

Original Article - Year 2016 - Volume 31 -
Lobuloplasty Torn earlobe repair
Tratamento de fissuras de lóbulo de orelha
ABSTRACT
INTRODUCTION: The use of ear ornaments is a multicultural practice. The lack of objective evaluations published in the national and international literature is surprising considering the high incidence of torn earlobe (TEL) worldwide.
OBJECTIVE: Evaluation of the results of torn earlobe repair with simple marginal excision and closure using a tissue adhesive.
METHODS: This was a prospective study in which TELs (36) were treated by simple excision of epithelialized edges and closure using cyanoacrylate as tissue adhesive.
RESULTS: TELs caused by earrings (91.7%) and trauma (8.3%) were treated. The following issues were found: flatness (14.8%), unsightly scar (13.9%), notching (11.1%), stretched earlobe (7.4%), and dehiscence (5.6%). No cases of necrosis or keloid scars occurred.
CONCLUSIONS: The proposed treatment proved safe and had satisfactory cosmetic results in 92.6% of patients.
Keywords: Pinna; Pinna/abnormalities; Reconstructive surgical procedures; Adhesives; Cyanoacrylates.
RESUMO
INTRODUÇÃO: O uso de ornamentos auriculares é uma prática multicultural. Considerando a grande incidência de fissuras de lóbulo de orelha (FLOs) no mundo inteiro, é surpreendente a escassez de avaliações objetivas na literatura nacional e internacional.
OBJETIVO: Avaliação dos resultados do fechamento de FLO's por meio de simples remoção de suas bordas e fechamento usando adesivo tissular.
MÉTODOS: Estudo prospectivo no qual FLOs (36) foram tratadas por simples excisão de suas bordas epitelizadas e fechamento usando cianoacrilato como adesivo tissular.
RESULTADOS: Foram tratadas FLOs causadas por brincos (91,7%) e por trauma (8,3%). Achatamento (14,8%), cicatriz inestética (13,9%), entalhe (11,1%), alongamento lobular (7,4%) e deiscência (5,6%) foram os problemas encontrados. Não houve casos de necrose ou queloides.
CONCLUSÕES: O tratamento proposto mostrou-se seguro e com resultados cosméticos satisfatórios em 92,6% das pacientes.
Palavras-chave: Pavilhão auricular; Pavilhão auricular/anormalidades; Procedimentos cirúrgicos reconstrutivos; Adesivos; Cianoacrilatos.
The use of ear ornaments by both sexes is an ancient practice in cultures worldwide. Surgical treatment of torn earlobes (TEL) resulting from ear piercing has been described from Babylon and Persia, through ancient India (100 BC to 100 AD), to Victorian England. Stretched earlobe resulting from TEL closure was termed kákusthapáli by Sushruta Samnhita over two millennia ago (606 BC)1,2.
The lack of objective evaluations published in the literature is surprising, considering the high incidence of TEL worldwide. Most available studies report small case series without replicable bases1-11. Furthermore, few attempts are made to identify etiological factors2.
OBJECTIVE
The present study aimed to assess the results of lobuloplasty through simple freshening of the cleft edges and use of tissue adhesive (cyanoacrylate).
METHODS
Prospective study performed from January 1, 2005 to August 1, 2010.
All patients with TEL seeking surgical correction of their injuries were included in the study. Patients with injured lobes with signs of inflammation, including local infections and dermatitis, and patients with keloid scars or a history of allergy to tissue adhesive components, were excluded from the study.
The present study was performed in accordance with the 1964 Declaration of Helsinki criteria and its subsequent amendments. Patients (or their legal guardians) gave signed informed consent after being informed about the objectives, methods, risks, and benefits associated with the use of anesthesia, incisions, sutures, and tissue adhesives.
Surgical technique
Lobuloplasty was performed according to the following steps (Figure 1):
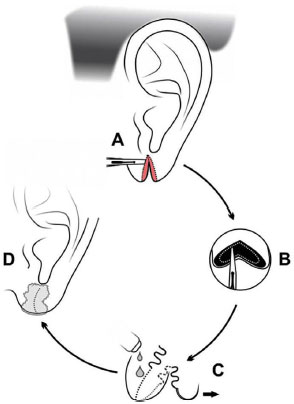
Figure 1. Surgical technique; A: Excision of cleft edges; B: Displacement of the skin edge; C: Intradermal suturing and start of adhesive bonding; D: Adhesive-bonded earlobe and exposed dressing.
• ear antisepsis with a solution of 0.5% chlorhexidine in alcohol and placement of sterile surgical fields around the wound;
• infiltration of cleft edges with 2 to 4 ml of 1% lidocaine with adrenalin 1:100.0001,3 and 10-minute wait for a vasoconstrictor effect;
• resection of the cleft edges: using a No. 11 scalpel, wedge excision of complete cleft edges and circular excision of incomplete cleft edges; excision of acute traumatic clefts (3) with open wound edges was obviously unnecessary;
• 1-mm displacement of the wound edges;
• intradermal suture with 5-0 monofilament nylon1,3
• sealing of the sutured edges with cyanoacrylate adhesive;
• removal of intradermal sutures;
• dressing exposure.
Digital photographs were taken immediately prior to surgery, 30 and 90 days after the procedures, and at any time complications appeared, for surgical documentation.
The author observed the earlobes for symmetry, volume reduction, bottom edge alignment, and presence of unsightly scars at the 3-month evaluation. At this time, patients were asked whether they were satisfied with the outcome, rating the results from the surgery as satisfactory or unsatisfactory.
RESULTS
The study population characteristics and technical details of the surgical procedure are shown in Table 1. Figures 2 to 9 shows the results assessed, incidence of complications, illustrative cases, and cosmetic results.
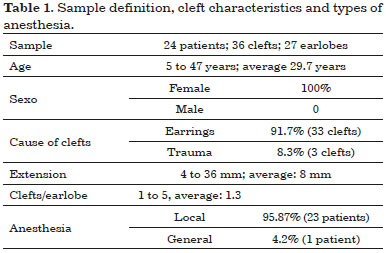
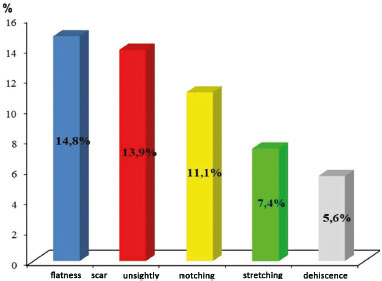
Figure 2. Complications.

Figure 3. Traumatic left earlobe cleft in a 5-year-old child; A: Preoperative; B: Postoperative after bonding with tissue adhesive.
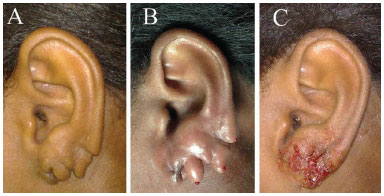
Figure 4. Triple earlobe cleft in a 27-year-old patient; A: Preoperative; B: After anesthetic infiltration; C: After bonding with tissue adhesive.
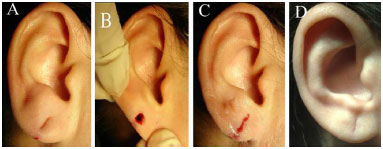
Figure 5. Incomplete earlobe cleft in a 35-year-old patient; A: After anesthetic infiltration; B: Excision of cleft edges; C: After adhesive bonding; D: Complication: depressed scar (POD 90).

Figure 6. Notching in a 33-year-old patient (POD 90); A: Preoperative; B: Postoperative: suture correction.

Figure 7. Dehiscence (posterior) in a 32-year-old patient (POD 7); A: Preoperative; B: Resulting hypertrophic Scar (POD 90).
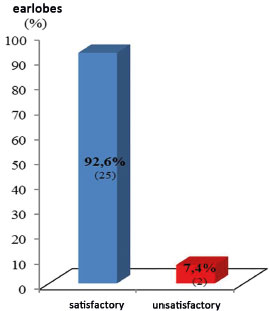
Figure 8. Aesthetic results.
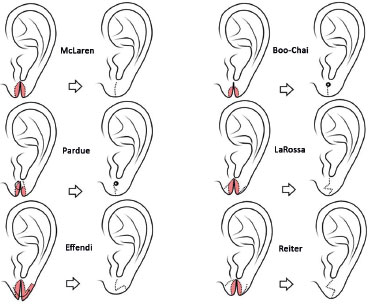
Figure 9. Surgical techniques.
DISCUSSION AND CONCLUSION
Ear piercing may result in early and late complications, despite being a low-risk procedure. The most serious complications include infections, keloid scarring, tissue avulsion, and TEL3.
TEL may be congenital, ischemic (compression by pressure earrings), cosmetic (erosion by pierced earrings), or traumatic. The relative incidence of each cause has not been reported2. The present study shows that cosmetic injuries are the most common cause of TEL (94.4%), thus confirming the standard clinical practice2,6.
Currently, TEL is the most common earlobe deformity, and is primarily caused by traction from heavy piercing earrings. The defect may be unilateral or bilateral, complete or incomplete, depending on the presence or absence of an intact skin edge on the periphery of the earlobe. Complete clefts often result from a small force applied to the earring placed in an incomplete cleft, which was previously extended. Less commonly, the cleft results from a strong, sudden traction on the earring. However, most patients ignore such trauma3-5.
There are numerous lobuloplasty methods (Figure 9)1,5,7. McLaren8 first approached the subject in a four-case report. He addressed the problem by simple linear suturing after freshening of the cleft edges and scar excision under general anesthesia2. Boo-Chai6 reported congenital and acquired clefts, and designated congenital clefts as "coloboma lobuli." In contrast to McLaren, Boo-Chai performed outpatient surgeries with local anesthesia. The technique consisted of excising the cleft edges, only leaving epithelium in the apex, wherein a rod was placed. Then, the cleft was closed linearly below the rod to redo the hole; 3 weeks later, the rod was replaced with an earring2,5,6,9.
Pardue10, when treating patients seeking to continue using earrings, modified the Boo-Chai technique by using a small skin flap from one side of the cleft near the apex, which was looped to form the floor of the epithelialized canal around a nylon thread, suturing the open wound edges. The earring was only used for 6 weeks after the surgery to maintain the sutures2.
Hamilton and LaRossa11 published the first study with objective data collected from repairing acquired earlobe clefts in 14 women. They performed linear closure with Z-plasty at the bottom edge of the earlobe2,5,9. Effendi9 reports a cleft reconstruction method that also corrects stretched and thin earlobes due to prolonged use of heavy earrings. The technique is an L-plasty, which begins with deepithelialization of the cleft edges. The posterior edge is further deepithelialized backwards until it is fitted into the end of the anterior flap. After suturing, the elongated earlobe is shortened in the vertical direction and lengthened in the horizontal direction. The earlobe is repierced after 90 days2. Reiter & Alford2 reported a series of 64 patients treated with full-thickness Z-plasty throughout the complete cleft in a comprehensive review on TEL.
Various Z-plasty techniques or small repairs have been reported for TEL correction since the publication of those seminal studies4. No useful purpose is served by repeating these data. Therefore, the references used in the present study are purposely limited and are summarized in Figure 9.
TEL repair has been influenced by the study of small case series and misadventures. The Boo-Chai technique leaves a large hole, which tends to become infected. Furthermore, the small rod left at the apex of the suture creates a very high earlobe hole. The Pardue technique is even more complex and was designed to avoid cleft recurrences. The Pardue flap fixes the position of the hole and gives it a firm bottom edge, also producing a large hole. Given these drawbacks, some authors advise against maintaining the earring hole2. The Effendi technique causes a trapdoor deformity both vertically and horizontally, which may leave a notch at the bottom edge of the earlobe2.
The technique used by the author (McLaren technique) is simpler than the Pardue technique and more advantageous than the Boo-Chai excision, enabling placement of a new hole anywhere in the earlobe. However, the technique precludes the immediate use of earrings3.
In the present study, no earlobe was repierced. However, when this is requested, the earlobe should be pierced when soft, without notches or linear white scars (thickness < 1 mm), and always after 90 postoperative days (POD)3. The McLaren technique allows symmetric placement of holes and anywhere in the ear lobe.
Repiercing anywhere along the repair line is unjustifiable considering the increased risk of cleft recurrence2 because the scar has reduced tensile strength12,13. The rate of TEL recurrence in repierced earlobes has been reported to range from 0 to 14.7%2,3,6,9. The technique used in the present case series provides time for the wound to heal; thus, in case of earlobe repiercing along the scar, the new hole becomes more stable and less prone to stretching and laceration3.
The overall rate of complications observed in the present study was 33.3% for repaired earlobes (9 of 27 earlobes) and 13.9% for the resulting scars (5 of 36 scars). Flattened earlobes (14.8%; 4) resulted from the inevitable removal of epithelialized edges of clefts along with a small flap of surrounding tissue. Notching occurred in 11.1% of cases (3) that were treated with new excision and simple suturing, without using cyanoacrylate; all cases resolved (Figure 6).
Notching and earlobe flatness are common complications when using wedge excision with linear repair, even if the result of surgery is considered satisfactory4,7. In other studies, the occurrence rates of flatness and notching have been 22% and 5.8%, respectively; these rates are slightly higher than observed herein2,3.
After reconstructing the earlobe, most authors performed Z-plasty at the earlobe edge to prevent notching2,5. However, Z-plasty requires precise incisions and angles, increases the scar size, and is difficult to perform where there is lack of tissue, as occurs in the cleft earlobe2,7.
In the present study, 7.4% (2) repaired earlobes became stretched. This problem has been reported in 0 to 1.5% of cases2,3. The repair of incomplete earlobe clefts by edge deepithelialization and direct suturing may result in abnormal earlobes, either pointed or downward elongated1.
The methods of Boo-Chai, Pardue, and Hamilton and LaRossa are satisfactory for earlobe clefts with adequate volume. However, if any of these methods is used to reconstruct small earlobes, they will become thin and stretched. Furthermore, if the patient continues to wear heavy earrings, the cleft will reoccur9.
In the present study, the incidence of hypertrophic scars (height > 1 mm) was 5.6% (2 of 36 scars), 5.6% for depressed scars (depth > 1 mm), and 2.8% (1) for enlarged scars (width > 1 mm). No patient perceived such scars as unaesthetic or requested treatment. Hypertrophic scars resulted from earlobe dehiscence; other cases of unsightly scars were attributed to individual predisposition because they occurred spontaneously, with no detectable relationship to complications. The incidence of unsightly scars in the treatment of TEL has not been reported by other authors1-11.
The advantages of cyanoacrylates include the bactericidal effect, avoiding the use of dressings, cost-effectiveness, absence of suture marks, safety, ease, and speed of use. Therefore, use of cyanoacrylate glue is currently the skin closure method that pleases most users14-16.
In the present case series, there were 2 complications of dehiscence related to using tissue adhesive (5.6%), resulting from the inadvertent early removal of the adhesive film by the patients, leading to partial opening of the wound and hypertrophic scarring (Figure 7).
Dehiscence has been considered the most common complication from the use of cyanoacrylates (0.3% to 26%), and primarily occurs in wounds located in taut skin areas. The use of cyanoacrylates is particularly indicated for small, linear, low-tension repairs, including TEL closure, because the adhesive only provides a tensile strength similar to that of a 5-0 nylon suture14,15.
In our country, the main obstacle to the use of tissue adhesives is the high cost15,16. However, the method reported herein is cost-effective because it requires the use of only one tube of cyanoacrylate, which increases the cost of the procedure by $ 25.00.
The assessment of cosmetic results showed a satisfactory rate (92.6%; 25), similar to that reported in the literature (91%; 100%)1-3,5,7,9,17. These good results were attributed to the reduced extent of surgery, simplicity of the technique, and reduced rate of complications perceived by patients.
CONCLUSIONS
The use of simple excision and direct closure using cyanoacrylate for TEL proved safe, and had satisfactory cosmetic results (92.5%) in this group of patients.
ACKNOWLEDGEMENTS
I thank Dr. José Humberto Oliveira Campos for the technical revision of the present study.
COLLABORATIONS
SCS Data analysis and/or interpretation; statistical analysis; final manuscript approval; study design; conducting operations and/or experiments; manuscript writing or content review analysis.
REFERENCES
1. Hochberg J, Ardenghy M. Repair of incomplete cleft earlobe. Ann Plast Surg. 1996;37(2):170-2. DOI: http://dx.doi.org/10.1097/00000637-199608000-00009
2. Reiter D, Alford EL. Torn earlobe: a new approach to management with a review of 68 cases. Ann Otol Rhinol Laryngol. 1994;103(11):879-84. PMID: 7979002 DOI: http://dx.doi.org/10.1177/000348949410301109
3. Apesos J, Kane M. Treatment of traumatic earlobe clefts. Aesthetic Plast Surg. 1993;17(3):253-5. DOI: http://dx.doi.org/10.1007/BF00636271
4. Clevens RA, Baker SR. Plastic and reconstructive surgery of the earlobe. Facial Plast Surg. 1995;11(4):301-9. DOI: http://dx.doi.org/10.1055/s-2008-1064546
5. Elsahy NI. Reconstruction of the cleft earlobe with preservation of the perforation for an earring. Plast Reconstr Surg. 1986;77(2):322-4. PMID: 3511485 DOI: http://dx.doi.org/10.1097/00006534-198602000-00031
6. Boo-Chai K. The cleft ear lobe. Plast Reconstr Surg Transplant Bull. 1961;28:681-8. PMID: 13871122 DOI: http://dx.doi.org/10.1097/00006534-196112000-00007
7. Kalimuthu R, Larson BJ, Lewis N. Earlobe repair: a new technique. Plast Reconstr Surg. 1984;74(2):299-300. PMID: 6463154 DOI: http://dx.doi.org/10.1097/00006534-198408000-00025
8. McLaren LR. Cleft ear lobes: a hazard of wearing ear-rings. Br J Plast Surg. 1954;7(2):162-5. DOI: http://dx.doi.org/10.1016/S0007-1226(54)80019-1
9. Effendi SH. Reconstruction of the middle-aged torn earlobe: a new method. Br J Plast Surg. 1988;41(2):174-6. DOI: http://dx.doi.org/10.1016/0007-1226(88)90047-1
10. Pardue AM. Repair of torn earlobe with preservation of the perforation for an earring. Plast Reconstr Surg. 1973;51(4):472-3. PMID: 4689697 DOI: http://dx.doi.org/10.1097/00006534197304000-00031
11. Hamilton R, LaRossa D. Method for repair of cleft earlobes. Plast Reconstr Surg. 1975;55(1):99-101. PMID: 1114186 DOI: http://dx.doi.org/10.1097/00006534-197501000-00021
12. Weinzweig J. Plastic surgery secret plus. 2nd ed. Philadelphia: Mosby Elsevier; 2010.
13. Thorne C, Grabb WC, Smith JW. Grabb and Smith's Plastic Surgery. 6th ed. Philadelphia: Lippincott-Ravens Publishers; 2007.
14. Singer AJ, Thode HC Jr. A review of the literature on octylcyanoacrylate tissue adhesive. Am J Surg. 2004;187(2):238-48. PMID: 14769312 DOI: http://dx.doi.org/10.1016/j.amjsurg.2003.11.017
15. Souza S, Brigia CH. Estudo comparativo entre etilcianoacrilato e sutura intradérmica no fechamento de excisões cutâneas. Rev Bras Cir Plast. 2011;26(4):566-72.
16. Souza SC, Oliveira WL, Soares DF, Briglia CH, Athanázio PR, Cerqueira MD, et al. Comparative study of suture and Cyanoacrylates in skin closure of rats. Acta Cir Bras. 2007;22(4):309-16. DOI: http://dx.doi.org/10.1590/S0102-86502007000400013
17. Ferreira MC. Cirurgia plástica estética: avaliação de resultados. Rev Soc Bras Cir Plást. 2000;15(1):61-6.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Geral de Camaçari, Camaçari, BA, Brazil
3. Hospital Geral do Estado, Salvador, BA, Brazil
Institution: Secretaria de Saúde do Estado da Bahia, Salvador, BA, Brazil.
Corresponding author:
Sandro Cilindro de Souza
Rua Conselheiro Correa de Menezes, 182 - Horto Florestal
Salvador, BA, Brazil Zip Code 40295-030
E-mail: sandrocilin@gmail.com
Article received: September 12, 2015.
Article accepted: May 12, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter