and
- What about the use of corticoids prior to lipofilling? A question to be considered...
COLLABORATIONS
RSF Conception and design of the study.
RG Conception and design of the study.
MCCO Final manuscript approval.
IMJ Manuscript writing or content review analysis.
IN Performing surgeries and/or experiments.
PB Performing surgeries and/or experiments.
PB Performing surgeries and/or experiments.
MACL Performing surgeries and/or experiments.
WMI Performing surgeries and/or experiments.
REFERENCES
1. Akhtar S. Fat embolism. Anesthesiol Clin. 2009;27(3):533-50. DOI: http://dx.doi.org/10.1016/j.anclin.2009.07.018
2. Costa AN, Mendes DM, Toufen C, Arrunátegui G, Caruso P, de Carvalho CR. Adult respiratory distress syndrome due to fat embolism in the postoperative period following liposuction and fat grafting. J Bras Pneumol. 2008;34(8):622-5.
3. Mellor A, Soni N. Fat embolism. Anaesthesia. 2001;56(2):145-54. PMID: 11167474 DOI: http://dx.doi.org/10.1046/j.1365-2044.2001.01724.x
4. Eriksson EA, Pellegrini DC, Vanderkolk WE, Minshall CT, Fakhry SM, Cohle SD. Incidence of pulmonary fat embolism at autopsy: an undiagnosed epidemic. J Trauma. 2011;71(2):312-5. DOI: http://dx.doi.org/10.1097/TA.0b013e3182208280
5. Giannoudis PV, Tzioupis C, Pape HC. Fat embolism: the reaming controversy. Injury. 2006;37 Suppl 4:S50-8. DOI: http://dx.doi.org/10.1016/j.injury.2006.08.040
6. Talbot M, Schemitsch EH. Fat embolism syndrome: history, definition, epidemiology. Injury. 2006;37 Suppl 4:S3-7. DOI: http://dx.doi.org/10.1016/j.injury.2006.08.035
7. Habashi NM, Andrews PL, Scalea TM. Therapeutic aspects of fat embolism syndrome. Injury. 2006;37 Suppl 4:S68-73. DOI: http://dx.doi.org/10.1016/j.injury.2006.08.042
8. Franco FF, Tincani AJ, Meirelles LR, Kharmandayan P, Guidi MC. Occurrence of fat embolism after liposuction surgery with or without lipografting: an experimental study. Ann Plast Surg. 2011;67(2):101-5. PMID: 21301303 DOI: http://dx.doi.org/10.1097/SAP.0b013e3181fe32b6
9. Zeidman M, Durand P, Kundu N, Doumit G. Fat embolism after liposuction in Klippel-Trenaunay syndrome. J Craniofac Surg. 2013;24(4):1319-21. DOI: http://dx.doi.org/10.1097/SCS.0b013e3182953a63
10. Taviloglu K, Yanar H. Fat embolism syndrome. Surg Today. 2007;37(1):5-8. PMID: 17186337 DOI: http://dx.doi.org/10.1007/s00595-006-3307-5
11. Panteli M, Lampropoulos A, Giannoudis PV. Fat embolism following pelvic injuries: a subclinical event or an increased risk of mortality? Injury. 2014;45(4):645-6. PMID: 24315483
12. Alho A. Clinical manifestations of fat embolism syndrome. Arch Orthop Trauma Surg. 1978;92(2-3):153-8. DOI: http://dx.doi.org/10.1007/BF00397952
13. Wang AZ, Ma QX, Zhao HJ, Zhou QH, Jiang W, Sun JZ. A comparative study of the mortality rate of rats receiving a half lethal dose of fat intravenously: under general anaesthesia versus under spinal anaesthesia. Injury. 2012;43(3):311-4. DOI: http://dx.doi.org/10.1016/j.injury.2011.08.022
14. Felzemburgh VA, Barbosa RC, Nunes VL, Campos JH. Fat embolism in liposuction and intramuscular grafts in rabbits. Acta Cir Bras. 2012;27(5):289-93. DOI: http://dx.doi.org/10.1590/S0102-86502012000500002
15. Fourme T, Vieillard-Baron A, Loubières Y, Julié C, Page B, Jardin F. Early fat embolism after liposuction. Anesthesiology. 1998;89(3):782-4. DOI: http://dx.doi.org/10.1097/00000542-199809000-00031
16. Filomeno LTB, Carelli CR, Silva NCLF, Barros Filho TEP, Amatuzzi MM. Embolia gordurosa: uma revisão para a prática ortopédica atual. Acta Ortop Bras. 2005;13(4):196-208. DOI: http://dx.doi.org/10.1590/S1413-78522005000400010
1. Hospital das Clínicas, Universidade Federal do Paraná, Curitiba, PR, Brazil
2. Universidade Federal do Paraná, Curitiba, PR, Brazil
3. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
4. Hospital Erasto Gaertner, Curitiba, PR, Brazil
5. Hospital Universitário Cajuru, Curitiba, PR, Brazil
Institution: Hospital das Clínicas, Universidade Federal do Paraná, Curitiba, PR, Brazil.
Corresponding author:
Ivan Maluf Junior
Rua Silva Jardim, 2833
Curitiba, PR, Brazil. Zip Code 80240-040
E-mail: ivanmalufjr@yahoo.com.br
Article received: February 12, 2015.
Article accepted: April 10, 2016.
Conflicts of interest: none.



 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter