

Original Article - Year 2016 - Volume 31 -
Nasal reconstruction: an analysis of a series of cases
Reconstrução nasal: análise de série de casos
ABSTRACT
INTRODUCTION: Nasal reconstruction is challenging because of the central position and role of the nose in the face. Minor defects in this region become obvious. A retrospective analysis of 146 nasal reconstruction surgeries in the Integrated Plastic Surgery Services of the Ipiranga Hospital (SICP-HI) was performed, evaluating the incidence of nasal defects, as well as the main surgical techniques performed in accordance with each nasal region.
METHODS: A retrospective descriptive study through a review of 109 medical records and photograph archives of patients treated in SICP-HI, São Paulo, SP, from January 2011 to June 2014.
RESULTS: A total of 146 surgeries were performed. The mean patient age was 67 years. Regarding the type of malignant tumors found, 104 (73%) were basal cell carcinoma and 3 (2%) were squamous cell carcinoma. The remaining 36 (25%) lesions were benign. The most affected nasal regions were as follows: nasal wing, 55 (38%); the dorsum, 36 (25%); tip, 26 (18%); sidewalls, 12 (8%); unspecified, 7 (5%); total involvement of the nose, 5 (3%); and the columella, 2 (1%). There was a preference for primary closure of the defect. However, if this was infeasible, local flaps were used, in agreement with the literature.
CONCLUSION: The nasal aesthetic subunits can be reconstructed using a variety of surgical techniques. The surgeon should seek an appropriate aesthetic and functional outcome.
Keywords: Nasal surgical procedures; Basal cell carcinoma; Squamous cell carcinoma; Skin cancer; Surgical flaps.
RESUMO
INTRODUÇÃO: A reconstrução nasal é desafiadora devido à posição central e proeminente do nariz na face. Pequenos defeitos nessa região tornam-se óbvios. Análise retrospectiva das 146 cirurgias de reconstrução nasal nos Serviços Integrados de Cirurgia Plástica do Hospital Ipiranga - SICPHI, avaliando a incidência dos defeitos nasais, assim como as principais técnicas cirúrgicas realizadas de acordo com cada região nasal.
MÉTODOS: Estudo descritivo retrospectivo pela revisão de 109 prontuários e arquivos fotográficos, dos pacientes atendidos nos Serviços Integrados de Cirurgia Plástica do Hospital Ipiranga, em São Paulo, SP, no período compreendido entre janeiro de 2011 a junho de 2014.
RESULTADOS: Foram realizadas 146 cirurgias. A faixa etária média foi de 67 anos. Em relação ao tipo de tumores malignos encontrados, 104 (73%) eram carcinoma basocelular e três (2%) carcinoma espinocelular. As 36 (25%) lesões restantes eram de características benignas. As regiões nasais mais acometidas foram: asa nasal, 55 (38%); dorso, 36 (25%); ponta, 26 (18%); lateral, 12 (8%); não especificada, sete (5%); comprometimento total do nariz, cinco (3%); e columela, dois (1%). Observou-se a preferência ao fechamento primário dos defeitos. No caso de impossibilidade do mesmo, realizaram-se retalhos locais, concordando com a literatura.
CONCLUSÃO: As subunidades estéticas nasais podem ser reconstruídas por uma variabilidade de técnicas cirúrgicas. O cirurgião deve buscar um adequado resultado estético e funcional.
Palavras-chave: Procedimentos cirúrgicos nasais; Carcinoma basocelular; Carcinoma de células escamosas; Neoplasias cutâneas; Retalhos cirúrgicos.
The first reports of nasal reconstruction date back to 2000 B.C. in the records of the Edwin Smith Papyrus1. In India, Sushruta described the use of the median forehead flap for total reconstruction of the nose, known to date as the Indian method2.
Sequelae because of lesions caused by syphilis and leprosy stimulated advances in nasal reconstructions during the Renaissance, and at that time, the flap described by Tagliacozzi was introduced (1597). The construction of this flap is based on the use of the inner surface of the upper third of the arm3.
For centuries, several techniques have been proposed, such as the one described by the Englishman Joseph Carpue and the German Carl Ferdinand von Graefe, at the beginning of the 19th century4. For better refinement of the coverage and support of the wings, Gillies, in 1943, and Converse, in 1956, used chondromucosal grafts of the septum and nasolabial flaps to change the skin folds of the frontal flap5.
Burget and Menick introduced the concept of aesthetic nasal subunits, divided into 9 regions: the sidewalls, alar lobules, soft triangles, dorsum, tip, and columella. The incisions had to be located between these. If the defect compromises more than 25-50% of the subunit, it should be completely removed6.
Defects in the tip and nasal septum can cause significant airway obstruction, as can sudden changes in the nasal contour. The surgeon should be able to provide functional and aesthetically refined nasal reconstruction by mastering the local anatomy7.
Nasal reconstruction is challenging due to the central position and role of the nose in the face. Minor defects in this region become obvious8. The skin varies in color, texture, and thickness according to the region, age, sex, and race of individuals. This variety should be taken into account in choosing the best donor area for a particular defect, to attain a better outcome9,10.
Some of the main causes of nasal deformities are skin tumors, especially basal cell and squamous carcinomas11. In 2014, it was estimated that there were approximately 182,000 cases of non-melanoma skin cancer in Brazil12. Other indications would be anomalies, radiodermatitis, trauma, and infections11.
The nose is particularly vulnerable to malignant skin diseases. About 75% of non-melanoma skin cancers occur in the head and neck. Of these, approximately 30% occur in the nose13.
OBJECTIVE
The objective of this study was to perform a retrospective analysis of 146 nasal reconstruction surgeries in the Integrated Plastic Surgery Services of the Ipiranga Hospital (SICP-HI), in São Paulo, SP, Brazil, and evaluate the incidence of nasal defects, as well as the main surgical techniques performed in each nasal region.
METHODS
The study was a retrospective descriptive study reviewing 109 medical records and photograph archives of patients treated at SICP-HI from January 2011 to June 2014. We analyzed data with respect to gender, age, location of the tumor in the nose, surgical margins, and types of reconstruction.
The SICP-HI is a reference service for the control and treatment of skin cancer in the state of São Paulo. The patients come from basic health care units to SICP-HI.
The inclusion criteria were patients with benign or malignant nasal tumors excluding those who underwent nasal reconstruction for other causes. The exclusion criteria were patients whose medical records were not found.
RESULTS
The total number of operated patients was 109, and 146 surgeries were performed. Some patients had more than 1 lesion. The mean age of patients was 67 (range, 26-95) years (Figure 1).
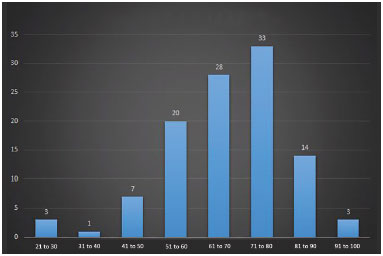
Figure 1. Age range of patients who underwent reconstruction.
The most common complaint of patients who sought the service was aesthetic deformity and concern with the progression of the lesion. Few patients had functional complaints.
The nasal regions most affected were as follows: nasal wing, 55 (38%); dorsum, 36 (25%); tip, 26 (18%); sidewalls, 12 (8%); unspecified, 7 (5%); total involvement of the nose, 5 (3%); and columella, 2 (1%) (Figure 2).
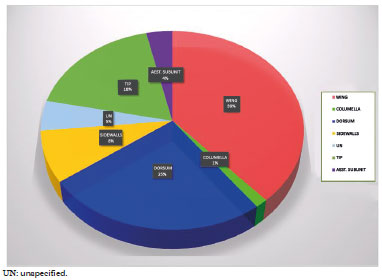
Figure 2. Percentage of involvement of the nasal subunits.
The procedure most often used for the reconstruction of the nasal wing was primary closure in 27 (49%) cases. The most common flap was the nasolabial flap in 11 (20%) cases, followed by the bilobed nasal flap in 4 (7%), and closure by the third intention in 4 (7%). Advanced, rotational, and rhomboid flaps were used in 2 patients each, totaling 4%. Grafts were used in 3 patients (5%) (Figure 3).

Figure 3. Patient who received a bilobed flap for correction of defect due to squamous cell carcinoma in the nasal wing.
In the nasal dorsum, there were 17 (47%) primary closures, 6 (17%) bilobed flaps, 5 (14%) Rintala flaps, 2 (6%) each of glabellar, grafts, and closure by the third intention, and 1 (3%) frontal and nasolabial flap, each (Figure 4).

Figure 4. Patient who underwent reconstruction of nasal deformity with frontal flap.
In the nasal tip, primary closure was performed in 16 (62%) cases, Rintala flap in 5 (19%), bilobed nasal flaps in 3 (12%), and tertiary closure and graft in 1 case each (4%) (Figure 5).

Figure 5. Patient who received a Rintala flap for correction of defect due to squamous cell carcinoma in the nasal tip.
In the sidewalls of the nose, 5 (42%) primary closures were performed, 4 (33%) bilobed nasal flaps, 2 (17%) glabellar, and 1 (8%) rhomboid flap. The 4 cases with lesions affecting the entire nose were reconstructed with a graft of the aesthetic nasal unit.
There were 2 lesions of the columella and primary closure was performed in 100% of the cases.
With regard to the type of malignant tumors found, 104 (73%) were basal cell carcinoma (BCC) and 3 (2%) were squamous cell carcinoma (SCC). The remaining 36 (25%) lesions were benign.
Twenty-two (15%) of the malignant tumors presented compromised surgical margins in the pathological examination.
During the period studied, total nasal reconstruction were performed in 3 cases for non-tumor causes. The causes were congenital malformation, infection after nasogastric intubation in childhood, and leprosy sequel. The forehead (Indian) flap was used, requiring subsequent improvements.
DISCUSSION
Skin tumors are the most common types of cancer. BCC and SCC are the first and second commonest types of cancer, respectively, with the highest incidence and have cure rates of over 90% when treated in the initial phase14, in accordance with that found in the SICP-HI.
In our experience, the topographical distribution of nasal tumor lesions had a higher incidence in the nasal wing, which is not consistent with published data that report a higher incidence in the nasal dorsum11,15.
There was a preference for primary closure of the defect. In cases where this was not possible, local flaps were used, in agreement with the literature4.
In our service, we noticed a reduction in the incidence of cases with a need for total nasal reconstruction over time. We believe that this is due to improvements in preventive medicine, increased accessibility of patients to health services, and treatment optimization of contagious diseases. Another explanation would be the advancement of automobile safety mechanisms, as well as individual protection equipment.
The choice of the best flap was based on the nasal subunits involved. The defects in the upper and middle third were repaired mainly with glabellar, bilobed, and rhomboid (Limberg) flaps. In the lower third (tip and wing), the preference was for reconstruction in one surgical moment with nasolabial flaps, bilobed (Esser), Rintala, and advancement flaps16. The most common flaps used in the SICP-HI on each nasal third are in agreement with the literature.
We also noticed that the recent integration of the pathology service in the Ipiranga Hospital has enabled the use of intraoperative frozen biopsy, providing flaps with greater safety and a decrease in the duration of nasal reconstruction. In only 6 (4%) of the cases, the wounded area was left, and pathology results were awaited for subsequent reconstruction.
When the loss of substance was larger, the association of grafts was required: flaps with composite grafts (auricular and septal cartilage) or even graft in the whole aesthetic unit. Often, more than 2 surgical times were needed.
Among plastic surgeons, the most frequent procedure for the treatment of nasal skin cancer is surgical resection. In our study, the rate of compromised margins was 22 (15%), which is in agreement with the literature, where the rates range from 4% to 18.2%17.
CONCLUSION
In this report, we aimed to show that nasal aesthetic subunits can be reconstructed using a variety of surgical techniques. Each reconstruction will depend on the location and size of the defect, skin characteristics, shape of the patient's nose, familiarity of the surgeons with certain flaps, as well as of their creativity in the planning of the surgery, seeking a suitable aesthetic and functional outcome.
COLLABORATIONS
BBM Analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
FLS Analysis and/or interpretation of data; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
TEB Conception and design of the study; drafting the manuscript or critical review of its contents.
LPW Data analysis and/or interpretation; completion of operations and/or experiments.
RF Final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
JOGF Data analysis and/or interpretation; statistical analysis; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
REFERENCES
1. Cintra HPL, Bouchama A, Holanda T, Jaimovich CA, Pitanguy I. Uso do retalho médio-frontal na reconstrução do nariz. Rev Bras Cir Plást. 2013;28(2):212-7. DOI: http://dx.doi.org/10.1590/S1983-51752013000200007
2. Melega JM. Cirurgia plástica - fundamentos e arte: cirurgia reparadora de cabeça e pescoço. Rio de Janeiro: Medsi; 2002.
3. Converse JM. Corrective and reconstructive surgery of the nose. In: Converse JM, ed. Reconstructive plastic surgery. 2nd ed. Philadelphia: Saunders; 1977.
4. Oliveira Junior FC, Figueiredo JCA, Piva AM. Técnicas de reconstrução cutânea aplicadas às subunidades estéticas nasais. Rev Bras Cir Craniomaxilofac. 2009;12(3):105-8.
5. Rohrich RJ, Barton FE, Hollier L. Nasal reconstruction. In: Aston SJ, Beasley RW, Thorne CHM, eds. Grabb and Smith's plastic surgery. 5th ed. Philadelphia: Lippincott-Raven; 1997. p.513-29.
6. Menick FJ. A 10-year experience in nasal reconstruction with the three-stage forehead flap. Plast Reconstr Surg. 2002;109(6):1839-55. DOI: http://dx.doi.org/10.1097/00006534-200205000-00010
7. Viksraitis S, Maslauskas K, Bagdonas R. Reconstruction of nasal defect with the composite expanded forehead flap. Medicina (Kaunas). 2010;46(1):34-7.
8. Jackson IT. Retalhos locais na reconstrução de cabeça e pescoço. Rio de Janeiro: DiLivros; 2002. p.87-188.
9. Vuyk HD, Watts SJ. Nasal Reconstruction. In: Vuyk HD, ed. Facial Plastic Reconstructive Surgery. London: Hodder; 2005. p.69-86.
10. Baker SR. Nasal lining flaps in contemporary reconstructive rhinoplasty. Facial Plast Surg. 1998;14(2):133-44. PMID: 11816203 DOI: http://dx.doi.org/10.1055/s-2008-1064337
11. Souza Filho MV, Kobig RN, Barros PB, Dibe MJA, Leal PRA. Reconstrução nasal: análise de 253 casos realizados no Instituto Nacional de Câncer. Rev Bras Cancerol. 2002;48(2):239-45.
12. Brasil. Ministério da Saúde. Instituto Nacional de Câncer. Estimativa 2010: incidência do Câncer no Brasil. Rio de Janeiro: INCA; 2009. 98p. [Acesso 2010 fev 22]. Disponível em: www.inca.gov.br/estimativa/2010
13. Wolfswinkel EM, Weathers WM, Cheng D, Thornton JF. Reconstruction of small soft tissue nasal defects. Semin Plast Surg. 2013;27(2):110-6. DOI: http://dx.doi.org/10.1055/s-0033-1351229
14. Scanavini Júnior RC, Martins AS, Tincani AJ, Altemani A. Fatores prognósticos do carcinoma espinocelular cutâneo de cabeça e pescoço. Rev Bras Cir Cabeça Pescoço. 2007;36(4):226-9.
15. Soares VR. Reconstrução de nariz em neoplasias. Rev Bras Med. 1975;32(1):3-9.
16. Burget GC, Menick FJ. Aesthetic reconstruction of the nose. St. Louis: Mosby; 1993.
17. Tan PY, Ek E, Su S, Giorlando F, Dieu T. Incomplete excision of squamous cell carcinoma of the skin: a prospective observational study. Plast Reconstr Surg. 2007;120(4):910-6. DOI: http://dx.doi.org/10.1097/01.prs.0000277655.89728.9f
1. Hospital Ipiranga, São Paulo, SP, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
3. Universidade Federal de São Paulo, São Paulo, SP, Brazil
Institution: Serviços Integrados de Cirurgia Plástica Hospital Ipiranga, São Paulo, SP, Brazil.
Corresponding author:
Beatriz Buzzini Moura
Rua Agostinho Gomes, 1326
Ipiranga - São Paulo- SP Zip Code 04206-000
E-mail: beatrizmoura@hotmail.com
Article received: November 30, 2015.
Article accepted: May 12, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter